What is PPPS (Personalized Prevention Plan Services)?
Personalized Prevention Plan Services (PPPS) are the structured preventive-care elements that CMS requires clinicians to deliver during the Medicare Annual Wellness Visit (AWV). PPPS involve creating or updating an individualized prevention plan based on a beneficiary’s current health status, medical and family history, and a completed Health Risk Assessment (HRA). The purpose is to identify modifiable health risks early and map out recommended preventive services for the coming year.
PPPS are not a separate stand-alone visit; they are embedded within the AWV benefit and reflected in the AWV HCPCS codes. The initial AWV (G0438) and subsequent AWV (G0439) both include PPPS as a required core component, meaning the preventive plan must be documented and communicated to the patient in order for the visit to meet CMS coverage standards. Through PPPS, providers translate risk findings into a forward-looking care roadmap that supports preventive screening, immunizations, behavioral risk reduction, and follow-up planning.
From a practice and billing perspective, PPPS are a compliance-critical deliverable within the AWV workflow. Clear documentation of the prevention plan and its linkage to the HRA helps confirm that the AWV was performed according to CMS expectations, reduces audit vulnerability, and strengthens the clinical value of preventive care by ensuring the visit results in actionable, personalized next steps.
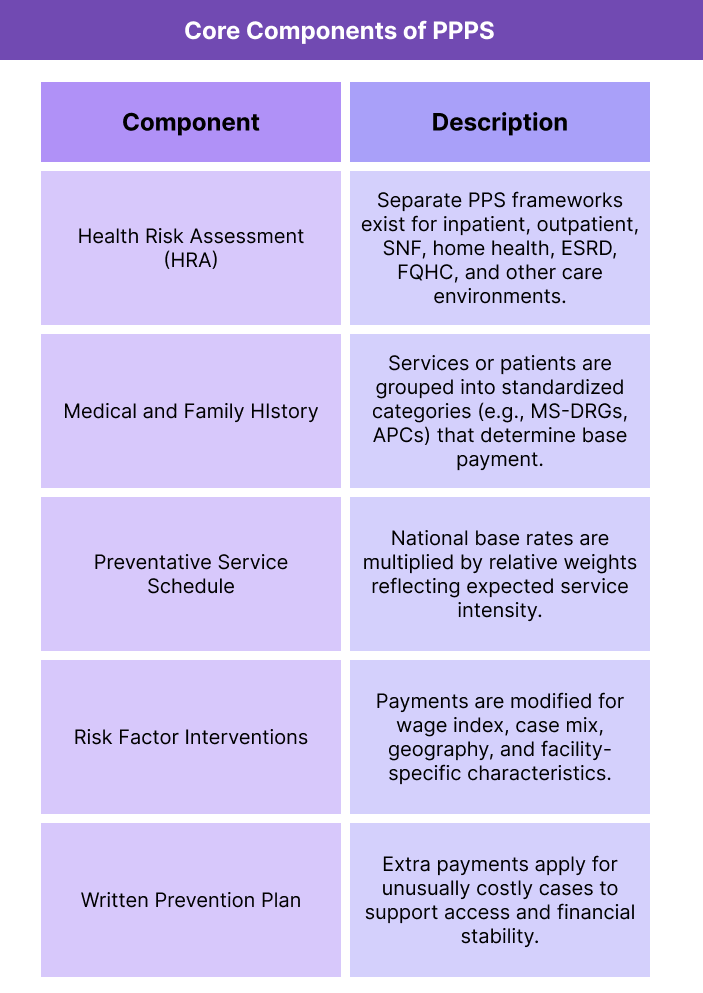
Key Components of PPPS
Personalized Prevention Plan Services (PPPS) make up the required preventive-care deliverables within the Medicare Annual Wellness Visit. They translate the Health Risk Assessment (HRA) and clinical history into a documented, patient-specific prevention roadmap that guides screenings, risk reduction, and follow-up for the next 12 months.
While PPPS are delivered during the AWV, they function as their own structured preventive planning package with specific CMS-required elements that must be completed and documented for the visit to qualify for coverage.
Health Risk Assessment (HRA) Foundation
PPPS are built on a completed HRA, which gathers standardized information about a beneficiary’s health status, functional ability, behavioral risks, and psychosocial factors. The HRA serves as the baseline dataset that drives the prevention plan.
Medical and Family History Review
Clinicians must review and update the patient’s medical and family history, including current providers, conditions, medications, and relevant risk factors. This ensures the prevention plan reflects the patient’s clinical reality and ongoing care needs.
List of Current Providers and Suppliers
PPPS include confirming or updating the list of clinicians, specialists, and suppliers involved in the patient’s care. This supports care coordination and ensures preventive recommendations align with the broader care team.
