What is an Integrated Delivery Network (IDN)?
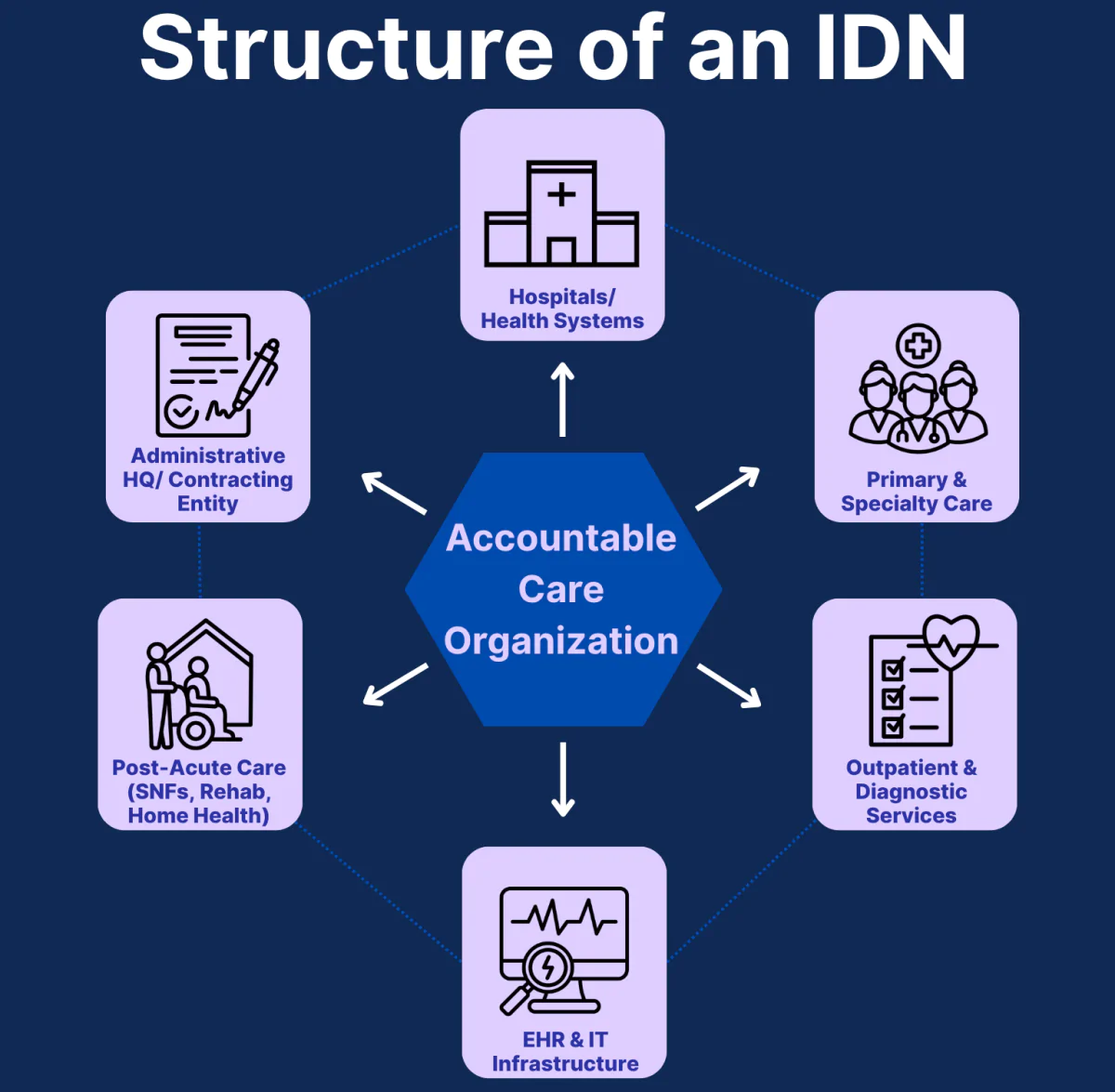
An Integrated Delivery Network (IDN) is a healthcare system made up of multiple provider types — such as hospitals, physician groups, and outpatient centers — that operate under a unified organizational and financial structure.
IDNs are designed to deliver the full continuum of care to patients, from primary care and specialty services to hospitalization and post-acute care. Their goal is to improve care coordination, reduce unnecessary utilization, and operate efficiently at scale.
Unlike looser affiliations or referral networks, IDNs share centralized governance, electronic health records, contracting, and often even branding. Many large health systems in the U.S. function as IDNs.
