What is IPPE (Initial Preventative Physical Examination)?
The Initial Preventive Physical Examination (IPPE)—often referred to as the “Welcome to Medicare” visit—is a one-time benefit available to Medicare Part B enrollees during their first 12 months of coverage. While it’s sometimes mistaken for a routine physical, the IPPE is actually a comprehensive preventive assessment designed to establish a patient’s health baseline and identify future risk factors.
For healthcare providers, understanding how the IPPE works is critical—not only for delivering proactive care but also for ensuring proper Medicare billing and documentation.
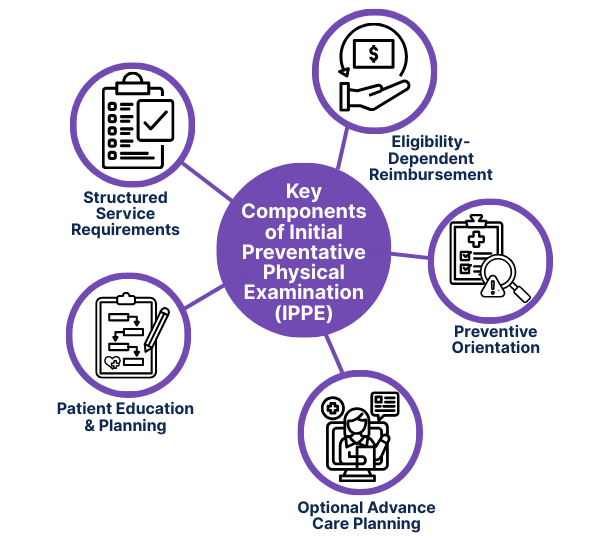
Key Components of the IPPE
The IPPE is built around prevention, education, and baseline documentation, rather than treatment. It differs from an annual wellness visit or physical exam in both scope and structure.
The core components include:
- Preventive Orientation: The visit is focused on identifying risks and planning future care—not diagnosing current complaints or chronic conditions.
- Structured Service Requirements: Medicare outlines specific services that must be included, from history taking to screening and counseling.
- Eligibility-Dependent Reimbursement: The IPPE is covered only once per beneficiary, and only within the first 12 months of Medicare Part B enrollment.
- Patient Education and Planning: A key outcome is a written prevention roadmap, which helps patients understand and access additional covered services.
- Optional Advance Care Planning: With patient consent, providers may also address end-of-life wishes, which is encouraged but not required.
Together, these components form the foundation of the IPPE’s value: Equipping new Medicare patients with preventive insight and care coordination from the start.
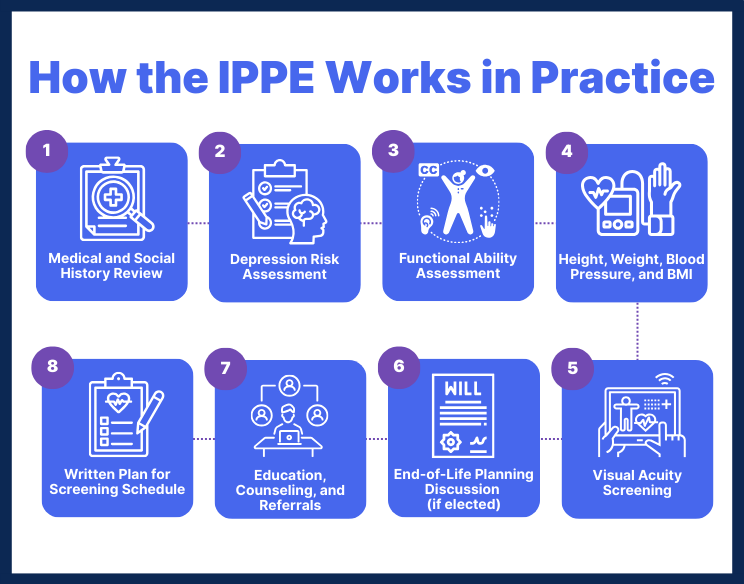
How the IPPE Works in Practice
The IPPE focuses on prevention, early detection, and care planning—not diagnosing or treating new problems. Medicare outlines specific elements that must be included in this visit to qualify for reimbursement:
1. Medical and Social History Review
Includes past illnesses, surgeries, hospital stays, current medications, lifestyle habits (e.g., tobacco/alcohol use), and family medical history.
