What Are Social Determinants of Health (SDOH)?
Social Determinants of Health (SDOH) are the non-medical factors that influence a person’s health outcomes. They include the conditions in which people are born, live, learn, work, and age—and the systems that shape those conditions.
These determinants can impact everything from access to care and treatment adherence to long-term wellness and quality of life. SDOH is increasingly central to value-based care models, risk adjustment, and clinical documentation workflows—especially in primary care and population health settings.
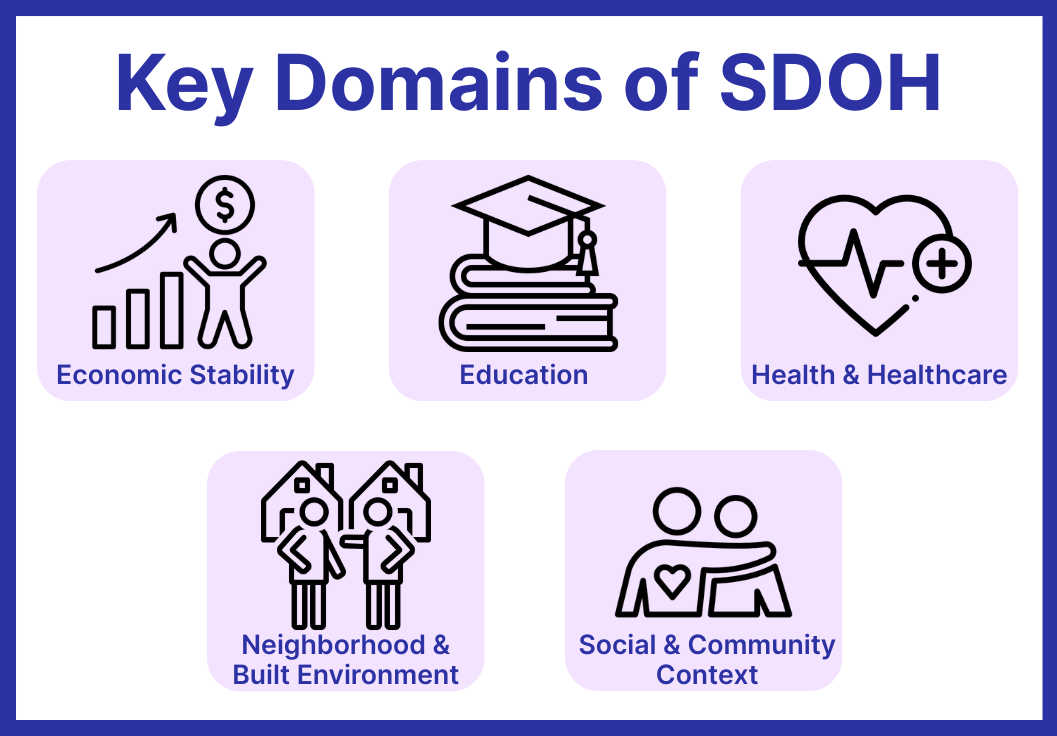
What Are the 5 Domains of Social Determinants of Health?
Health outcomes are shaped by far more than clinical care. The U.S. Department of Health and Human Services (HHS) categorizes Social Determinants of Health into five key domains:
-
Economic Stability: Includes access to stable income, employment, housing costs, food affordability, and financial security.
-
Education Access and Quality: Covers literacy, early childhood education, language barriers, graduation rates, and access to higher education or vocational training.
-
Health Care Access and Quality: Reviews caseloads weekly, provides treatment recommendations, and advises on medication or therapy adjustments based on patient response.
-
Neighborhood and Built Environment: Refers to housing safety, walkability, access to transportation, food deserts, air quality, and neighborhood violence.
-
Social and Community Context: Encompasses social support networks, community engagement, experiences with discrimination, and levels of chronic stress.
These domains often intersect. For example, a person with limited transportation access (domain 4) may also struggle to receive consistent care (domain 3).
How Social Determinants of Health Impact Care Delivery
Social Determinants of Health can significantly affect a patient’s ability to access care, follow treatment plans, and achieve long-term wellness. For providers and care teams, SDOH introduces factors that often fall outside the traditional clinical model but are essential to delivering effective, equitable care.
Examples of Impact:
- A patient with unstable housing may miss follow-up appointments
- Limited transportation can prevent timely prescription refills
- Language barriers can affect comprehension of discharge instructions
- Lack of access to healthy food may complicate chronic disease management
These factors influence outcomes at both the individual and population level. Addressing SDOH is essential for achieving health equity, reducing avoidable utilization, and succeeding in value-based care models.

Why Social Determinants of Health Matter in Healthcare
Improved Risk Adjustment
Capturing SDOH data—through Z codes or structured documentation—provides a more accurate view of patient complexity and population-level needs.
Better Care Coordination
Flagging social risks enables care teams to adjust workflows, prioritize follow-ups, and route patients to appropriate community resources.
Value-Based Care Alignment
SDOH-informed models support health equity initiatives, quality reporting, and contracts that reward preventive, whole-person care.
Competitive Differentiation
Payers, ACOs, and large employers increasingly look for partners that address root causes—not just clinical symptoms.
Addressing Social Determinants of Health in Clinical Workflows
Many healthcare organizations are building programs that identify and address social needs as part of standard care delivery. This may include:
- Screening patients for food insecurity, housing instability, or transportation issues
- Referring patients to local community-based organizations
- Documenting findings using standardized tools or coding systems
- Assigning care team members (e.g., social workers, community health workers) to follow up
One example of this in practice is Community Health Integration (CHI)—a care model designed to connect patients with local resources and provide structured, non-clinical support that complements medical treatment.
Frequently Asked Questions About SDOH
1. What are Social Determinants of Health?
Social Determinants of Health (SDOH) are non-medical factors that influence health outcomes. These include a person’s environment, economic situation, education, social context, and access to healthcare services.
2. Why are SDOH important in healthcare?
Because they shape up to 80% of a person’s health outcomes, SDOH help explain disparities in access, treatment success, and long-term wellness. Addressing them is essential for value-based care and health equity.
3. What are examples of common SDOH barriers?
Barriers include lack of transportation, food insecurity, housing instability, limited health literacy, and financial challenges that prevent patients from following treatment plans or attending appointments.
4. How do providers address SDOH?
Providers may screen for social needs, document them in the patient record, refer patients to support services, or engage care team members to provide follow-up and resource navigation.
5. What is the connection between SDOH and Community Health Integration?
Community Health Integration (CHI) programs are designed to address SDOH by linking patients with non-clinical support such as transportation, housing assistance, or food access—helping remove barriers to effective care.
