What is a Skilled Nursing Facility (SNF)?
A Skilled Nursing Facility (SNF) is a licensed healthcare facility that provides round-the-clock medical care and rehabilitation services to patients who require a higher level of care than can be delivered at home but do not need acute hospitalization. Often used as post-acute care settings, SNFs serve patients recovering from surgery, stroke, injury, or chronic illness who need ongoing support from registered nurses, physical therapists, or other licensed professionals.
While the term “SNF” is often confused with “nursing home,” they are not the same — SNFs are Medicare-certified clinical facilities with defined care standards, while nursing homes may focus more on long-term custodial care.
How Skilled Nursing Facilities Work in Practice
Skilled Nursing Facilities (SNFs) operate as regulated, short-term care settings for patients who require daily medical support or rehabilitation following a hospital discharge. They play a critical role in the post-acute care continuum, often bridging the gap between inpatient hospitalization and home-based recovery.
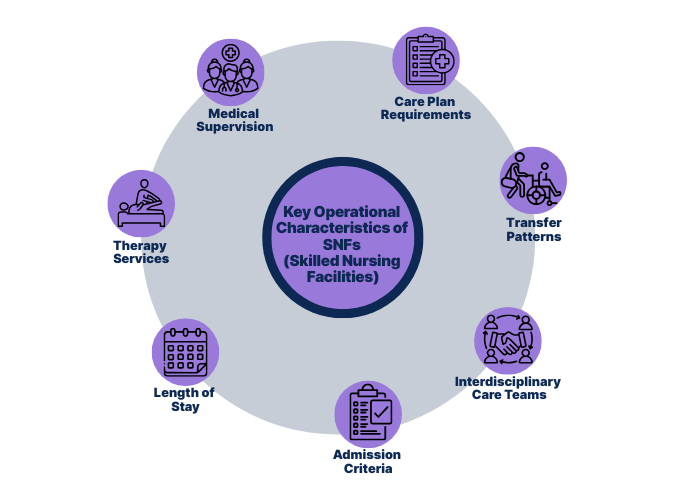
Key Operational Characteristics of SNFs:
- Medical Supervision: Each SNF has a physician or medical director who oversees patient care, supported by RNs, LPNs, nurse aides, and therapists
- Care Plan Requirements: Patients must receive a personalized care plan reviewed by a licensed clinician
- Therapy Services: Most SNFs offer physical, occupational, and speech-language therapy multiple times per week
- Length of Stay: Typically short-term (7–30 days), but can vary based on clinical need and payer coverage
- Admission Criteria: Must meet medical necessity and be ordered by a physician (especially for Medicare Part A billing)
- Interdisciplinary Care Teams: Include nursing, social work, dietary, therapy, and administrative professionals working together
- Transfer Patterns: Patients are commonly referred from hospitals and discharged to home, assisted living, or hospice
SNFs may also participate in value-based care initiatives, including Transitional Care Management (TCM), Principal Care Management (PCM), and remote care coordination programs.