2. Depression Risk Assessment
Evaluation for signs of depression using a validated screening tool or structured approach, with documentation of findings and next steps.
3. Functional Ability Assessment
Review of hearing, fall risk, activities of daily living (ADLs), home safety, and cognitive function (if relevant).
4. Height, Weight, Blood Pressure, and BMI
Basic biometric measurements must be recorded to assess physical health baseline.
5. Visual Acuity Screening
Simple screening to identify potential vision concerns that could impact daily function or safety.
6. End-of-Life Planning Discussion (if elected)
Includes conversation and documentation around advance directives, living wills, and patient preferences—only if the patient consents.
7. Education, Counseling, and Referrals
Based on risk factors uncovered during the exam, providers must offer personalized health advice and referrals for preventive services.
8. Written Plan for Screening Schedule
Delivery of a customized checklist outlining which preventive services the patient is eligible for, including timelines for follow-ups.
Eligibility and Timing for the IPPE
The IPPE is a time-sensitive, one-time benefit designed specifically for new Medicare beneficiaries. To qualify for reimbursement, patients and providers must meet the following criteria:
Who Is Eligible for an IPPE?
- Any patient enrolled in Medicare Part B
- Must be within their first 12 months of Part B coverage
- No previous IPPE billed under their Medicare record
This visit is not available to patients who have had Part B for more than a year, regardless of whether they previously saw a provider.
When Can an IPPE be Performed?
- Only once per lifetime
- Must occur within the first 12 months after enrolling in Medicare Part B
- Cannot be substituted or repeated as an Annual Wellness Visit (AWV)
What If a Patient Misses the Deadline for the IPPE?
If the 12-month window expires without the IPPE being completed, the patient loses eligibility permanently. They can, however, receive other Medicare-covered preventive services, including the AWV starting in their second year of Part B coverage.
Billing and Coding for the IPPE
Medicare allows providers to bill the IPPE as a covered preventive service—but only when all required components are completed and documented. Understanding the correct coding is critical for reimbursement and compliance.
Primary CPT Code for IPPE
- G0402 — Initial Preventive Physical Examination
This is the dedicated HCPCS code for the IPPE visit. It covers all core components, including history, screening, education, and planning. - Optional Add-On Codes (If Applicable)
If these services are performed and documented during the IPPE, they may be billed in addition:- G0403 – G0405 — ECG tracing, interpretation, and report (only if ordered and medically necessary)
- 99497 — Advance care planning (if the patient elects to discuss end-of-life preferences)
- G0468 — IPPE billed in a federally qualified health center (FQHC)
Note: These services must be clearly separate and medically necessary—and not bundled with the IPPE unless CMS guidelines allow.
IPPE Place of Service and Provider Type
- Eligible Providers include physicians (MD/DO), nurse practitioners, physician assistants, and clinical nurse specialists.
- IPPE can be conducted in physician offices, clinics, FQHCs, or RHCs, depending on the billing structure.
IPPE Cost to the Patient
When billed correctly, the IPPE is covered in full by Medicare Part B—meaning no deductible or coinsurance for the patient.
Frequently Asked Questions about the IPPE
1. Is the IPPE the same as an annual wellness visit?
No. The IPPE is a one-time visit offered during a patient’s first 12 months of Medicare Part B enrollment. The Annual Wellness Visit (AWV) is available annually starting in the second year and has different requirements.
2. What is the CPT code for the IPPE?
The IPPE is billed under HCPCS code G0402. Additional codes like G0403–G0405 (ECG) or 99497 (advance care planning) may be added if performed.
3. Can providers bill the IPPE and a problem-oriented E/M visit together?
Yes, but only if the problem-oriented service is medically necessary, separately documented, and billed with modifier -25. Routine findings or incidental discussions don’t justify a second code.
4. What happens if a patient misses the 12-month window?
They lose eligibility for the IPPE permanently. However, they may receive the Annual Wellness Visit starting in their second year of Part B coverage.
5. Can an RN perform the IPPE?
No. Only physicians, nurse practitioners, physician assistants, and clinical nurse specialists may perform and bill for the IPPE.
6. Is the IPPE free for patients?
Yes. When billed correctly, it is fully covered under Medicare Part B—no deductible or coinsurance applies.
