Who Qualifies for Chronic Care Management?
What Do CMS’s Guidelines State?
Because CMS’s list of CCM-eligible conditions isn’t exhaustive, the provider’s discretion is often needed on a patient-by-patient basis. CMS does, however, outline some basic requirements that must be satisfied:
- The patient must have two or more chronic conditions, and
- The conditions must be expected to last at least 12 months or until the patient’s death, or
- The conditions must put the patient at risk of “death, acute exacerbation or decompensation, or functional decline.”
Defining Terms
Let’s dig a little deeper to understand the terms used in CMS’s criteria: Acute exacerbation, decompensation, and functional decline.
Acute Exacerbation:
An abrupt worsening of symptoms that could require immediate medical attention or lead to serious complications.
Example: A patient with congestive heart failure suddenly begins experiencing swelling in the legs and shortness of breath.
Decompensation:
The health condition deteriorates due to organ system failure. Compensatory mechanisms may additionally become exhausted or overwhelmed.
Example: A patient with type 2 diabetes that is normally well-managed begins experiencing extreme thirst and confusion, indicating the potential for diabetic ketoacidosis.
Functional Decline:
The gradual decrease of physical or cognitive abilities, including difficulties with mobility, communication, and other daily activities.
Example: A patient with Parkinson’s disease who was previously capable of performing everyday activities on their own now struggles with these tasks due to worsening tremors and bradykinesia.
What Conditions Qualify for Chronic Care Management?
The following is a sample list of chronic conditions that typically qualify a patient for CCM:
Cancer & Oncology Conditions
- Breast cancer
- Lung cancer
- Prostate cancer
- Colorectal cancer
- Leukemia
Cardiovascular & Blood Conditions
- Hypertension
- Congestive heart failure
- Anemia
- Diabetes
- Angina
Bone & Joint Conditions
- Rheumatoid arthritis
- Osteoporosis
- Chronic back pain
Eye Conditions
- Cataracts
- Glaucoma
- Age-related macular degeneration
Gastrointestinal Conditions
- Irritable bowel syndrome (IBS)
- Crohn’s disease
- Ulcerative colitis
Ear, Nose, & Throat Conditions
- Sleep apnea
- Vertigo
- Tinnitus
Mental Health & Neurological Conditions
- Depression
- Anxiety
- Alzheimer’s disease and dementia
- Post-traumatic stress disorder (PTSD)
- Autism spectrum disorder
Substance Use Disorders
- Alcohol use disorder
- Opioid dependence
- Nicotine dependence
Autoimmune Conditions
- Multiple sclerosis
- HIV/AIDS
- Hypothyroidism
- Viral hepatitis
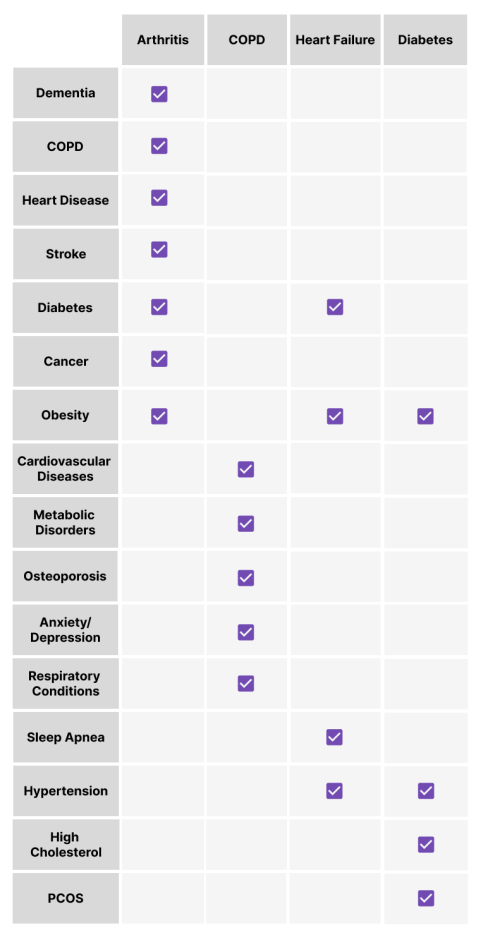
Common Multimorbid Conditions: A Visual Overview
As CMS’s guidelines state, patients must have two or more chronic conditions present to be considered for CCM. Below is a visual representation of some multimorbid conditions that are common in those who qualify.
Determining CCM Eligibility Doesn’t Have to Be Complicated
Trying to figure out which patients qualify for Chronic Care Management can feel like a daunting task—but with the right knowledge and tools it doesn’t have to be. A comprehensive CCM platform can help determine patient eligibility, all while boosting revenue and automating clinical workflows, so providers can focus more on direct patient care.
This content was created for and owned by Clinii. For all inquiries regarding distribution, please contact marketing@clinii.com.
Ready to Unlock the Benefits of CCM?
Let’s talk about how Clinii can help you launch or optimize your Chronic Care
Management program.



