CPT 99497 Description, Billing Rules, & Use Cases
CPT 99497 is used to report Advance Care Planning (ACP) services, which involve face-to-face discussions about future medical care, end-of-life preferences, and documentation such as advance directives or POLST forms.
This code reflects the first 30 minutes of time spent by a physician or qualified healthcare professional (QHP) with the patient, family member, or surrogate in a voluntary, patient-centered conversation.
What is CPT Code 99497?
CPT 99497 is a time-based code that captures the first 30 minutes of Advance Care Planning services delivered during a face-to-face encounter. It applies when a provider leads a structured conversation focused on:
- Clarifying the patient’s values and care preferences
- Educating the patient about treatment options (e.g., resuscitation, mechanical ventilation, artificial nutrition)
- Discussing the role and legal implications of documents like:
- Advance directives
- Durable Power of Attorney for Healthcare
- Living wills or DNR orders
- Supporting surrogate decision-makers or family in understanding care goals
- Documenting the conversation and decision-making outcomes
CPT 99497 may be billed:
- During a dedicated ACP visit
- In addition to an E/M service (e.g., annual wellness visit)
- Regardless of whether the patient completes an advance directive
- As a standalone service, even if no other medical management is provided
If the conversation lasts longer than 30 minutes, additional time may be reported using CPT 99498.
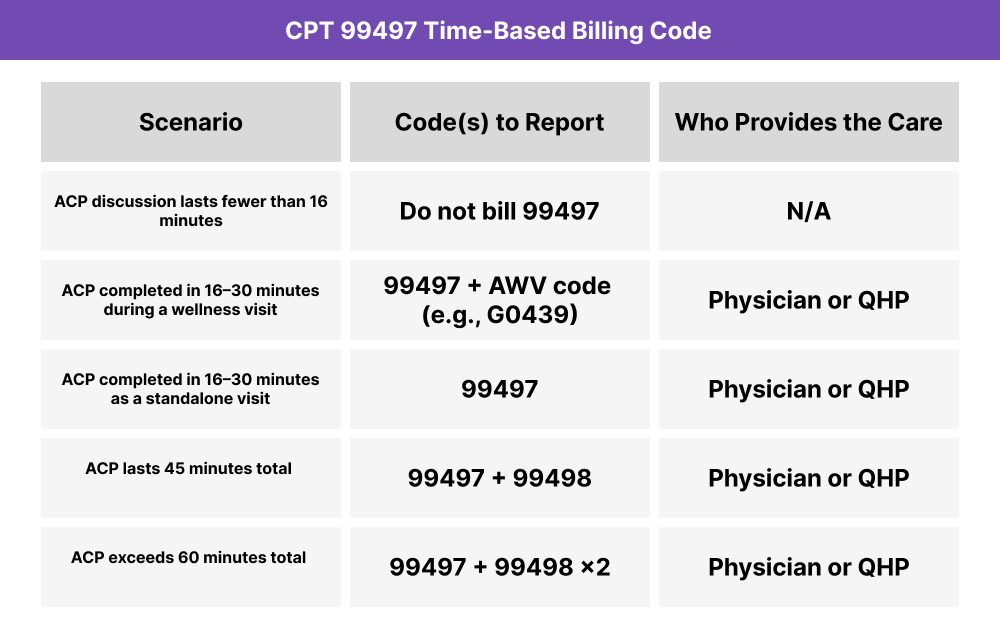
CPT 99497 Time Thresholds and Code Combinations
CPT 99497 is a standalone time-based code used to report the first 30 minutes of face-to-face Advance Care Planning (ACP). It may be reported alone or in conjunction with another service — but only when the minimum time and documentation requirements are met.
Important to Note:
- At least 16 minutes must be spent on face-to-face ACP activities to bill 99497
- If the conversation extends beyond 30 minutes, CPT 99498 may be used for each additional 30-minute block
- ACP may be billed:
- With an E/M service (e.g., 99214)
- During an Annual Wellness Visit
- As a standalone encounter with no other services
When to Use CPT 99497: Common Scenarios and Use Cases
CPT 99497 is appropriate when a provider spends at least 16 minutes in a face-to-face conversation discussing the patient’s goals of care, future medical decisions, and documentation like advance directives or living wills. The service may occur during any medically appropriate encounter.
Here are examples of how CPT 99497 is used in practice:
CPT 99497 Billing Requirements and Eligibility
CPT 99497 is used to report the first 30 minutes of Advance Care Planning (ACP) delivered in a face-to-face setting. It may be provided in any care location, and it can be billed on its own or in addition to other services, such as an annual wellness visit (AWV), chronic care encounter, or discharge planning session.
