What Is an MAO (Medicare Advantage Organization)?
A Medicare Advantage Organization (MAO) is a private health plan that contracts with Medicare to provide Medicare Part A and Part B benefits through a Medicare Advantage (MA) plan. MAOs manage member coverage, provider networks, utilization management, and payment models while meeting Medicare program requirements for quality, access, and compliance.
Operationally, MAOs function as the administrator of care and payment within Medicare Advantage. They are responsible for building provider networks, managing authorizations, processing claims and encounters, coordinating benefits, and operating quality programs like Star Ratings. MAOs also carry significant compliance responsibilities tied to program integrity, including monitoring downstream providers and vendors for Fraud, Waste, and Abuse (FWA).
For providers and healthcare vendors, MAOs are key decision-makers because they define coverage rules, documentation expectations, payment policies, and operational workflows that directly affect care delivery and reimbursement.
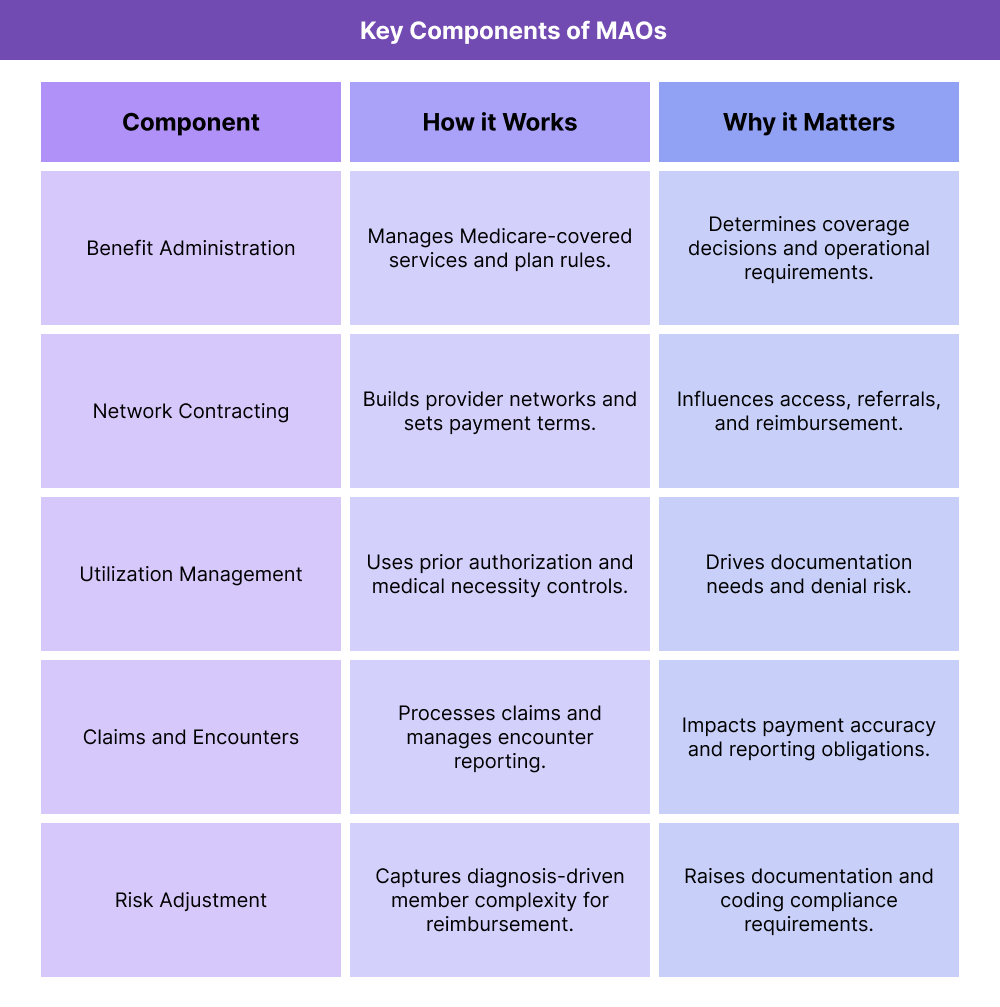
Key Components of Medicare Advantage Organizations (MAOs)
MAOs are not just payers—they are operational entities responsible for managing Medicare benefits under a regulated framework. These components explain how MAOs work and why they matter to provider organizations and partners.
MAO Plan Administration and Medicare Benefit Coverage
MAOs administer Medicare benefits through plan rules that must align with Medicare requirements while also reflecting plan design choices, such as supplemental benefits and network structures. This includes managing coverage determinations, member communications, and benefit coordination.
MAO Provider Networks and Contracting
MAOs build and manage provider networks, negotiate contracts, and establish payment methodologies. Network design affects access, referral patterns, and which providers are eligible to deliver covered services under the plan.
