What is PRC (Patient Review and Coordination) in Healthcare?
Patient Review and Coordination (PRC) is a Medicaid program designed to ensure that members receive care safely and appropriately by consolidating their healthcare access through a single primary care provider and pharmacy. PRC is used when a member’s medical, pharmacy, or emergency department utilization suggests patterns that may be excessive, unsafe, or uncoordinated. Rather than restricting benefits, PRC redirects care through an assigned provider who oversees most non-emergent services.
From a business and operational perspective, PRC is both a care coordination framework and a utilization management mechanism. It helps Medicaid agencies and managed care organizations reduce avoidable emergency department visits, prevent duplicative or conflicting prescriptions, and ensure that high-risk members stay connected to a consistent care team. Many states refer to these programs as Patient Review and Restriction (PRR) or “lock-in” programs, but the intent remains the same: improve safety, accountability, and continuity of care.
In practice, members enrolled in PRC continue to receive full Medicaid benefits, but their routine services—appointments, prescriptions, referrals, and care management encounters—are expected to flow through their assigned primary care provider and pharmacy. For providers, health systems, and care management partners, understanding PRC is essential to navigating referrals, coordinating documentation, and keeping utilization aligned with program requirements.
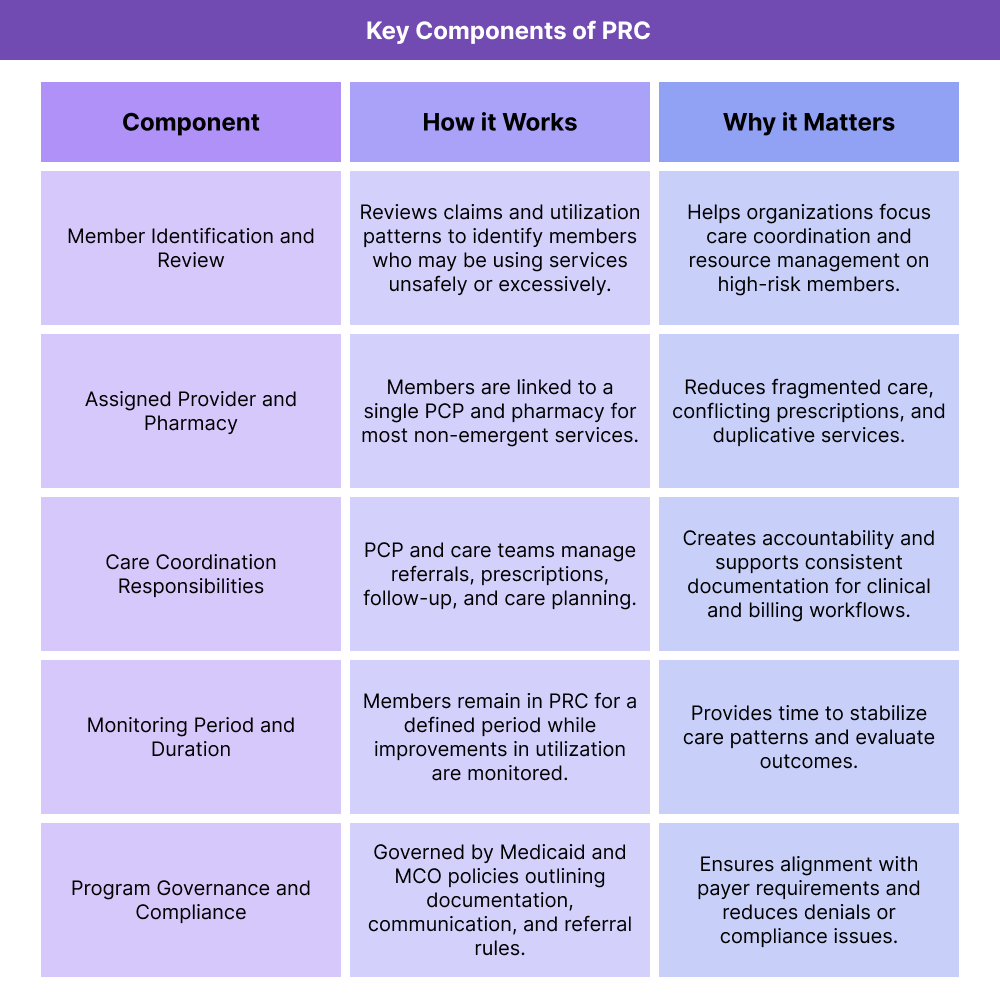
Key Components of PRC Programs
PRC programs share the same core purpose—supporting safe, coordinated care for high-risk Medicaid members—but each state or managed care organization implements the model slightly differently. At a high level, PRC programs follow a predictable structure: members are identified based on utilization patterns, enrolled in the program, assigned to a provider and pharmacy, and monitored over a defined period while maintaining full coverage.
