What Is an IRF (Inpatient Rehabilitation Facility) in Healthcare?
An Inpatient Rehabilitation Facility (IRF) is a specialized healthcare setting that provides intensive rehabilitation services to patients who require coordinated, multidisciplinary therapy following serious illness, injury, or surgery. In Medicare, IRFs are distinct provider types with specific admission criteria, coverage rules, and payment requirements.
From an operational standpoint, IRFs sit at the intersection of acute care, post-acute care, and value-based payment. Patients admitted to an IRF must be able to tolerate and benefit from intensive rehabilitation—typically multiple therapy disciplines delivered daily under physician supervision.
For providers, health systems, and Medicare Advantage organizations, IRFs are compliance-sensitive environments. Coverage, reimbursement, and audit risk depend heavily on admission decisions, documentation quality, and adherence to Medicare-specific IRF requirements. As a result, IRFs are frequently referenced in compliance reviews, program integrity work, and FWA monitoring.
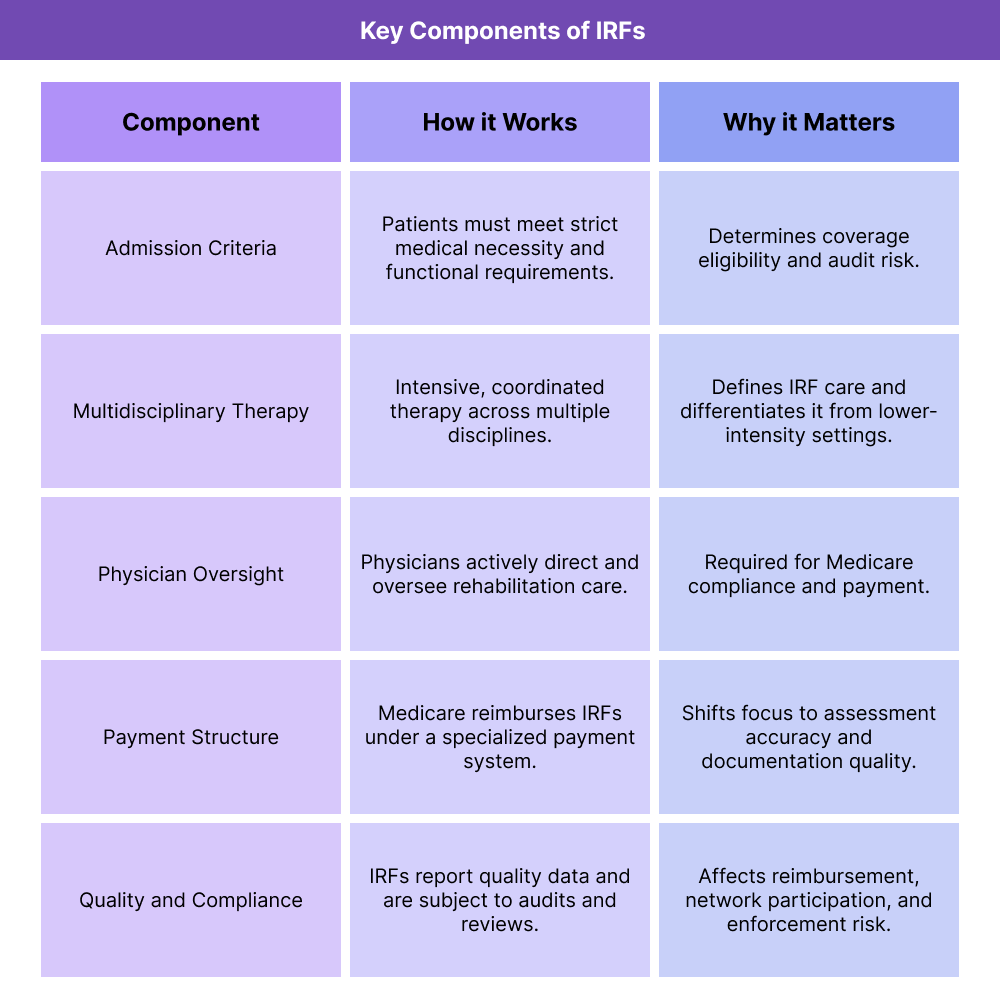
Key Components of Inpatient Rehabilitation Facilities (IRFs)
IRFs are governed by a structured set of clinical, operational, and reimbursement requirements. Understanding these components is essential for organizations that operate IRFs, refer patients to them, or manage post-acute care networks.
