What is a Qualified Health Provider (QHP)?
A Qualified Health Professional (QHP) is a licensed or credentialed clinician authorized to provide or oversee certain healthcare services, often as defined by federal, state, or payer-specific guidelines. The term is commonly used in medical billing, care coordination, and regulatory compliance — especially in the context of value-based care programs like Chronic Care Management (CCM) and Principal Care Management (PCM).
QHPs typically include physicians, nurse practitioners, physician assistants, and other licensed practitioners such as clinical psychologists or social workers, depending on the service and setting. While “QHP” can also refer to Qualified Health Plans under the Affordable Care Act, in care delivery and billing, it refers to the qualified provider role, not an insurance product.
Key Components of a Qualified Health Professional
-
Holds a valid license or credential recognized by state or federal authorities
-
Authorized to diagnose, treat, and/or supervise care within their scope of practice
-
Meets CMS or payer-defined criteria for services like CCM, PCM, TCM, or CoCM
-
May include physicians, NPs, PAs, psychologists, LCSWs, and others depending on service
-
Plays a central role in billing, documentation, and clinical oversight
-
Often cited in EMR workflows, billing requirements, and compliance policies

The Role of a QHP in Care Delivery
Qualified Health Professionals (QHPs) play a central role in initiating, delivering, and overseeing care across a wide range of outpatient and value-based programs. Depending on the service, a QHP may work independently or as part of a team — and is often the one who meets the credentialing requirements to bill or supervise billable services under Medicare or commercial payer rules.
In practice, a QHP might:
-
Conduct patient assessments and develop care plans
-
Oversee care coordination for Chronic Care Management (CCM), Principal Care Management (PCM), or Transitional Care Management (TCM)
-
Supervise other clinical team members such as RNs or care coordinators
-
Sign off on documentation and fulfill billing attestation requirements
-
Provide direct patient care within their licensed scope
-
Participate in compliance reviews and quality reporting
Because QHP status is defined differently depending on the payer and program, organizations often reference CMS guidance or state-specific rules to determine whether a provider qualifies.
Who Qualifies as a QHP?
There’s no single, universal definition of a Qualified Health Professional (QHP) — instead, eligibility depends on the care setting, the payer (e.g., Medicare or Medicaid), and the specific program or service being billed.
Common QHP Types
Most payers and regulatory bodies consider the following licensed roles to be QHPs:
-
Physicians (MD/DO)
-
Nurse Practitioners (NP)
-
Physician Assistants (PA)
-
Clinical Psychologists
-
Licensed Clinical Social Workers (LCSW)
-
Other advanced or licensed clinicians, depending on state scope of practice and program rules
Credentialing Requirements
To be recognized as a QHP, the provider must typically:
-
Hold a valid license to practice in their state
-
Be enrolled as a Medicare or Medicaid provider (if billing federally funded programs)
-
Be listed on the practice’s credentialing roster for payer contracts
-
Maintain any program-specific training or documentation required (e.g., CoCM workflows, risk assessments)
In some cases, state Medicaid agencies or commercial payers may extend QHP status to other licensed professionals such as RNs, clinical pharmacists, or care managers — especially if working under supervision.
Billing and Reimbursement Involving QHPs
The term Qualified Health Professional (QHP) is commonly used in CMS guidance and payer policies to indicate who is authorized to bill for — or supervise billing of — certain healthcare services. In many cases, QHP status is the key determinant for care management billing eligibility.
When QHP Status Matters
To bill for or supervise services like CCM or PCM, a QHP must:
-
Personally provide the service
-
Or supervise non-QHP clinical staff, such as RNs or care coordinators
-
Meet all documentation and attestation requirements
-
Be recognized as a billing provider by Medicare or the relevant payer
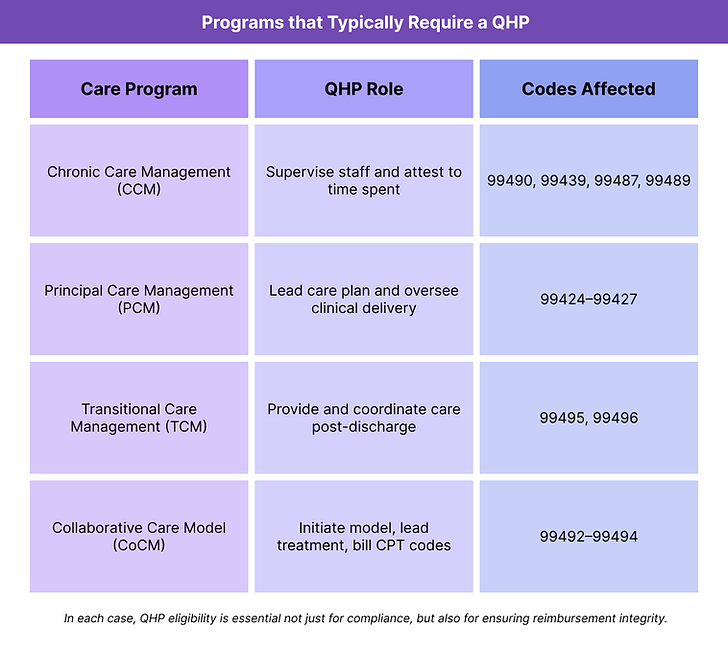
In CoCM (Collaborative Care Model) billing, for example, only a QHP (usually a PCP or NP) may report CPT codes 99492–99494, even though other team members deliver portions of care.
Frequently Asked Questions about QHPs
1. What is a QHP?
A Qualified Health Professional (QHP) is a licensed or credentialed clinician who is authorized to provide or supervise certain healthcare services. The term is commonly used in medical billing, care coordination, and compliance documentation to indicate which providers meet payer or regulatory requirements.
2. Is a QHP the same as a Qualified Health Plan?
No. While “QHP” can also refer to Qualified Health Plans under the Affordable Care Act, in clinical and billing contexts, it refers to a Qualified Health Professional — a person, not a product. The glossary definition on this page focuses on the provider role.
3. Who qualifies as a QHP in Medicare care management programs?
In most cases, QHPs include:
-
Physicians (MD, DO)
-
Nurse Practitioners (NP)
-
Physician Assistants (PA)
-
Clinical Psychologists
-
Licensed Clinical Social Workers (LCSW)
Some payers may recognize other licensed professionals depending on scope of practice and state laws.
4. Why does QHP status matter for billing?
QHP status is required to:
-
Bill directly for certain services
-
Supervise clinical staff providing time-based or care management services
-
Attest to compliance in CMS programs like CCM, PCM, and CoCM
Without a QHP, many of these services cannot be billed or reimbursed.
5. What’s the difference between a QHP and a non-qualified clinical staff member?
A QHP is licensed to make clinical decisions, diagnose, and bill for services. Non-qualified staff (like RNs or MAs) can provide support but must be supervised by a QHP for services to be billable.
6. Can a Registered Nurse (RN) be a QHP?
It depends on the program and the state. RNs are generally not considered QHPs for billing purposes under Medicare but may qualify in certain Medicaid programs or under supervision when documentation requirements are met.