Understanding these components is critical for health systems, FQHCs, RHCs, care managers, and vendors supporting PRC workflows, especially when navigating referrals, data exchange, and documentation.
Member Identification and Enrollment
PRC begins with a review of claims and care patterns to identify members whose healthcare use suggests risk—such as frequent emergency department visits, multiple prescribers for controlled substances, or inconsistent use of pharmacies. After meeting program criteria, members are enrolled in PRC and notified of their assigned provider and pharmacy.
Assigned Primary Care Provider and Pharmacy
Once enrolled, the member is linked to a single primary care provider and a single pharmacy responsible for most non-emergency care. Specialists may still see PRC members, but referrals, authorizations, and prescribing activity often must originate from the assigned provider. This structure reduces fragmentation and supports safer medication management.
Care Coordination Responsibilities
The assigned primary care provider becomes the central point for care planning, referrals, follow-up, and review of medical and pharmacy history. Care managers and interdisciplinary teams support outreach, appointment reminders, medication monitoring, and documentation needed to demonstrate medical necessity and compliance with PRC rules.
Monitoring Period and Duration
Members typically remain in PRC for a defined period—commonly 12 to 24 months—while the health plan evaluates whether utilization patterns have stabilized. Members may switch assigned providers under specific circumstances, but continuity is encouraged to strengthen coordinated care.
Program Governance and Compliance
PRC programs operate under state Medicaid rules, with additional policies defined by contracted managed care organizations. Each program outlines expectations for documentation, referrals, claims, medical necessity, patient communication, and provider roles.
How PRC (Patient Review and Coordination) Works in Practice
Patient Review and Coordination (PRC) programs sit at the intersection of clinical care, utilization management, and member safety. Day to day, they function as structured workflows that connect high-risk Medicaid members to a single accountable care team, while still allowing necessary access to hospitals, emergency departments, specialists, and community providers.
Operationally, PRC is a defined workflow:
- Identify members whose utilization patterns raise concern
- Enroll them in PRC and clearly communicate the change
- Assign a primary care provider and pharmacy
- Coordinate care and monitor utilization over time
- Reevaluate the member for continuation or graduation from PRC
For health systems, primary care practices, and care management vendors, understanding these steps is key to integrating PRC into scheduling, referrals, documentation, and population health workflows.
Step 1: Member Identification and Initial Review
PRC typically begins with a data-driven review of claims and care patterns. Health plans and Medicaid agencies analyze utilization to identify members who may be:
- Using multiple emergency departments for non-urgent care
- Filling overlapping or high-risk prescriptions from multiple prescribers
- Seeing many different PCPs or specialists without clear coordination
Clinical teams or utilization review staff then examine these patterns in more detail, confirm whether the member meets PRC criteria, and document why PRC is being considered. This step is critical for making sure the program is used consistently and fairly, and for giving providers a clear rationale when they receive PRC assignments.
