What are Alternative Payment Models (APMs)?
Alternative Payment Models (APMs) are payment approaches developed by the Centers for Medicare & Medicaid Services (CMS) that reward healthcare providers for delivering high-quality, cost-efficient care. Instead of relying solely on fee-for-service billing, APMs tie reimbursement to value-based metrics such as patient outcomes, care coordination, and reduced healthcare spending.
APMs are part of the Quality Payment Program (QPP), alongside the Merit-based Incentive Payment System (MIPS). Providers who participate in qualifying Advanced APMs may earn additional incentives and become exempt from MIPS reporting requirements.
Key Components of APMs
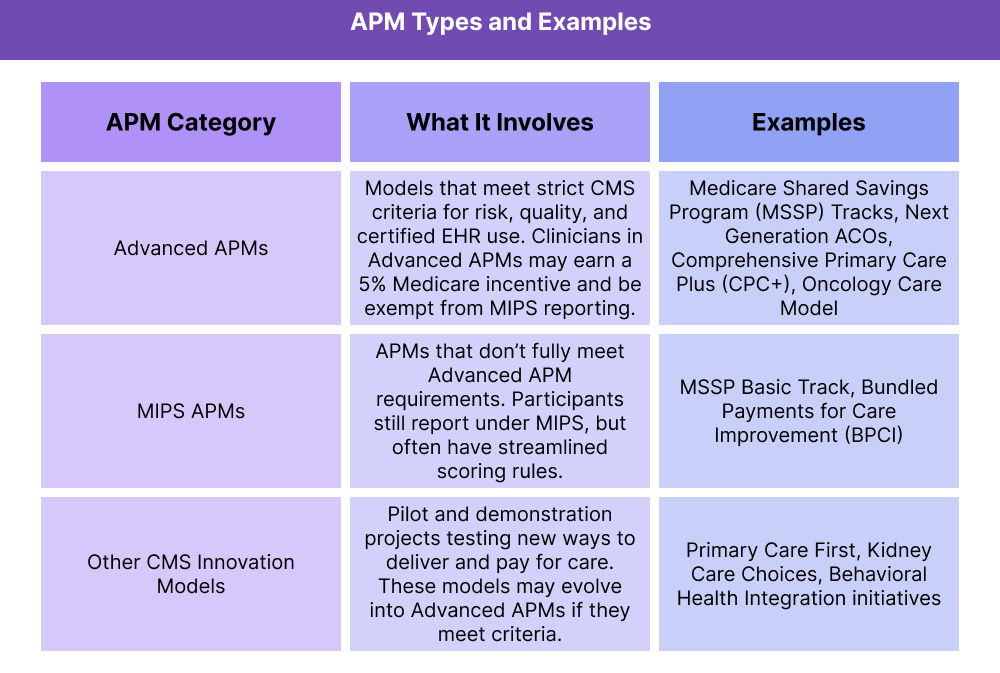
Alternative Payment Models (APMs) come in several forms, but all share the same goal: to shift healthcare from volume to value by aligning provider payment with quality and efficiency. CMS organizes APMs into categories that determine participation requirements and potential incentives.
Key Features Across APMs
- Value-Based Reimbursement: Payment depends on performance, not just service volume.
- Risk Sharing: Many APMs require providers to share in savings — and sometimes losses — based on cost and quality results.
- Care Coordination Focus: APMs often target chronic disease management, transitions of care, and population health improvements.
- Flexibility by Model: Requirements vary; some APMs require certified EHR use, others emphasize specific patient populations or specialties.
How APMs Work in Practice
Alternative Payment Models (APMs) reward providers for delivering high-value, cost-efficient care instead of focusing solely on the number of services provided. Here’s how participation typically works:
Step 1 — Join an APM Model
Providers or organizations choose to participate in a CMS-approved APM, such as an Accountable Care Organization (ACO) or a bundled payment model. Participation may be voluntary or tied to a larger healthcare network.