IRF Admission Criteria and Medical Necessity
Medicare coverage for IRF care is contingent on strict admission criteria. Patients must require intensive rehabilitation services that cannot be effectively provided in a less intensive setting, such as a SNF or home health environment.
Operationally, this requires:
- Clear documentation of the patient’s condition and functional limitations
- Evidence that the patient can participate in and benefit from intensive therapy
- Physician involvement in care planning and oversight
Admission decisions are a major focus of audits and reviews, making front-end documentation critical.
Multidisciplinary Therapy Requirements in IRFs
IRFs are defined by the delivery of coordinated, multidisciplinary therapy. Patients typically receive services from multiple therapy disciplines, such as physical therapy, occupational therapy, and speech-language pathology.
From a workflow perspective, this requires tight coordination across therapy teams, scheduling systems, and documentation practices to demonstrate intensity, frequency, and patient progress.
Physician Oversight and Care Planning in IRFs
Medicare requires active physician involvement in IRF care, including admission certification, ongoing oversight, and participation in interdisciplinary team meetings. This distinguishes IRFs from some other post-acute settings and adds an additional compliance layer.
Failure to document physician involvement appropriately can jeopardize coverage and reimbursement, even when therapy services are otherwise appropriate.
IRF Payment and Reimbursement Structure
IRFs are paid under a Medicare-specific payment system that differs from traditional fee-for-service models. Payment is generally based on patient classification and expected resource use rather than individual therapy minutes billed line by line.
This structure creates incentives for accurate assessment, coding, and documentation, while also increasing scrutiny around medical necessity and length of stay.
Quality Reporting and Compliance Expectations for IRFs
IRFs participate in quality reporting programs and are subject to oversight related to outcomes, functional improvement, and care transitions. Quality data is increasingly used by Medicare and Medicare Advantage organizations to assess network performance and post-acute care value.
Because IRFs operate in a highly regulated space, quality reporting, compliance monitoring, and FWA prevention are closely linked.
How Inpatient Rehabilitation Facilities (IRFs) Work in Practice
Inpatient Rehabilitation Facilities (IRFs) operate as highly structured post-acute care environments designed for patients who need intensive, coordinated rehabilitation following serious illness, injury, or surgery. In practice, IRFs function as a transition point between acute hospital care and lower-intensity settings such as skilled nursing or home health.
Operational success in an IRF depends on getting three things right from the start: admission decisions, care intensity, and documentation discipline.
Step 1: Patient Identification and Referral to an IRF
IRF care typically begins with a referral from an acute-care hospital. Discharge planners, case managers, and physicians assess whether a patient’s functional limitations and medical complexity warrant admission to an IRF rather than a SNF or home-based setting.
Key operational considerations at this stage include:
- Whether the patient meets Medicare’s IRF medical necessity criteria
- Whether the patient can tolerate and benefit from intensive therapy
- Whether required therapy disciplines are appropriate and available
- Whether the patient’s payer (Medicare FFS or Medicare Advantage) authorizes IRF care
This step is critical because inappropriate admissions are one of the most common drivers of audits and payment denials.
Step 2: IRF Admission, Certification, and Care Planning
Once a patient is accepted, IRF admission requires formal physician certification and documentation supporting the need for inpatient rehabilitation. Care teams develop an interdisciplinary plan that outlines therapy goals, expected intensity, and anticipated length of stay.