Step 2: Enrollment, Notification, and Member Education
Once a member is approved for PRC, they are formally enrolled and notified—often through mailed letters, outreach calls, or care management contact. Communication explains:
- That their Medicaid benefits remain in place
- Which primary care provider and pharmacy they are being assigned to
- How to schedule visits and refill prescriptions going forward
- What to do in an emergency or when traveling
From a workflow standpoint, this is where scheduling teams, front-desk staff, and care managers need clear scripts and documentation so they can answer questions and redirect members appropriately. Good education up front reduces confusion, complaints, and denials later.
Step 3: Assigned Provider and Pharmacy Workflows
After enrollment, the assigned primary care provider and pharmacy become the central access points for most non-emergent care. In practice, this means:
- Appointment routing: Routine visits are booked with the assigned PCP or their team.
- Prescription consolidation: The assigned pharmacy fills most prescriptions and monitors for potential interactions or early refills.
- Referral management: Specialists and other prescribers are looped in through referrals, with the PCP documented as the coordinating provider.
For clinics and health systems, this step shows up in very practical ways: flags on the patient record, prompts in the EHR, payer-specific rules on which claims will be paid, and care management tasks to support PRC members. Vendors supporting PRC workflows often focus on surfacing PRC status inside the EMR, managing referral pathways, and logging PRC-related outreach.
Step 4: Ongoing Care Coordination and Utilization Monitoring
Throughout the PRC period, health plans and care teams monitor utilization trends and member outcomes. This may include:
- Tracking emergency department visits, urgent care use, and hospitalizations
- Reviewing prescription patterns, especially for controlled substances
- Monitoring no-show rates, follow-up adherence, and care plan engagement
- Documenting care management outreach, education, and social needs support
Care managers and population health teams use this data to prioritize outreach, close gaps in care, and adjust care plans. For many organizations, PRC members become a defined high-risk cohort with more frequent touchpoints, warm handoffs between inpatient and outpatient teams, and tighter communication between the PCP and pharmacy.
Step 5: Program Review, Continuation, or Graduation
PRC enrollment is not intended to be permanent. After a set monitoring period, the health plan or Medicaid agency reviews each member’s utilization and clinical status to determine whether:
- The member has stabilized and can be released from PRC
- The member would benefit from continued PRC enrollment
- A different care model (such as intensive case management or a specific behavioral health program) is more appropriate
Providers may be asked to contribute clinical context, especially when members have complex medical or behavioral health conditions. Clear documentation of visit reasons, prescriptions, and care management activities during the PRC period makes these decisions easier and more defensible.
For health systems and vendors, this final step reinforces the importance of having PRC workflows embedded in everyday practice—so that when the time comes to review the member, the organization can demonstrate not just controlled utilization, but coordinated, high-quality care.
PRC (Patient Review and Coordination) in Billing, Reimbursement, and System Limitations
Patient Review and Coordination (PRC) programs change how claims are routed, how providers appear in payer systems, and how documentation is reviewed on the back end. For revenue-cycle and operations teams, the key reality is that PRC is not just a clinical program—it is a billing and reimbursement rule set that must be reflected in workflows, contracts, and system configurations.
How PRC Affects Billing and Reimbursement
When a member is enrolled in PRC, the health plan expects most non-emergent services to be ordered, coordinated, or provided by the assigned primary care provider and pharmacy. That has several implications for prc billing and reimbursement:
- Claims from non-assigned providers may be denied or pended for review if they do not have appropriate referrals or PRC overrides.
- Pharmacy claims may be limited to the assigned pharmacy, with tighter review of controlled substances and overlapping prescriptions.
- Utilization management teams may apply additional reviews to emergency department visits and out-of-network encounters to confirm medical necessity.
From a revenue-cycle perspective, organizations need to know when a patient is in PRC before the claim is generated. That means eligibility checks, registration workflows, and front-end edits must surface PRC status early so staff can route appointments, referrals, and prescriptions through the correct provider.