Prior Authorization and Utilization Management
MAOs commonly use prior authorization and utilization management to control cost and ensure services meet coverage and medical necessity standards. This has direct operational impact on scheduling, referrals, documentation quality, and denial management.
Claims, Encounters, and Payment Operations
MAOs process claims and collect encounter data that supports oversight, reporting, and payment integrity. For providers, MAO payment accuracy depends heavily on clean coding, timely submission, and documentation that supports medical necessity.
Risk Adjustment and Diagnostic Documentation
MAOs are responsible for risk adjustment processes that align member complexity with reimbursement. This creates strong operational emphasis on accurate diagnosis capture, documentation support, and compliant coding practices.
Quality Programs, Star Ratings, and Performance Measurement
MAOs participate in Medicare quality programs, including Star Ratings, which influence plan payments and market competitiveness. This drives operational focus on preventive care, chronic disease management, member experience, and closing care gaps.
Compliance, Program Integrity, and FWA Oversight
MAOs have explicit compliance responsibilities, including monitoring for FWA, managing delegated entities, and ensuring vendors and providers follow program requirements. This creates strong linkage to OIG priorities and enforcement risk.
How Medicare Advantage Organizations (MAOs) Work in Practice
Medicare Advantage Organizations operate as the primary administrators of care, coverage, and payment for Medicare Advantage (MA) members. In practice, MAOs replace traditional Medicare fee-for-service (FFS) administration with a managed model that combines network contracting, utilization management, quality programs, and financial risk.
For providers and vendors, working with an MAO means interacting with a payer that actively shapes how care is delivered, documented, and reimbursed—often with more operational touchpoints than FFS Medicare.
Step 1: Member Enrollment and Benefit Administration
MAO operations begin with member enrollment. Once a beneficiary enrolls in a Medicare Advantage plan, the MAO becomes responsible for administering their Medicare-covered benefits and any supplemental benefits offered by the plan.
Operationally, this includes:
- Managing eligibility and enrollment files
- Communicating benefit coverage and cost-sharing rules
- Coordinating Medicare benefits with supplemental or supplemental-like offerings
- Managing member materials and required notices
Errors at this stage can affect access, eligibility verification, and downstream billing accuracy.
Step 2: Provider Network Management and Contracting
MAOs build and manage provider networks that define where members can receive covered services. Network design directly affects access to primary care, specialists, post-acute care (such as HHA, IRF, and SNF services), and ancillary providers.
Operational responsibilities include:
- Contracting and credentialing providers
- Setting reimbursement methodologies and rates
- Managing network adequacy and access standards
- Monitoring downstream delegated entities
For providers, network participation determines patient volume, referral patterns, and payment terms.
Step 3: Utilization Management and Prior Authorization
One of the most visible MAO functions is utilization management. MAOs frequently require prior authorization for certain services, procedures, or settings of care.
In practice, this step affects:
- Scheduling and referral workflows
- Documentation quality and completeness
- Care delays when authorization is pending
- Appeals and reconsideration processes
Utilization management rules vary by MAO and are a major source of operational complexity for provider organizations.
Step 4: Claims Processing, Encounters, and Payment Operations
MAOs process claims submitted by providers and manage encounter data that supports oversight and reporting. While providers are paid by the MAO, encounter data also feeds CMS oversight processes.
Operational considerations include:
- Clean claims submission and adjudication
- Accurate coding and diagnosis capture
- Timely payment and reconciliation
- Management of denials and appeals
Because encounter data supports multiple downstream functions, errors can affect both payment and compliance.
Step 5: Quality Programs, Risk Adjustment, and Ongoing Oversight
MAOs operate under performance-based programs that directly affect revenue and market competitiveness. These include Star Ratings, risk adjustment, and member experience measures.
Operational focus areas include:
- Closing care gaps
- Capturing accurate diagnoses to reflect member complexity
- Monitoring quality metrics and performance trends
- Managing compliance with CMS requirements and audits
This step ties together clinical care, documentation, and financial performance in a tightly regulated environment.
MAOs in Billing, Reimbursement, and System Limitations
MAOs significantly shape billing and reimbursement workflows for Medicare Advantage providers. Unlike FFS Medicare, MAOs actively manage utilization, documentation expectations, and payment models.
How MAOs Affect Medicare Billing and Reimbursement
MAO reimbursement is governed by contract terms and plan policies rather than uniform Medicare FFS rules. This creates variability across plans and regions.
Common operational impacts include:
- Prior authorization requirements for covered services
- Different reimbursement methodologies (FFS-like, bundled, or value-based)
- Plan-specific billing and coding rules
- Increased documentation expectations to support medical necessity
For providers, this means billing workflows must be tailored to individual MAO requirements.
MAOs, Risk Adjustment, and Documentation Sensitivity
Risk adjustment is a core financial driver for MAOs. Accurate diagnosis documentation affects how plans are paid and how they manage population risk.