Operationally, this involves:
- Physician admission documentation and certification
- Interdisciplinary team assessments
- Therapy scheduling across multiple disciplines
- Baseline functional measurement and goal-setting
Early documentation quality here sets the tone for the entire stay and strongly influences audit defensibility.
Step 3: Delivery of Intensive, Multidisciplinary Rehabilitation
IRF care is defined by intensity and coordination. Patients typically receive daily therapy across multiple disciplines, supported by nursing and physician oversight.
Day-to-day operations focus on:
- Coordinating therapy schedules and staffing
- Documenting therapy minutes, patient participation, and progress
- Adjusting care plans based on patient response
- Maintaining physician involvement through regular review
This is also where operational strain can emerge. Staffing shortages, missed therapy sessions, or inconsistent documentation can quickly create compliance risk, even when care delivery is clinically appropriate.
Step 4: Ongoing Review, Documentation, and Compliance Monitoring
Throughout the IRF stay, teams continuously document patient progress, medical status, and therapy outcomes. Medicare and Medicare Advantage plans expect clear evidence that inpatient-level rehabilitation remains necessary.
Operationally, this includes:
- Ongoing physician progress notes
- Interdisciplinary team meeting documentation
- Therapy progress and goal updates
- Length-of-stay management
This step is closely tied to FWA monitoring, as prolonged stays without documented progress are often flagged for review.
Step 5: Discharge Planning and Care Transition
IRF care is transitional by design. As patients improve, teams plan discharge to the most appropriate next setting, such as home with home health services or a SNF for continued recovery.
Effective discharge planning includes:
- Clear documentation of functional gains
- Coordination with downstream providers
- Patient and caregiver education
- Accurate communication of discharge status to payers and partners
Poorly managed transitions can affect quality outcomes, readmissions, and payer evaluations of IRF performance.
IRFs in Billing, Reimbursement, and System Limitations
IRFs operate under a distinct Medicare reimbursement structure that creates both opportunity and risk. Payment is not driven by individual therapy services alone, but by patient classification, documented need, and compliance with coverage rules.
How IRFs Are Reimbursed Under Medicare
Medicare reimburses IRFs under a specialized prospective payment system rather than traditional fee-for-service billing. Payment is based on patient characteristics, clinical complexity, and expected resource use.
Operational implications include:
- Heavy reliance on accurate assessment and coding
- Less flexibility to “bill around” documentation gaps
- Increased scrutiny on admission appropriateness and length of stay
Medicare Advantage plans often apply additional authorization and utilization controls on top of these baseline rules.
Documentation as the Primary Reimbursement Driver
In IRFs, documentation is the foundation of payment. Even when therapy is delivered as required, weak documentation can result in denials or recoupments.
Common documentation risk areas include:
- Inadequate justification for inpatient-level care
- Inconsistent therapy intensity records
- Missing or incomplete physician certifications
- Poorly documented progress or lack of measurable improvement
Because IRFs are frequent targets for audits, documentation must support not just what was done, but why the IRF setting was necessary.
System Limitations and Operational Pain Points in IRFs
IRFs often face system-level challenges that increase administrative burden and risk:
- Complex documentation requirements across multiple disciplines
- Fragmented systems for therapy, nursing, and physician notes
- Staffing constraints that affect therapy intensity and scheduling
- Payer variability, especially between Medicare FFS and MA plans
- Audit lag, where reviews occur long after services are delivered
Organizations that invest in integrated documentation workflows and proactive compliance monitoring tend to perform better financially and operationally.
How IRFs Influence Quality, Access, and Equity in Healthcare
IRFs play a significant role in post-acute care quality and access, particularly for patients recovering from strokes, orthopedic injuries, neurological conditions, and complex medical events.