PRC Documentation Requirements
Even though PRC does not change the underlying Medicaid benefit, it does change how closely documentation is scrutinized. Typical prc documentation requirements include:
- Clear identification of the assigned primary care provider and their role in ordering or coordinating services
- Visit notes that establish medical necessity, especially for high-cost imaging, procedures, or controlled substances
- Documentation of referrals, authorizations, and care management outreach, particularly when services are delivered outside the assigned provider or pharmacy
Weak documentation can lead to denials, recoupments, or disputes later, especially if a pattern suggests the member’s care is still fragmented despite PRC enrollment. For health systems, this puts added importance on tight prc workflow design and consistent documentation standards.
Coordination With Medicaid, Managed Care, and Other Payers
PRC programs are typically implemented by Medicaid fee-for-service and Medicaid managed care plans, but many members have overlapping coverage such as Medicare or commercial secondary insurance. Operationally, that can create:
- Confusion about which plan’s PRC rules apply when a member is dual-eligible
- Complex coordination between Medicaid PRC requirements and Medicare billing rules
- Additional burden on scheduling, care management, and RCM staff to interpret plan-specific guidance
Vendors and partners need to support configuration by plan and state so that PRC rules can vary without breaking core workflows. A “one-size-fits-all” approach to eligibility flags, claim edits, or referral routing often fails once organizations operate in multiple Medicaid markets.
System Limitations and Revenue-Cycle Watch-Outs
Common pressure points for PRC in healthcare include:
- Incomplete eligibility data: PRC status not flowing cleanly into EHR and practice management systems, leading to surprises at the claim level.
- Inconsistent provider mappings: Assigned PCPs or pharmacies not configured correctly in payer systems, producing denials even when providers think they are in-network and designated.
- Fragmented care management tools: Care managers tracking PRC members in spreadsheets or siloed tools instead of integrated platforms.
- Limited staff training: Front-desk, referral, and billing teams unsure how to handle PRC members, resulting in misrouted appointments and avoidable denials.
Addressing these gaps requires intentional design: clear flags in the EHR, automated work queues for PRC members, and shared playbooks across clinical, care management, and revenue-cycle teams.
How IHS Clinics Influence Quality, Access, and Equity in Healthcare
PRC programs are often viewed purely as cost-control tools, but they can significantly influence quality, access, and equity—especially for members with complex medical, behavioral health, or social needs. The way PRC is implemented determines whether it reduces risk and fragmentation or unintentionally creates new barriers.
PRC and Access to Primary Care
At their best, PRC programs strengthen access by ensuring each enrolled member has a clear “home base” in primary care. Members know who their main provider is, where to refill medications, and how to get non-emergency help. For practices that lean into prc in primary care, this can create:
- More predictable panels of high-risk members
- Opportunities to build trust over time with a consistent care team
- A clearer structure for proactive outreach instead of reactive ED use
However, if the assigned provider has limited capacity, inconvenient hours, or poor geographic accessibility, PRC can feel more like a restriction than a support. This is where careful provider selection, telehealth options, and transportation support become equity issues, not just convenience issues.
Quality and Care Management in PRC Programs
PRC members are often “frequent flyers” across emergency, inpatient, behavioral health, and pharmacy services. That makes them a logical focus for prc in care management and quality programs. Done well, PRC can:
- Improve medication safety by consolidating prescribing and pharmacy use
- Reduce duplicative tests and conflicting treatment plans
- Increase adherence to follow-up visits and chronic care appointments
- Create clearer accountability for closing gaps in care and addressing social needs
Care management teams can treat PRC members as a defined cohort with tailored pathways—for example, warm handoffs from ED to primary care, structured follow-ups after hospital discharge, and integrated behavioral health support for members with SUD, chronic pain, or serious mental illness.
Equity Considerations and Potential Unintended Consequences
Because PRC programs often focus on members with high utilization, they frequently include individuals with unstable housing, trauma histories, behavioral health conditions, or substance use. Those same populations already experience systemic barriers and stigma.