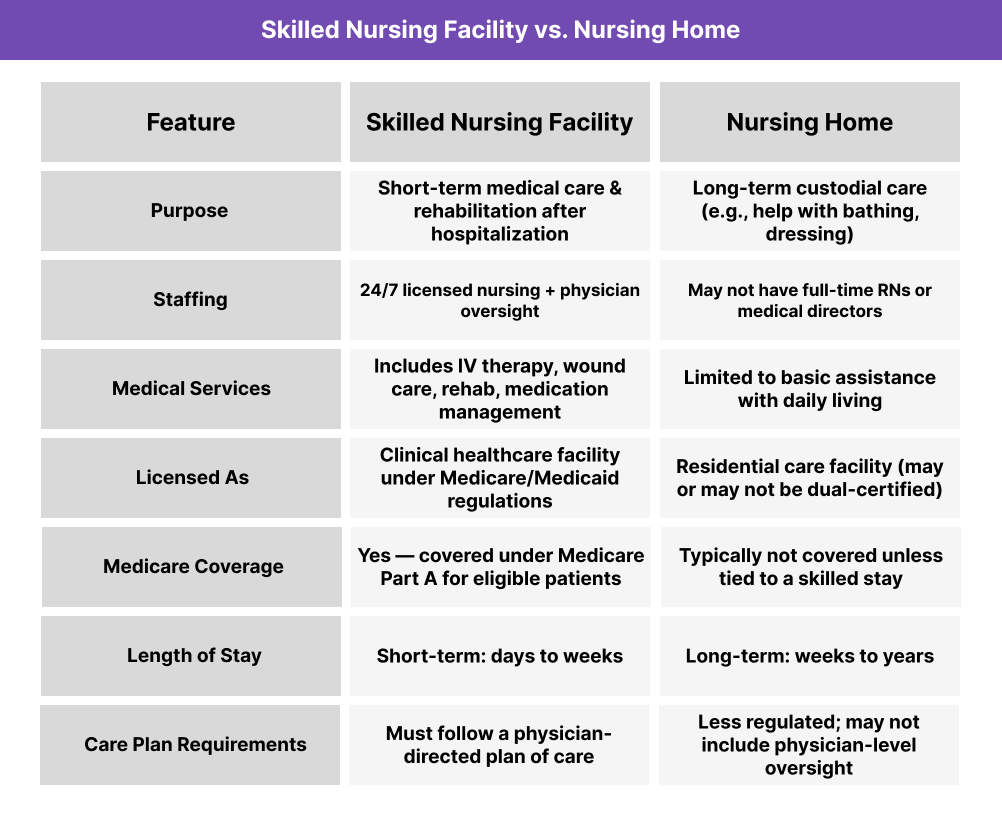
Skilled Nursing Facility vs. Nursing Home
Although the terms “Skilled Nursing Facility (SNF)” and “nursing home” are often used interchangeably, they refer to two very different types of care settings — especially in terms of medical scope, licensing, and reimbursement.
The chart to the right provides a visual comparison.
Benefits and Challenges of Skilled Nursing Facilities
Benefits of SNFs
- Medically Supervised Recovery: Patients receive 24/7 clinical oversight and structured therapy after discharge
- Medicare Coverage for Eligible Patients: Short-term SNF care is often covered under Medicare Part A for up to 100 days
- Supports Transitional Care Goals: SNFs help bridge the gap between inpatient hospitalization and home-based care
- Enables Intensive Rehab: Facilities provide physical, occupational, and speech therapy multiple times per week
- Reduces Readmission Risk: When managed well, SNF stays can prevent bounce-backs to the hospital
- Qualified Care Teams: Staff typically include RNs, PTs, OTs, social workers, and licensed administrators
Challenges of SNFs
- Strict Medicare Billing Rules: Must meet daily skilled care criteria, physician orders, and face scrutiny under SNF PPS audits
- High Operational Costs: Staffing, licensing, and regulatory compliance place pressure on margins
- Documentation Burden: Care teams must produce detailed MDS assessments, care plans, and progress notes
- Variable Quality: Performance, staffing ratios, and infection control standards vary significantly across facilities
- Discharge Planning Complexity: Coordinating transitions from SNF to home or hospice requires tight communication and often external support tools
- Limited Reimbursement Beyond Acute Need: Many SNFs face financial pressure once a patient no longer meets “skilled” status
Licensure and Certification for Skilled Nursing Facilities
In the US, Skilled Nursing Facilities (SNFs) are not “recognized” like FQHCs — instead, they must obtain state licensure and federal certification to legally operate and bill Medicare or Medicaid.
