What is Promoting Interoperability (PI)?
Promoting Interoperability (PI) is a federal program created by the Centers for Medicare & Medicaid Services (CMS) to encourage the secure, efficient exchange of patient health information through certified electronic health record (EHR) technology.
The program focuses on helping providers improve data sharing, enhance patient access to their health records, and support better care coordination across the healthcare ecosystem. PI replaced the earlier Meaningful Use program and is now a core component of the CMS Quality Payment Program (QPP), which also includes MIPS and Alternative Payment Models (APMs).
By participating in PI and meeting program objectives, eligible clinicians can avoid payment penalties and, in some cases, qualify for positive payment adjustments tied to Medicare Part B reimbursements.
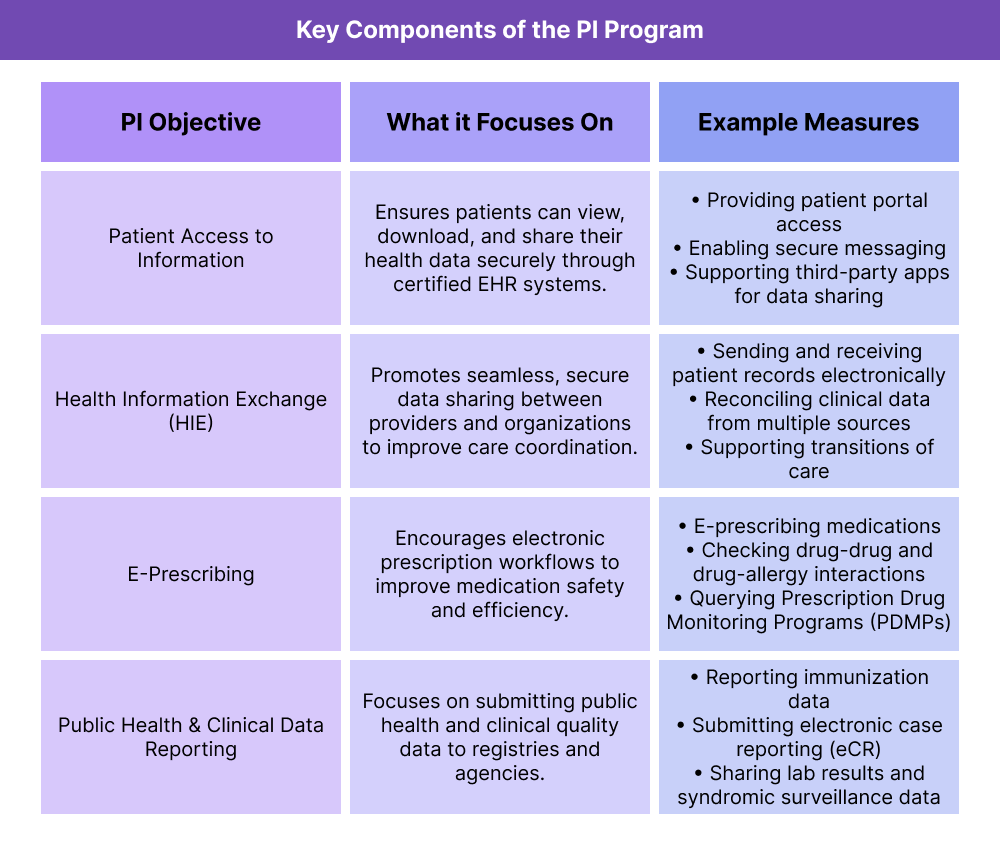
Key Components of Promoting Interoperability (PI)
The Promoting Interoperability (PI) program evaluates provider performance based on four core objectives, each designed to improve data exchange, patient engagement, and care coordination. Within each objective, CMS defines specific measures that eligible clinicians must report on to meet compliance requirements.
1. Patient Access to Information
Enables patients to view, download, and share their health data securely through certified EHR technology.
Measures Include:
- Providing patients with online access to their health information
- Offering secure messaging and patient portals
- Supporting third-party apps that allow data sharing
2. Health Information Exchange (HIE)
Focuses on seamless, secure data sharing between providers and organizations to improve coordination of care.
Measures Include:
- Sending and receiving patient records electronically
- Reconciling clinical data from multiple sources
- Supporting transitions of care between providers
3. E-Prescribing
Encourages providers to use certified EHR systems to send prescriptions electronically and track medication-related information.