If PRC is implemented without an equity lens, it can:
- Make it harder for members to change providers when relationships are not working
- Increase administrative friction for members who move frequently or lack reliable contact information
- Reinforce punitive narratives around “misuse” of services instead of recognizing unmet needs and structural barriers
On the other hand, when PRC is framed as a supportive coordination program, paired with strong care management, culturally competent providers, and attention to social determinants of health, it can:
- Increase continuity for members who have historically bounced between many providers
- Improve safety for individuals at risk of overdose or medication-related harm
- Create more stable relationships that support behavior change and long-term health goals
Collaboration Across Systems
Finally, PRC programs shape how different parts of the healthcare system collaborate. Emergency departments, hospitals, FQHCs, behavioral health providers, and pharmacies all encounter PRC members. When information about PRC status, assigned providers, and care plans is easy to share, the system can respond in a coordinated way. When it is hidden, fragmented, or outdated, members experience mixed messages and avoidable friction.
For B2B partners—particularly health IT, care management platforms, and analytics vendors—PRC is an opportunity to design tools that respect plan rules while keeping quality, access, and equity at the center of the model.
Frequently Asked Questions about PRC
1. What is PRC (Patient Review and Coordination)?
Patient Review and Coordination (PRC) is a Medicaid program that assigns certain members to a single primary care provider and pharmacy to oversee most of their non-emergency care. The goal is to improve safety, reduce fragmented or potentially unsafe service use, and create a clear “home base” for high-risk members.
2. Does PRC limit a member’s Medicaid benefits?
No. PRC does not take away Medicaid benefits. Instead, it changes how members access their benefits by routing most routine care through their assigned primary care provider and pharmacy. Emergency services remain available, and medically necessary care is still covered when program rules are followed.
3. Who is placed in a PRC program?
Members are typically enrolled in PRC when their claims or utilization patterns suggest high risk or inappropriate use—such as frequent emergency department visits, overlapping prescriptions, or using several different providers without coordination. Criteria vary by state and plan, but the focus is on members who would benefit from more structured care oversight.
4. How does PRC affect providers and billing workflows?
PRC changes which claims are considered valid for payment. Most non-emergent services are expected to be ordered or coordinated by the assigned primary care provider. Claims from non-assigned providers may require referrals or special PRC authorizations. Identifying PRC status early in scheduling and registration helps prevent avoidable denials.
5. Can members change their assigned provider or pharmacy in PRC?
Yes, many programs allow changes when members move, need a different provider, or experience issues that affect continuity or trust. Changes are typically processed through the member’s health plan or Medicaid agency and may be limited to specific circumstances or timeframes.
6. How long do members stay in PRC?
PRC enrollment is usually time-limited, commonly 12–24 months. During this period, the plan monitors utilization, prescribing patterns, and primary care engagement. At the end of the cycle, members may graduate from PRC, continue in the program, or transition to another type of care management support.
7. Is PRC the same as prior authorization?
No. Prior authorization applies to specific services, tests, or medications. PRC is a member-level program that defines where and how a member should seek most of their care. A prior authorization may still be required, but PRC adds a layer of provider and pharmacy assignment.
8. How does PRC interact with emergency and urgent care visits?
Emergency services are always available. PRC members can still use the emergency department when medically necessary. However, plans may review frequent ED use more closely and coordinate follow-up to redirect members to primary care whenever appropriate.
9. Does PRC support quality and safety, or is it just about cost?
PRC supports both. While reducing unnecessary costs is one goal, consolidating care with a single provider and pharmacy improves medication safety, reduces conflicting treatment plans, and strengthens continuity—especially for members with complex medical or behavioral health needs.
10. How can care management and health IT tools support PRC?
Effective tools make PRC status visible during eligibility checks, scheduling, prescribing, and care planning. They help track referrals, surface high-risk cases, support documentation needs, and standardize workflows so organizations can meet PRC requirements while improving member outcomes.