Licensure Requirements
- SNFs must be licensed as nursing facilities by their state’s health department or regulatory agency
- State licensure confirms compliance with fire, safety, staffing, and operational standards
- Requirements vary by state but generally include inspections, background checks, and staffing ratios
CMS Certification
To receive payment from Medicare or Medicaid, SNFs must be certified by the Centers for Medicare & Medicaid Services (CMS) under:
- Medicare Part A (Title 18) for skilled care reimbursement
- Medicaid (Title 19) for long-term care services
Certification is based on meeting Conditions of Participation, which include:
- 24/7 licensed nursing
- Medical director oversight
- Patient assessment and care planning
- Documentation and reporting (e.g., MDS)
SNFs are routinely surveyed by state survey agencies acting on behalf of CMS, and can lose certification if found out of compliance.
Reimbursement and Billing for SNFs
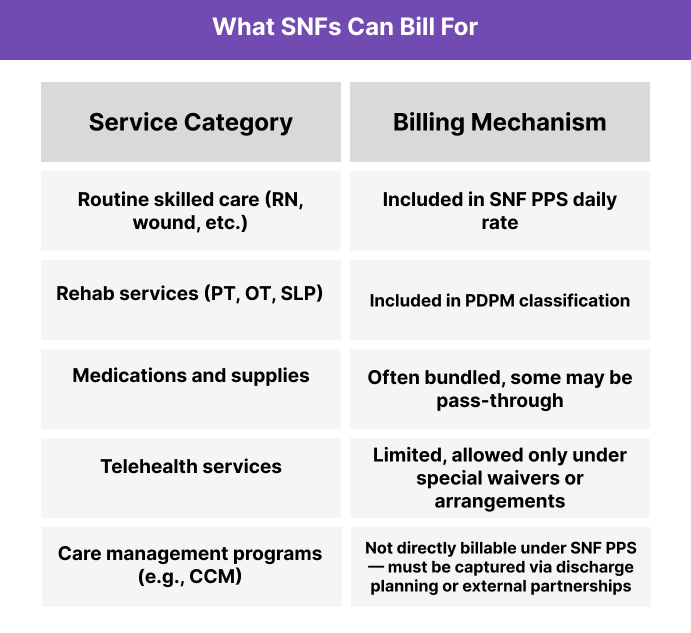
SNFs operate under a distinct payment structure known as the Skilled Nursing Facility Prospective Payment System (SNF PPS). This system is used by Medicare Part A to reimburse for short-term skilled care.
How SNF PPS Billing Works:
- Medicare pays a daily per diem rate based on the patient’s clinical profile, functional status, and therapy needs
- The system is powered by PDPM (Patient-Driven Payment Model) — not service-level CPT codes
- Billing is tied to accurate Minimum Data Set (MDS) assessments, which determine the case-mix classification
- Coverage is limited to up to 100 days per benefit period, with the first 20 fully covered and coinsurance applying after that
Frequently Asked Questions about SNFs
1. What is a Skilled Nursing Facility (SNF)?
A Skilled Nursing Facility (SNF) is a licensed clinical care setting that provides short-term medical treatment and rehabilitation services for patients recovering from illness, surgery, or hospitalization. SNFs are certified by Medicare and staffed with licensed nurses and therapy professionals.
2. How is an SNF different from a nursing home?
SNFs deliver short-term, medically necessary care — including IV therapy, wound care, and rehab — under physician supervision. Nursing homes provide long-term custodial care, such as help with bathing or eating, and often lack the same clinical staffing or Medicare coverage.
3. Who licenses and certifies SNFs?
SNFs must be licensed by their state health department and certified by CMS (Centers for Medicare & Medicaid Services) to bill Medicare and Medicaid. Certification requires compliance with federal Conditions of Participation and regular facility surveys.
4. What services can SNFs bill for?
SNFs bill Medicare under the SNF Prospective Payment System (SNF PPS). Covered services include skilled nursing, physical/occupational therapy, medications, and medical supplies — all bundled into a per diem rate based on the PDPM classification.
5. Can SNFs bill for care management programs like CCM or CoCM?
No — SNFs generally cannot bill directly for CCM or CoCM under PPS. These services may be addressed through discharge planning, external partnerships, or by eligible providers post-discharge.