The goal of ACP is to help patients understand and express their treatment preferences in the event they are unable to speak for themselves.
Patient Eligibility Criteria
To bill CPT 99497, the patient must:
- Participate in a voluntary, face-to-face conversation
- Be cognitively able to engage in care discussions (or have a legally recognized surrogate present)
- Have medical circumstances or preferences that warrant planning (e.g., serious illness, aging, care transition)
- Consent to the discussion without coercion or incentive
ACP services may be offered to:
- New or established patients
- Patients with or without a terminal diagnosis
- Individuals at any age or stage of care when appropriate
Service and Documentation Requirements
To qualify for CPT 99497:
- The provider must spend at least 16 minutes (of the 30-minute code threshold) engaged in documented Advance Care Planning
- The service must be conducted face-to-face with the patient, family member, or surrogate
- The following should be documented:
- Time spent on the conversation
- Key discussion points (e.g., CPR preferences, goals of care, surrogate roles)
- Outcome of the discussion (e.g., advance directive created or deferred)
- Confirmation that the discussion was voluntary and patient-centered
Billing Frequency and Code Combinations
- CPT 99497 may be billed:
- With an E/M visit (e.g., 99214, 99397, or Annual Wellness Visit)
- As a standalone encounter, when no other services are performed
- If the ACP conversation exceeds 30 minutes, CPT 99498 may be reported for each additional 30-minute block
- There are no frequency limits, but documentation must support the time and medical relevance
Who Can Bill CPT 99497
CPT 99497 may be billed by:
- Physicians
- Nurse Practitioners (NPs)
- Physician Assistants (PAs)
- Other Qualified Healthcare Professionals (QHPs)
Clinical staff time does not count toward the threshold. All billable time must be personally performed by the billing provider.
CPT 99497 Billing Documentation Checklist
To support compliant billing of CPT 99497, include the following elements in the patient’s record:
- Patient consent and voluntary participation:
- Document that the patient (or surrogate) agreed to the ACP discussion
- Include a statement confirming the service was voluntary and not incentivized
- Time tracking:
- Total time spent in face-to-face Advance Care Planning
- Must reflect ≥16 minutes to qualify for billing
- Include exact or cumulative time logs
- Content of discussion:
- Description of topics covered, such as:
- Resuscitation preferences
- Mechanical ventilation or life-sustaining treatment
- Feeding tubes or hydration preferences
- Advance directives, living wills, or POLST forms
- Summary of patient or surrogate responses
- Documentation of goals-of-care values and priorities
- Description of topics covered, such as:
- Outcome of the discussion:
- Whether a new document was created, updated, deferred, or declined
- Location of advance directive (if completed) or next steps planned
- Any follow-up actions or referrals initiated
- Provider qualifications:
- Service was personally performed by a physician or QHP
- Clinical staff time was not included in the billed duration
- Coding context (if applicable):
- If billed with an E/M or Annual Wellness Visit:
- Clearly distinguish the ACP from the other service components
- Consider use of modifier –33 (preventive service) if appropriate
- If billed with an E/M or Annual Wellness Visit:
Common CPT 99497 Billing Mistakes (and How to Avoid Them)
❌ ACP Time Under 16 Minutes
CPT 99497 requires at least 16 minutes of face-to-face time. Billing with only 10–15 minutes documented, even if the content was thorough, does not meet the minimum threshold.
❌ No Documentation of Voluntary Participation
ACP services must be voluntary and patient-centered. Always include language noting that the patient (or surrogate) agreed to the conversation without coercion or incentive.
❌ Missing or Vague Discussion Details
”Reviewed advance directives” or “discussed goals of care” is not enough. You must specify:
- What was discussed (e.g., resuscitation, feeding tube preferences)
- Who was involved (patient or surrogate)
- What the outcome was (e.g., document completed, deferred, or declined)
❌ Billing Without Face-to-Face Contact
CPT 99497 cannot be billed for telephonic or asynchronous discussions. It requires a face-to-face encounter, either in person or via real-time video under applicable rules.
❌ Double Billing With E/M Without Clear Distinction
When ACP is performed during another billable visit, documentation must separate time and content from the E/M service. If not, 99497 may be denied as duplicative.
❌ Using 99497 Alone for Extended ACP Time
If the total provider time exceeds 30 minutes, remember to report CPT 99498 for each additional 30-minute block. Omitting the add-on code may lead to underbilling.