Key Components of a Clinically Integrated Network
- Centralized Governance: IDNs operate under a single administrative leadership, allowing for unified decision-making across care settings.
- Multiple Care Sites: They include a mix of hospitals, outpatient clinics, physician practices, urgent care centers, and post-acute facilities.
- Shared EHR and IT Systems: Most IDNs use a single electronic health record platform to streamline information flow and patient tracking across locations.
- Standardized Clinical Protocols: Care guidelines are consistent across the network, which supports quality assurance and evidence-based treatment.
- Risk-Based Contracting Capabilities: IDNs often engage in value-based contracts with payers, enabled by their broad scope and ability to manage population health.
- Branding and Patient Experience Integration: Many IDNs present a unified brand and patient portal, offering continuity of experience across care settings.
How Integrated Delivery Networks Work in Practice
An Integrated Delivery Network functions as a single healthcare organization, even though it’s made up of many distinct facilities and care teams.
Here’s how it typically operates:
- Unified Administration: Leadership teams oversee strategic planning, performance metrics, and clinical operations across all care sites.
- Cross-Continuum Care Coordination: From primary care to inpatient treatment to rehabilitation, care teams collaborate to ensure seamless patient transitions.
- Centralized Contracting: The IDN negotiates contracts with payers as a single entity, often securing favorable terms due to its size and care scope.
- Shared Infrastructure: Billing, scheduling, patient portals, and population health tools are integrated across the system.
- In-Network Optimization: Patients are often encouraged or incentivized to stay within the IDN for specialty referrals, diagnostics, and follow-up care.
Large systems like Kaiser Permanente and Intermountain Health are examples of IDNs that deliver coordinated care across an entire region.
Benefits and Challenges of Integrated Delivery Networks
Benefits of IDNs
- Continuity of Care: Patients receive services across the care continuum from a single, integrated system.
- Contracting Power: IDNs can negotiate more favorable payer contracts due to size and scope.
- Operational Efficiency: Shared IT systems, scheduling, and billing reduce duplication and streamline administration.
- Brand Cohesion: A unified brand experience across sites can improve patient trust and retention.
- Scalability for Value-Based Care: IDNs are well-positioned to support population health, bundled payments, and shared risk arrangements.
Challenges of IDNs
- High Capital Requirements: Building and maintaining IDN infrastructure requires significant investment in technology, facilities, and personnel.
- Integration Complexity: Aligning culture, workflows, and quality standards across disparate sites is an ongoing challenge.
- Referral Leakage: Despite internal networks, some patients still seek care outside the system, which can undermine coordination efforts.
- Bureaucratic Slowdowns: Large systems may face slower innovation cycles or decision-making processes due to administrative layers.
How Are Integrated Delivery Networks Paid?
Integrated Delivery Networks are not payers themselves — but they often negotiate and manage contracts on behalf of the facilities and providers within their network.
Here’s how it typically works:
- Fee-for-Service Billing: Most providers within an IDN still bill insurers or Medicare directly under traditional fee-for-service (FFS) models.
- Pooled Contracting: The IDN may negotiate contracts collectively with payers for improved rates, bundled payments, or shared savings programs.
- Value-Based Arrangements: Many IDNs participate in accountable care models or risk-based agreements, managing population health across their network.
- Internal Cost-Sharing Models: Some IDNs use internal budget targets, care benchmarks, or incentive pools to distribute resources and align goals between departments or entities.
In essence, the IDN streamlines how care is delivered and paid for across multiple service lines — but it does not replace the provider or hospital as the billing entity.
Frequently Asked Questions about IDNs
1. What is an Integrated Delivery Network (IDN)?
An IDN is a unified healthcare system that includes hospitals, physician groups, and outpatient services, all working under a shared administrative and financial structure.
2. What makes an IDN different from a hospital network?
While a hospital network may share branding or ownership, an IDN integrates clinical protocols, data systems, and value-based care strategies across all care levels.
3. Who pays an IDN?
IDNs themselves don’t bill patients. Instead, their providers bill under typical insurance models. The IDN negotiates contracts and may participate in shared savings or risk-based reimbursement.
4. Are all large health systems considered IDNs?
Not necessarily. To be an IDN, a system must integrate its care coordination, administrative processes, and contracting strategy. Many large systems qualify, but not all do.
5. What is the purpose of an IDN?
The goal of an IDN is to improve patient outcomes, reduce healthcare costs, and manage care more effectively across the entire treatment journey.