Step 2 — Deliver Care Under the Model
Providers care for patients following the model’s rules and goals, such as:
- Reducing hospital readmissions
- Coordinating chronic care management
- Meeting preventive care and quality benchmarks
Step 3 — CMS Evaluates Performance
At the end of the performance period, CMS analyzes:
- Quality metrics (patient outcomes, preventive screenings, safety indicators)
- Cost efficiency (total spending vs. benchmarks)
- Use of technology (EHR requirements, interoperability standards)
Step 4 — Payment Adjustment
Based on results, providers may:
- Earn shared savings or incentive payments if benchmarks are met or exceeded
- Face financial penalties if spending is higher than expected or quality metrics aren’t met
Step 5 — Program Updates and Evolution
CMS refines APMs regularly. Some models expand nationally, others end, and promising pilots may transition into Advanced APMs if they meet the criteria.
APMs and Their Impact on Billing and Reimbursement
Alternative Payment Models (APMs) are designed to shift reimbursement away from volume-based care toward value-based care. Instead of being paid solely on the number of services delivered, providers are rewarded for achieving better outcomes, improving coordination, and reducing costs.
How APMs Affect Payments
- Shared Savings and Risk: Many APMs allow providers to share in savings if they deliver care at a lower cost than expected, but some also require providers to take on downside risk if costs exceed benchmarks.
- Advanced APM Incentives: Clinicians who qualify under Advanced APMs may earn a 5% Medicare bonus payment on Part B services and become exempt from MIPS reporting.
- MIPS APMs: Participants in MIPS APMs still report under MIPS but may have streamlined scoring rules, affecting how their reimbursement adjustments are calculated.
- Innovation Models: Pilot APMs may offer incentives tied to specific populations (e.g., kidney care or primary care) but do not always guarantee broad reimbursement adjustments.
Financial Implications
- Bonuses for High Performance: Providers who meet quality and cost benchmarks can increase revenue through shared savings or incentive payments.
- Penalties for Poor Performance: If spending exceeds benchmarks or quality metrics aren’t met, providers may lose revenue under downside-risk models.
- Alignment with Value-Based Care: By rewarding outcomes instead of volume, APMs support the broader transition to value-based reimbursement models across U.S. healthcare.
Why This Matters
APMs represent a critical shift in Medicare reimbursement policy. For providers, success in these models means aligning financial performance with quality improvement and patient outcomes, rather than service volume alone.
Frequently Asked Questions about APMs
1. What is an Alternative Payment Model (APM)
An APM is a CMS payment approach that rewards providers for delivering high-quality, cost-efficient care. Instead of focusing only on the number of services provided, APMs tie reimbursement to outcomes, patient safety, and care coordination.
2. How are APMs different from MIPS?
MIPS adjusts Medicare payments based on a composite performance score across four categories, including quality and cost. APMs, on the other hand, focus on specific care delivery models such as Accountable Care Organizations (ACOs) or bundled payments. Clinicians in Advanced APMs may qualify for a 5% bonus and are exempt from MIPS reporting.
3. What qualifies as an Advanced APM?
An Advanced APM must meet strict CMS criteria, including:
- Using certified EHR technology
- Reporting on CMS-defined quality measures
- Bearing more than nominal financial risk (sharing in losses as well as savings)
Examples of Advanced APMs include Medicare Shared Savings Program (MSSP) Tracks, Comprehensive Primary Care Plus (CPC+), and the Oncology Care Model.
4. How do APMs affect Medicare reimbursement?
Providers in APMs may earn shared savings if they deliver care at lower-than-expected costs while maintaining quality standards. In downside-risk models, they may face penalties if costs exceed benchmarks. Clinicians in Advanced APMs also qualify for a 5% incentive payment on Medicare Part B services
5. What are examples of APM models?
APM models include:
- Accountable Care Organizations (ACOs)
- Bundled Payments for Care Improvement (BPCI)
- Comprehensive Primary Care Plus (CPC+)
- Primary Care First
- Kidney Care Choices
These models focus on specific populations, care settings, or clinical conditions.
6. Do APMs replace traditional Medicare fee-for-service?
No. APMs operate alongside fee-for-service billing, but they change how payments are adjusted by introducing shared savings, risk-sharing, and performance-based incentives.