This creates heightened scrutiny around:
- Diagnosis capture and coding accuracy
- Clinical documentation completeness
- Audit readiness and retrospective reviews
- Alignment between clinical care and coded data
Weak documentation can create compliance risk and payment disruption, even when care delivery is appropriate.
MAOs, Compliance, and FWA Oversight
MAOs are explicitly responsible for monitoring downstream providers and vendors for Fraud, Waste, and Abuse (FWA). This includes implementing compliance programs, monitoring utilization patterns, and responding to potential issues.
Operationally, this can result in:
- Increased audits and chart reviews
- Data requests tied to utilization or quality concerns
- Contractual compliance requirements for providers and vendors
- Escalation to CMS or OIG when issues are identified
Providers working with MAOs must be prepared for ongoing oversight and documentation review.
System Limitations and Common MAO Operational Challenges
MAO-driven workflows introduce several system-level challenges:
- Policy variability: different rules across MAOs
- Authorization friction: delays and rework due to prior auth
- Data fragmentation: claims, encounters, and clinical data living in separate systems
- Retroactive reviews: post-payment audits affecting cash flow
- Provider burden: increased administrative work compared to FFS Medicare
Organizations that invest in strong intake, documentation, and authorization workflows are better positioned to manage MAO complexity.
How MAOs Influence Quality, Access, and Equity in Healthcare
MAOs play a central role in shaping Medicare beneficiary experience. Their policies influence not only cost and utilization, but also quality outcomes and access to care.
MAOs and Quality Improvement in Medicare
MAOs are financially incentivized to perform well on quality measures, which can drive investment in preventive care, chronic disease management, and care coordination.
When aligned well, MAO quality programs can improve outcomes. When poorly implemented, they can increase administrative burden without clear clinical benefit.
MAOs and Access to Care
Access under Medicare Advantage depends heavily on network design and authorization rules. Narrow networks or restrictive utilization management can limit provider choice and delay care.
Access challenges are often most acute in post-acute and specialty care settings, where network availability varies widely.
Equity Considerations in Medicare Advantage
Equity impacts emerge when MAO policies disproportionately affect certain populations. Administrative complexity, language barriers, and digital access issues can all influence member experience.
Equity-aware MAO operations often include:
- Clear, accessible member communications
- Support for care navigation and coordination
- Monitoring of access and outcomes across populations
- Adjustments to utilization management for vulnerable groups
When MAOs balance cost control with access and support, they can play a meaningful role in improving equity for Medicare beneficiaries.
Frequently Asked Questions about MAOs
1. What is an MAO (Medicare Advantage Organization) in healthcare?
A Medicare Advantage Organization (MAO) is a private health plan that contracts with Medicare to offer Medicare Part A and Part B benefits through a Medicare Advantage (MA) plan. MAOs manage member coverage, provider networks, utilization management, payment, and quality programs under Medicare rules.
2. What is the difference between Medicare Advantage (MA) and an MAO?
Medicare Advantage (MA) is the type of Medicare coverage (the plan product), while an MAO is the organization that operates and administers that Medicare Advantage plan. In practice, MA refers to the coverage option and MAO refers to the payer entity running it.
3. What do MAOs manage for Medicare Advantage members?
MAOs manage benefits, provider networks, prior authorization and utilization management, claims and encounter operations, care coordination programs, and performance measures such as Star Ratings. They also oversee compliance and program integrity requirements.
4. How do MAOs affect provider billing and reimbursement?
MAOs set plan-specific reimbursement policies and contract terms, which can differ from Medicare fee-for-service. Providers must often follow MAO rules around prior authorization, documentation requirements, coding standards, and denial management to receive timely payment.
5. Why do MAOs require prior authorization for some services?
MAOs use prior authorization to confirm that requested services meet coverage and medical necessity requirements and to manage utilization. While intended to control cost and ensure appropriate care, prior authorization can also create operational burden and delays if workflows are not well managed.
6. How do MAOs use risk adjustment and why does documentation matter?
MAOs use risk adjustment to align reimbursement with member health complexity. Accurate diagnosis documentation and compliant coding are essential because they affect payment, reporting, and audit exposure. Weak documentation can create compliance risk and financial disruption.
7. How do MAOs monitor Fraud, Waste, and Abuse (FWA)?
MAOs are required to maintain FWA compliance programs that include training, monitoring, auditing, and investigation processes. They often review utilization patterns, coding trends, and documentation quality across downstream providers and vendors as part of program integrity oversight.
8. How do MAOs influence quality and Star Ratings performance?
MAOs are evaluated on quality measures, member experience, and care outcomes through Star Ratings. This drives MAOs to invest in preventive care outreach, chronic condition management, closing care gaps, and care coordination programs to improve performance.
9. Can MAO network rules affect access to care?
Yes. MAO network design and utilization management policies influence which providers members can see, how quickly services can be scheduled, and whether referrals require authorization. Narrow networks or restrictive rules can create access challenges, especially for specialty and post-acute care.
