What is a Patient-Centered Medical Home (PCMH)?
A Patient-Centered Medical Home (PCMH) is a care delivery model designed to improve patient outcomes through coordinated, team-based primary care. In a PCMH, providers take a holistic approach to health management — emphasizing long-term patient relationships, accessibility, and proactive care planning rather than episodic treatment.
Many primary care practices adopt the PCMH model to strengthen care continuity, support value-based reimbursement strategies, and enhance performance in programs like Chronic Care Management (CCM) and Principal Care Management (PCM).
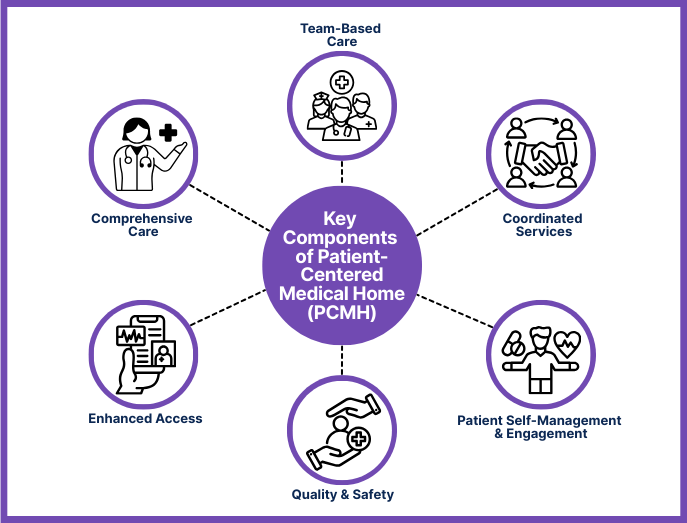
Key Components of a Patient-Centered Medical Home (PCMH)
- Ongoing, team-based patient-provider relationships
- Whole-person, comprehensive care approach
- Enhanced access to care through flexible scheduling and communication
- Coordinated services across the broader healthcare system
- Commitment to continuous quality improvement and safety
- Emphasis on patient self-management and engagement
These elements may be formalized through certification by NCQA, The Joint Commission, or similar accrediting bodies.
How Patient-Centered Medical Homes Work in Practice
The Patient-Centered Medical Home model transforms the traditional primary care practice into a coordinated, patient-first care hub. Instead of treating individual symptoms during isolated visits, PCMHs aim to manage whole-person health over time, especially for patients with chronic or complex conditions.
Key features of how the PCMH model operates:
- Team-Based Care: Physicians, nurse practitioners, care coordinators, behavioral health providers, and administrative staff work as a unified care team.
- Care Continuity: Patients are assigned a primary care provider who oversees their ongoing care and acts as their central point of contact.
- Enhanced Access: Many PCMHs offer extended hours, same-day appointments, telehealth services, and secure messaging to improve accessibility.
- Data-Driven Decision-Making: EMR systems and population health tools help practices proactively identify gaps in care and manage risk.
- Care Coordination: PCMHs communicate directly with specialists, hospitals, and community services to ensure seamless transitions and follow-up care.
This model supports both Value-Based Care goals and reimbursement eligibility for programs like Chronic Care Management (CCM), Principal Care Management (PCM), and Transitional Care Management (TCM).
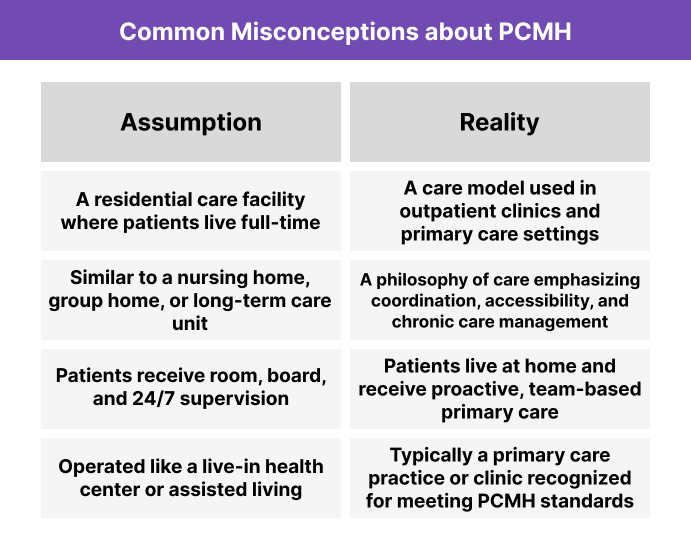
Is a PCMH a Residential Facility?
Although the name “Patient-Centered Medical Home” might suggest a residential care setting, it actually refers to a care delivery model used in outpatient primary care. The word “home” is metaphorical—not a place where patients live, but rather a central hub for coordinating all aspects of a patient’s ongoing healthcare.