Preventive Screening and Immunization Schedule
A core PPPS element is developing a schedule for recommended preventive services over the next year. This includes age- and risk-appropriate screenings, immunizations, and Medicare-covered preventive benefits tailored to the beneficiary.
Risk Factor Identification and Intervention Recommendations
PPPS require identifying health risks and conditions that may benefit from behavioral counseling, chronic disease prevention, or early intervention. The prevention plan should link identified risks to clear, actionable recommended steps.
Personalized Prevention Plan Document
The prevention plan must be summarized in a written format and provided to the beneficiary. This document functions as the official PPPS output and is required for the AWV to meet CMS standards.
How PPPS Works in Practice
Personalized Prevention Plan Services (PPPS) are delivered as the operational core of the Medicare Annual Wellness Visit (AWV). In practice, PPPS convert the Health Risk Assessment and clinical review into a structured preventive roadmap that providers update annually. The workflow is designed to ensure preventive care is proactive, individualized, and tied to Medicare-covered benefits.
1. The Patient Completes a Health Risk Assessment
Before or during the AWV, the beneficiary completes an HRA that captures functional status, psychosocial risks, lifestyle factors, and self-reported health concerns. This becomes the primary input for prevention planning.
2. The Clinician Reviews History and Current Care Context
The provider reviews and updates the patient’s medical and family history, confirms active conditions, medications, and care-team involvement, and identifies any newly emerging risks that should influence preventive priorities.
3. Risks Are Identified and Prioritized
Using the HRA and clinical review, the care team identifies health risks such as chronic disease progression, fall risk, depression, substance use concerns, nutrition or activity gaps, and barriers to adhering to preventive screenings.
4. A 12-Month Preventive Plan Is Created
The provider develops a personalized schedule of Medicare-covered preventive services for the year ahead. This includes screenings, immunizations, counseling, and any follow-up evaluations that match the beneficiary’s risk profile and eligibility.
5. The Plan Is Documented and Shared
The prevention plan is summarized in a written document that is either provided to the patient at the visit or made accessible through the patient portal. This document serves as the formal PPPS deliverable required by CMS.
6. The Plan Guides Ongoing Preventive Care
The PPPS output functions as a yearlong reference point for the patient and the care team. It supports follow-through on screenings, referrals, behavioral counseling, and care coordination between AWVs.
PPPS in Billing, Reimbursement, and System Limitations
Personalized Prevention Plan Services (PPPS) are a required component of the Medicare Annual Wellness Visit (AWV) and are embedded in the AWV benefit structure. While PPPS are not billed as a standalone service, CMS considers them a core deliverable that must be completed and documented for an AWV to qualify for coverage and payment.
How PPPS Are Billed Within the AWV
PPPS are included within the AWV HCPCS codes rather than reported separately. The initial AWV code (G0438) and subsequent AWV code (G0439) both represent visits “including PPPS,” meaning the prevention plan is part of what Medicare is paying for. If the PPPS elements are missing or incomplete, the AWV may fail coverage requirements even if other parts of the visit were performed.
PPPS Documentation Requirements
To support compliant AWV billing, the prevention plan must be clearly documented as an individualized, forward-looking roadmap based on the Health Risk Assessment and clinical review. Documentation should show that risks were assessed, a preventive screening schedule was created, and the plan was provided to the beneficiary. The prevention plan should be easy to locate in the record, as it is one of the most straightforward elements for auditors to validate.
Common Billing Errors and Denial Triggers
Organizations can face AWV denials or recoupments when PPPS elements are not properly completed. Frequent issues include missing evidence of a finalized prevention plan, lack of linkage between the HRA and plan recommendations, or failure to provide a copy of the plan to the patient. Another risk area is billing G0438 or G0439 when the beneficiary is not eligible (for example, too soon after a prior AWV), which can lead to automated denials regardless of PPPS quality.
PPPS vs Routine Physical Exams
PPPS are part of the AWV preventive planning benefit, which is distinct from a routine physical exam. If the encounter is documented or delivered as an annual physical rather than a preventive planning visit, Medicare may consider it non-covered. Providers must maintain clear separation between AWV/PPPS workflows and problem-oriented E/M services, which should be billed separately only when medically necessary and properly documented.
System Limitations and Workflow Friction
PPPS can be operationally intensive because they require structured data collection, risk interpretation, preventive planning, and patient-facing documentation in a single visit. Practices without strong AWV workflows may struggle with time burden, inconsistent plan quality, or incomplete documentation. Digital HRA tools and standardized plan templates often help reduce friction and protect compliance, but uneven adoption across sites can create variability in billing performance.