Measures Include:
- E-prescribing medications
- Checking for drug-drug and drug-allergy interactions
- Querying state Prescription Drug Monitoring Programs (PDMPs)
4. Public Health and Clinical Data Reporting
Promotes reporting public health data and clinical quality information to appropriate registries and agencies.
Measures Include:
- Submitting immunization data to state registries
- Sharing electronic case reporting (eCR) data
- Reporting syndromic surveillance and electronic lab results
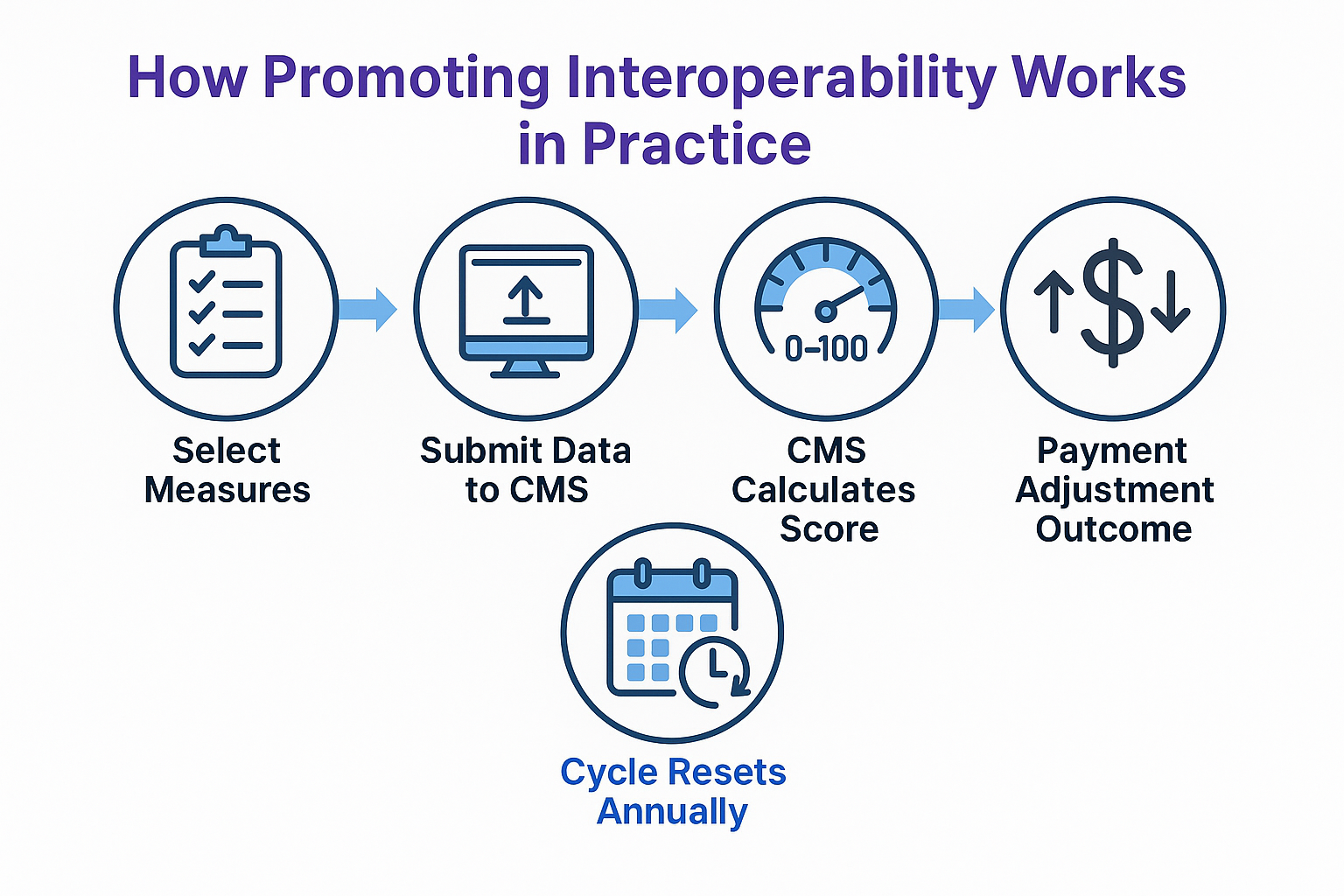
How Promoting Interoperability (PI) Works in Practice
Promoting Interoperability (PI) operates on an annual reporting cycle. Eligible clinicians must use certified electronic health record (EHR) technology to report specific objectives and measures. CMS then evaluates the submissions and assigns a score, which determines whether providers meet program requirements and avoid penalties.