Benefits and Challenges of the PCMH Model
Benefits of the PCMH Model
- Improved Patient Outcomes: Coordinated care and long-term provider relationships lead to better chronic condition management and preventive care uptake.
- Higher Patient Satisfaction: Patients value greater access, personalized attention, and continuity of care.
- Eligibility for Reimbursement Programs: Many PCMHs participate in CCM, PCM, and other CMS-aligned care management initiatives.
- Support for Value-Based Care: Practices can align more easily with ACOs, MCOs, or payer incentive programs by demonstrating quality and coordination.
- Streamlined Workflows Through Team-Based Care: Distributing tasks across a care team can reduce clinician burnout and improve operational efficiency.
Challenges of the PCMH Model
- Resource Intensive to Implement: Transitioning to a PCMH often requires new staffing models, training, and technology investment.
- Certification and Recognition Can Be Complex: Meeting standards from accrediting bodies like NCQA or The Joint Commission involves documentation and evaluation.
- Workflow Redesign: Shifting from episodic care to team-based, longitudinal care can disrupt established routines.
- Requires Strong Health IT Infrastructure: EMR optimization, care management tools, and data reporting are critical but not always in place.
- Sustainability Depends on Payer Alignment: Financial success with the model often hinges on supportive payer contracts or participation in value-based programs.
PCMH Recognition and Participation
Practices don’t need formal certification to follow the Patient-Centered Medical Home model — but many pursue official recognition to validate their commitment to coordinated, high-quality care and to qualify for incentive programs.
Who Recognizes PCMHs?
- NCQA (National Committee for Quality Assurance) – the most widely used PCMH accreditor in the U.S.
- The Joint Commission – offers PCMH recognition as an add-on to ambulatory care accreditation
- AAAHC (Accreditation Association for Ambulatory Health Care) – offers a Medical Home accreditation option
Each organization has its own standards and review process, often involving:
- Documentation of care coordination and access
- Demonstration of quality improvement initiatives
- Patient experience metrics
- Integration of population health tools and EMR usage
Who Can Become a PCMH?
PCMH recognition is typically available to:
- Primary care practices, including family medicine, internal medicine, and pediatrics
- FQHCs (Federally Qualified Health Centers) and RHCs
- Multi-site or health system-affiliated clinics
- Independent practices participating in ACOs or value-based contracts
While specialty practices are not typically recognized as standalone PCMHs, they often participate as extensions of a recognized primary care PCMH.
Reimbursement and Billing for PCMH-Aligned Care
While there is no single CPT code that directly reimburses a practice for being a Patient-Centered Medical Home, recognized PCMHs are better positioned to bill for care coordination and chronic care services under Medicare and commercial payer programs.
Common Billing Codes for PCMH-Aligned Practices
- Chronic Care Management (CCM) — CPT 99490, 99439, 99487, 99489
- Principal Care Management (PCM) — CPT 99424, 99425, 99426, 99427
- Transitional Care Management (TCM) — CPT 99495, 99496
- Collaborative Care Model (CoCM) — CPT 99492, 99493, 99494
These codes require strong documentation, care team coordination, and consistent patient engagement — all core features of the PCMH model.
Value-Based Payment Opportunities
Many payers and state Medicaid programs offer:
- PCMH recognition bonuses
- Per-member-per-month (PMPM) care coordination payments
- Shared savings programs tied to PCMH performance metrics
In many cases, PCMH recognition by NCQA or other accrediting bodies is required to access these incentives.
Frequently Asked Questions about PCMHs
1. What is a PCMH?
A Patient-Centered Medical Home (PCMH) is a primary care model that emphasizes long-term patient relationships, care coordination, and whole-person health management. It is not a physical residence, but rather a framework for delivering proactive, team-based outpatient care.
2. Is a PCMH a type of residential care facility?
No. A PCMH is not a nursing home or group home. It refers to an outpatient care model where a patient’s primary care provider acts as the central hub for managing their ongoing health needs.
3. Do you need to be certified to be a PCMH?
Not necessarily. Any practice can follow PCMH principles, but formal recognition from organizations like NCQA, The Joint Commission, or AAAHC is often required to participate in payer incentive programs.
4. What are the requirements for PCMH recognition?
Requirements vary by accrediting body but usually include:
- A designated care team
- 24/7 access to clinical advice
- Regular quality improvement efforts
- Strong care coordination and follow-up
- Use of electronic health records and data tools
5. What services can PCMHs bill for?
PCMHs often provide and bill for Chronic Care Management (CCM), Principal Care Management (PCM), and Transitional Care Management (TCM). These services align naturally with the PCMH model due to their focus on continuous care, patient engagement, and clinical oversight.
6. What’s the difference between a PCMH and an ACO?
While both aim to improve care quality and reduce costs, a PCMH is a primary care practice model, while an Accountable Care Organization (ACO) is a broader healthcare network that may include hospitals, specialists, and other providers. A PCMH can operate independently or as part of an ACO.