How PPPS Influences Quality, Access, and Equity
PPPS are designed to improve preventive care delivery for Medicare beneficiaries by ensuring that wellness visits result in a personalized and actionable prevention roadmap rather than a generic screening checklist.
PPPS and Preventive Care Quality
By requiring an individualized prevention plan, PPPS push AWVs beyond risk identification toward concrete follow-through. When implemented well, PPPS support earlier detection of chronic disease, improved adherence to screenings and immunizations, and better alignment between patient risk profiles and recommended preventive services.
Access to Preventive Services Through PPPS
PPPS can expand access by formalizing preventive recommendations and embedding them into a covered annual benefit. For beneficiaries who may not otherwise receive routine preventive planning, PPPS create a structured opportunity for clinicians to identify gaps and connect patients to appropriate covered services over the year ahead.
Equity Implications for Underserved Populations
PPPS have the potential to reduce disparities by creating a consistent preventive planning standard for all Medicare beneficiaries. However, equity gains depend on whether practices are equipped to address social risk factors identified in the HRA. Beneficiaries facing transportation barriers, low health literacy, housing instability, or limited local service availability may require more intensive planning and follow-up than standard PPPS workflows provide.
Risk Identification and Social Determinants Sensitivity
Because PPPS are driven by HRA findings, the quality of equity impact depends on how thoroughly the assessment captures behavioral, functional, and psychosocial risks. If HRAs are overly generic or not adapted for language and cultural accessibility, PPPS may under-identify needs in diverse populations and miss opportunities to improve preventive engagement.
Long-Term Community and System Outcomes
Over time, PPPS can support healthier aging and reduced downstream costs by reinforcing consistent preventive care. Their population-level impact is strongest when practices pair AWV prevention plans with ongoing outreach, chronic care coordination, and referral infrastructure that helps high-risk beneficiaries complete recommended services.
Frequently Asked Questions about PPPS
1. What is PPPS?
Personalized Prevention Plan Services (PPPS) are the preventive-care planning elements required during the Medicare Annual Wellness Visit (AWV). They include an individualized prevention roadmap based on the Health Risk Assessment and clinical history, outlining recommended screenings, immunizations, and risk-reduction steps for the next 12 months.
2. Are PPPS a separate billable service?
No. PPPS are not billed on their own. They are built into the AWV benefit and included in the payment for G0438 (initial AWV) and G0439 (subsequent AWV).
3. What is included in a PPPS prevention plan?
A PPPS plan typically includes identified health risks, a personalized schedule of Medicare-covered preventive services, and recommendations for counseling or follow-up based on the beneficiary’s risk profile.
4. What role does the Health Risk Assessment play in PPPS?
The HRA is the foundation for PPPS. It provides standardized information about the beneficiary’s functional status, psychosocial risks, behavioral factors, and self-reported health concerns, which drive the prevention plan.
5. Do providers have to give the prevention plan to the patient?
Yes. CMS requires the prevention plan to be documented and provided to the beneficiary (in print or electronically). Without evidence that the plan was shared, the AWV may not meet coverage requirements.
6. What are common documentation mistakes that put AWV billing at risk?
Common issues include missing proof of a finalized prevention plan, no clear linkage between the HRA findings and plan recommendations, or burying the plan in the record where it is hard to verify.
7. How are PPPS different from an annual physical?
PPPS are part of the AWV preventive planning benefit, which focuses on risk assessment and future preventive needs. A routine annual physical is a head-to-toe medical exam and is not covered by Medicare as an AWV.
8. Can problem-oriented E/M services be billed with an AWV that includes PPPS?
Yes, but only if a significant, separately identifiable medical issue is evaluated and documented. The AWV/PPPS must remain clearly distinct from the problem-oriented portion of the visit.
9. How often can PPPS be provided?
PPPS are provided once per AWV. Medicare covers an initial AWV after eligibility is met, and then one subsequent AWV every 12 months, each including updated PPPS.
10. Who can perform PPPS within the AWV?
A physician or qualified healthcare professional must oversee the AWV, but clinical staff can assist with HRA collection and plan preparation as allowed under practice policy, as long as required elements are completed and documented properly.
11. Why do PPPS matter for preventive care outcomes?
PPPS turn risk identification into a concrete year-ahead prevention roadmap, increasing the likelihood that beneficiaries complete screenings, immunizations, and risk-reduction steps tied to Medicare benefits.
12. What makes a PPPS plan “personalized” under CMS expectations?
A PPPS plan should reflect the beneficiary’s specific risks and history, not a generic checklist. It should show tailored preventive priorities, timelines, and follow-up recommendations based on the HRA and clinical review.
