What is a Nurse Practitioner (NP)?
A Nurse Practitioner (NP) is an advanced practice registered nurse (APRN) who is licensed to assess, diagnose, treat, and manage acute and chronic health conditions. NPs hold a graduate degree in nursing—typically a Master of Science in Nursing (MSN) or Doctor of Nursing Practice (DNP)—and are certified by national nursing boards.
In Medicare-recognized care management programs, NPs are considered Qualified Health Professionals (QHPs) and are eligible to bill directly for services under models like Chronic Care Management (CCM), Principal Care Management (PCM), Transitional Care Management (TCM), and Collaborative Care (CoCM). NPs often function as the lead clinician or supervising provider for other care team members.
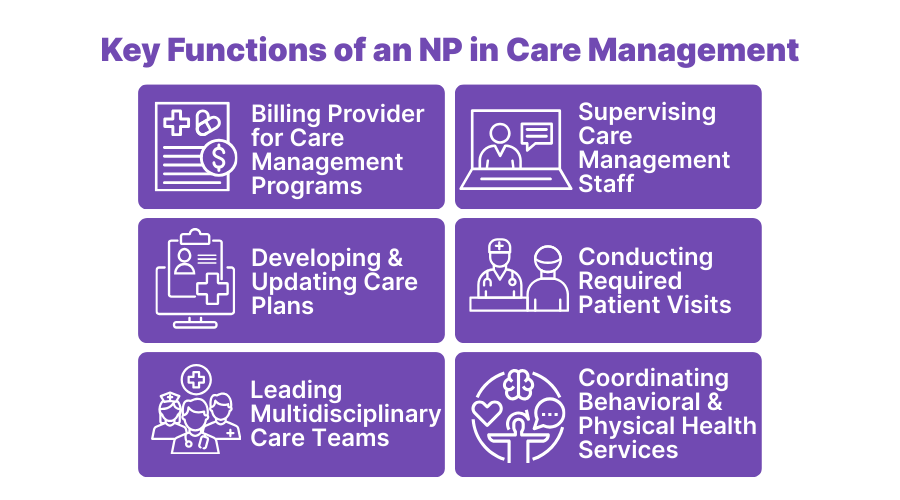
Key Functions of an NP in Care Management
Nurse Practitioners are central to the delivery and coordination of chronic and longitudinal care. Their dual training in clinical care and patient education makes them well-suited for managing Medicare billing programs that require documentation, supervision, and continuity.
Common functions of an NP in CMS care management models include:
- Serving as the billing provider for CCM, PCM, TCM, and CoCM
- Supervising care management staff performing non-face-to-face services
- Creating, reviewing, and updating patient care plans
- Conducting initial or follow-up face-to-face visits required for billing eligibility
- Leading multidisciplinary care teams in both primary and specialty settings
- Coordinating behavioral and physical health services in Collaborative Care Models
NPs are particularly valuable in rural or high-volume clinics where physician availability is limited. Their ability to bill directly and provide comprehensive care makes them critical to sustainable care management programs.
The Role of a Nurse Practitioner in Care Delivery
Nurse Practitioners serve as frontline clinical leaders in a variety of healthcare environments, from primary care clinics to specialty practices. With training rooted in both medicine and nursing, NPs offer a unique blend of diagnostic authority and patient-centered support that aligns closely with CMS’s care management goals.
In daily practice, NPs often:
- Act as the primary provider managing high-risk and chronic patients
- Lead care management programs, overseeing clinical and documentation workflows
- Supervise and delegate tasks to RNs, LPNs, and care coordinators
- Serve as the point of continuity for patients transitioning across care settings
- Bridge medical and behavioral care teams in integrated models like CoCM
- Ensure compliance with billing regulations, time-tracking, and program-specific criteria
Because NPs are licensed to evaluate, prescribe, and coordinate care, they are frequently used to expand access and drive revenue in both independent practices and enterprise health systems.
Billing and Supervision Rules for Nurse Practitioners
Nurse Practitioners are fully authorized to bill Medicare for a wide range of care management services when properly credentialed. As Qualified Health Professionals (QHPs), NPs can independently fulfill billing, supervision, and documentation roles within time-based and service-based CMS care models.
Care management programs NPs may bill for include:
- Chronic Care Management (CCM): CPT 99490, 99439, 99491
- Principal Care Management (PCM): CPT 99424–99427
- Transitional Care Management (TCM): CPT 99495–99496
- Collaborative Care Model (CoCM): CPT 99492–99494
- Annual Wellness Visits, Advance Care Planning, and more
Nurse Practitioner Supervision Capabilities:
NPs may oversee clinical staff (e.g., RNs, medical assistants, care coordinators) delivering non-face-to-face services. Their attestation and documentation fulfill CMS’s supervision requirements, allowing the practice to meet billing criteria without direct physician involvement.
Note: Some state laws may still place limits on NP autonomy, particularly for prescribing or initiating care plans. However, from a Medicare billing standpoint, NPs are fully eligible to lead care management programs.
Frequently Asked Questions about Nurse Practitioners NPs
1. What is a Nurse Practitioner (NP)?
A Nurse Practitioner is an advanced practice registered nurse (APRN) licensed to diagnose, treat, and manage a wide range of patient conditions. NPs may work independently or collaboratively depending on state laws, and they often serve as primary care providers.
2. Can an NP bill Medicare for care management services?
Yes. NPs are Qualified Health Professionals (QHPs) under CMS and may bill directly for services like Chronic Care Management (CCM), Principal Care Management (PCM), Transitional Care (TCM), and the Collaborative Care Model (CoCM).
3. Is a Nurse Practitioner allowed to supervise other clinical staff for billing purposes?
Yes. NPs may supervise RNs, care coordinators, and other staff performing non-face-to-face care management activities. They are responsible for attesting to time and ensuring documentation meets CMS standards.
4. How does an NP compare to a Physician Assistant (PA)?
NPs and PAs have overlapping scopes of practice and can both bill Medicare for care management services. NPs are trained in a nursing model and may operate more autonomously in states with full practice authority. PAs are trained in the medical model and typically work under formal collaboration or supervision agreements with physicians.
5. What CMS billing codes can NPs use in care management?
NPs can bill 99490 and 99439 for CCM, 99424–99427 for PCM, 99495–99496 for TCM, and 99492–99494 for CoCM, among others. They must be enrolled as Medicare providers and follow program-specific documentation guidelines.
6. Are NPs recognized as Qualified Health Professionals (QHPs) by CMS?
Yes. NPs are explicitly recognized as QHPs in CMS documentation and are eligible to independently bill for a wide range of time-based and service-based care codes.