Step 1 — Select and Report Measures
Providers choose measures within the four PI objectives — Patient Access, Health Information Exchange, E-Prescribing, and Public Health Reporting.
- Data is submitted through the CMS Quality Payment Program (QPP) portal or certified registries.
- Each measure requires a numerator and denominator, an attestation, or a “yes/no” response depending on the objective.
Step 2 — CMS Scoring
CMS calculates a Promoting Interoperability score by evaluating performance across the required measures.
- Scores are reported on a 0–100 point scale.
- To avoid penalties, providers must reach the performance threshold set for that program year.
- Scoring emphasizes not just data submission but actual use of EHR functionality.
Step 3 — Compliance and Penalties
If providers successfully meet PI requirements:
- They avoid negative payment adjustments under Medicare Part B.
- Their performance may also contribute to a higher MIPS composite score, depending on participation track.
Clinicians who fail to report PI measures (without an approved exemption) automatically receive the maximum negative adjustment for that year’s program.
Step 4 — Annual Updates
CMS regularly updates the objectives, measures, and thresholds for PI. Providers must confirm the latest requirements each year to remain compliant.
Promoting Interoperability (PI) and its Impact on Billing & Reimbursement
Promoting Interoperability (PI) participation is directly tied to Medicare Part B reimbursements. Providers who successfully meet PI program requirements avoid penalties and may help boost their overall performance scores under the Merit-based Incentive Payment System (MIPS).
How PI Impacts Payments
- Part of the MIPS Composite Score
PI is one of the weighted categories within MIPS. Performance in this category contributes to the final composite score that determines whether a provider earns a bonus, neutral adjustment, or penalty on Medicare reimbursements. - Penalties for Non-Participation
Clinicians required to participate in PI who fail to report measures (without a valid exemption) automatically receive a zero score in the PI category. This can significantly lower the overall MIPS score and result in a negative payment adjustment. - Indirect Financial Benefits
Strong PI performance supports broader goals like interoperability, patient safety, and quality reporting, which can improve outcomes in other value-based programs and reduce costly administrative errors.
Annual PI Adjustments
Because CMS updates thresholds and scoring rules every year, PI requirements — and their impact on reimbursement — change over time. Providers must stay current to ensure compliance and protect revenue.
Frequently Asked Questions about Promoting Interoperability (PI)
1. What is the Promoting Interoperability program?
Promoting Interoperability (PI) is a CMS program that requires providers to use certified electronic health record (EHR) technology to improve data sharing, patient access, and care coordination. It replaced the earlier Meaningful Use program and is part of the Quality Payment Program (QPP).
2. Who is required to participate in PI?
PI generally applies to eligible clinicians and hospitals who participate in Medicare. Most clinicians in the MIPS track of QPP must report PI measures unless they qualify for an exemption. Exemptions are available for reasons such as low patient volume, lack of control over EHR technology, or hardship situations recognized by CMS.
3. What measures are included in PI?
The PI program is organized around four main objectives:
- Patient Access to Information
- Health Information Exchange (HIE)
- E-Prescribing
- Public Health and Clinical Data Reporting
Each objective contains specific measures (such as providing patient portal access, submitting immunization data, or sending electronic prescriptions) that must be reported annually.
4. How does PI relate to MIPS?
Promoting Interoperability is a scored category within MIPS. Performance in PI contributes to the composite MIPS score, which directly affects Medicare Part B payment adjustments. Poor PI reporting can lower the overall score, while strong PI performance helps protect against penalties.
5. What happens if I don’t participate in PI?
Clinicians who are required to participate but fail to report PI measures (and do not qualify for an exemption) automatically receive a zero score in the PI category. This can result in a negative payment adjustment under Medicare Part B for the corresponding adjustment year.
6. What exemptions are available for PI?
CMS offers PI hardship exemptions for certain clinicians and organizations. Examples include providers who:
- Have insufficient internet access
- Face extreme or uncontrollable circumstances
- Lack control over certified EHR technology
Exemptions must be applied for and approved by CMS each performance year.