IRFs and Quality of Post-Acute Care
High-quality IRF care can lead to meaningful functional improvement, reduced long-term disability, and lower readmission rates. Quality is closely tied to:
- Therapy intensity and coordination
- Timely physician involvement
- Effective discharge planning
- Accurate measurement of functional outcomes
Because these outcomes are measurable, IRFs are increasingly evaluated based on performance rather than volume alone.
IRFs and Access to Intensive Rehabilitation
Access to IRF care can be uneven. Geographic availability, payer authorization policies, and staffing shortages all affect whether patients can receive inpatient rehabilitation when needed.
Medicare Advantage plans, in particular, may apply stricter criteria or prior authorization requirements, which can influence referral patterns and patient access.
Equity Considerations in IRF Utilization
Equity challenges arise when access to IRFs varies by socioeconomic status, geography, or payer type. Patients with limited advocacy support may be less likely to access IRF care, even when clinically appropriate.
Equity-focused IRF operations often emphasize:
- Clear, standardized admission criteria
- Strong advocacy during discharge planning
- Consistent documentation to support authorization decisions
- Collaboration with hospitals serving underserved populations
When implemented thoughtfully, IRFs can help reduce long-term disparities by restoring function and independence after major health events.
Frequently Asked Questions about IRFs (Inpatient Rehabilitation Facilities)
1. What is an IRF (Inpatient Rehabilitation Facility) in healthcare?
An Inpatient Rehabilitation Facility (IRF) is a specialized care setting that provides intensive, multidisciplinary rehabilitation for patients recovering from serious illness, injury, or surgery. IRFs deliver coordinated therapy services under physician oversight and follow Medicare-specific coverage and reimbursement rules.
2. What types of patients qualify for an IRF under Medicare?
Patients typically qualify for an IRF when they require intensive rehabilitation services, need close medical management, and can tolerate a high level of therapy. Coverage depends on medical necessity, functional limitations, and documentation showing that inpatient rehabilitation is needed rather than a lower-intensity setting.
3. How is an IRF different from a SNF (Skilled Nursing Facility)?
IRFs provide more intensive, coordinated rehabilitation with structured physician oversight and multidisciplinary therapy, while SNFs generally provide less intensive rehab and more custodial or skilled nursing-focused care. The admission criteria, reimbursement models, and documentation requirements also differ substantially.
4. How do Medicare Advantage plans handle IRF coverage and authorization?
Medicare Advantage plans often require prior authorization for IRF admission and may apply additional utilization management rules beyond Medicare’s baseline requirements. Approval typically depends on clear documentation of medical necessity, therapy needs, and why IRF-level care is required.
5. What documentation is required for IRF Medicare reimbursement?
IRF documentation typically must support admission appropriateness, physician certification, interdisciplinary care planning, therapy intensity, and measurable functional progress throughout the stay. Weak documentation is a common cause of denials and recoupments in IRF audits.
6. How are IRFs reimbursed under Medicare?
IRFs are reimbursed under a specialized Medicare prospective payment system, where payment is generally based on patient classification and expected resource use rather than line-by-line therapy billing. Accurate assessment, coding, and compliance with coverage rules are critical for payment.
7. Why are IRFs considered high-risk for audits and compliance reviews?
IRFs are audit-sensitive because reimbursement depends heavily on medical necessity, admission criteria, and documentation of therapy intensity and patient progress. Inconsistent admissions or weak documentation can trigger denials, recoupments, and program integrity scrutiny tied to FWA monitoring.
8. How do IRFs impact quality outcomes and readmissions?
High-performing IRFs can improve functional outcomes, accelerate recovery, and reduce hospital readmissions through intensive rehabilitation and strong discharge planning. Quality outcomes depend on coordinated therapy delivery, physician oversight, and effective transitions of care.
9. What are common operational challenges in IRF workflows?
Common challenges include staffing and scheduling constraints for therapy intensity, fragmented documentation across disciplines, payer authorization variability, and the administrative burden of maintaining audit-ready records throughout the stay.
