What is an HRA (Health Risk Assessment)?)
A Health Risk Assessment (HRA) is a structured questionnaire that collects patient-reported information about health status, medical history, behaviors, and social or functional risks. HRAs are used to identify clinical and non-clinical factors that may affect a person’s health outcomes, then guide preventive care, risk stratification, and care planning.
In healthcare operations, HRAs serve as an early-signal tool. They help providers detect gaps in care, surface safety or behavioral risks, and prioritize follow-up for patients who may need more support. HRAs are commonly used in primary care, care management programs, and value-based models where ongoing risk monitoring and proactive intervention are essential.
HRAs also play a formal role in certain preventive workflows, including Medicare Annual Wellness Visits, where an HRA is required to support a personalized prevention plan. But the use of HRAs extends beyond any single payer—they are broadly applied across population health, chronic care, and quality improvement settings to strengthen outcomes and continuity of care.
CMS requires an HRA for the Annual Wellness Visit and allows practices to use an HRA of their choice that covers the minimum CMS domains.
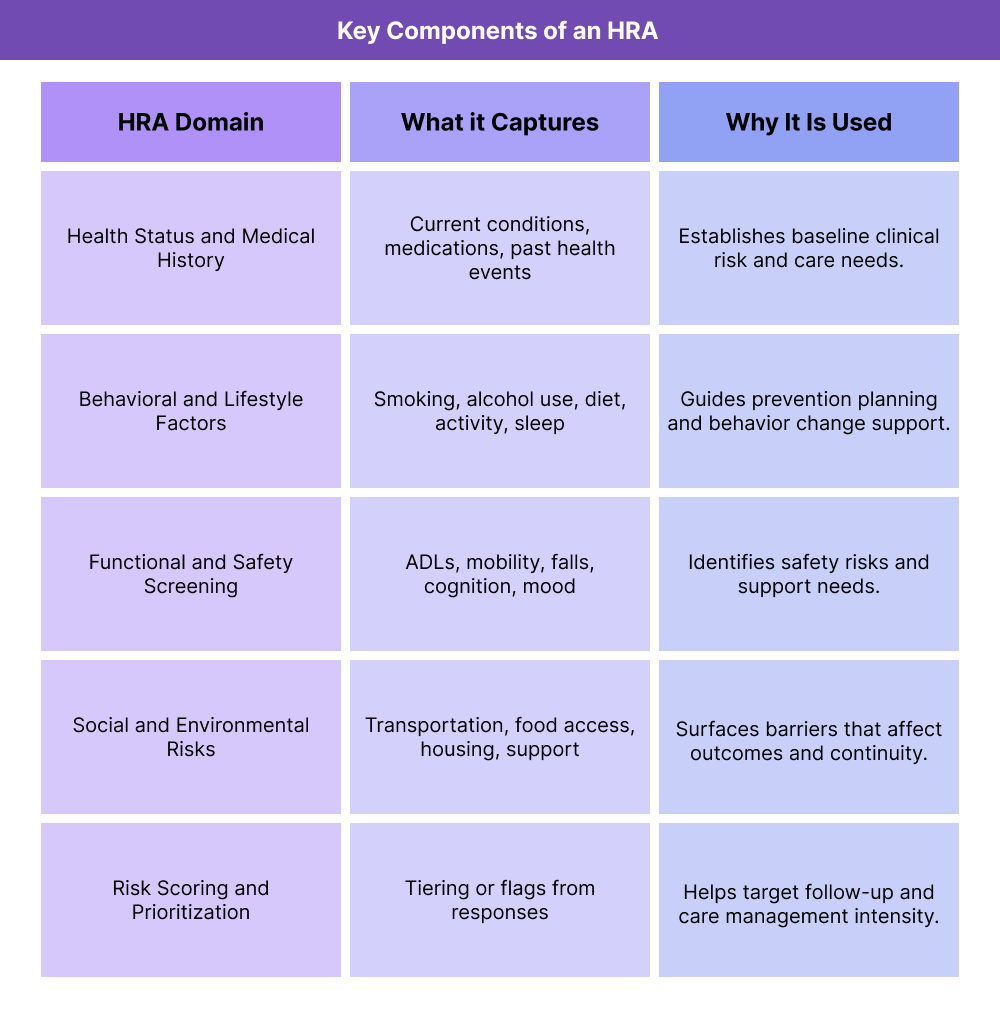
Key Components of an HRA
Health Risk Assessments are designed to capture patient-reported risks in a consistent, repeatable way so care teams can identify needs early and tailor prevention or care management plans. While HRAs can vary by organization or care model, they typically include a defined set of domains that align with clinical risk and functional realities.
Patient Health Status and Medical History
HRAs collect self-reported information about current conditions, prior diagnoses, surgeries, medications, and family health history. This helps care teams understand baseline risk and spot gaps that may require follow-up or documentation support.
Behavioral and Lifestyle Risk Factors
Most HRAs include questions about behaviors that influence outcomes, such as tobacco use, alcohol use, nutrition, physical activity, sleep, and fall risk. These inputs guide preventive counseling and help prioritize high-impact interventions.
Functional, Cognitive, and Safety Screening
HRAs often assess daily functioning, mobility, pain, memory concerns, depression risk, and home safety indicators. Identifying these issues early supports more accurate care planning and better continuity across clinical and non-clinical support services.
Social and Environmental Risk Drivers
Many HRAs now include social and environmental questions that affect a patient’s ability to maintain health, such as transportation access, food security, housing stability, or caregiver support. These risks are important for understanding why clinical plans may fail unless barriers are addressed.
Risk Scoring and Care Prioritization
Some HRAs include scoring or tiering logic that helps categorize patients by risk level. Even when scoring is not formalized, HRA results typically feed a broader risk stratification approach used in preventive care and care management workflows.
How HRA Works in Practice
Health Risk Assessments are used as a practical intake and risk-spotting tool that feeds prevention, care management, and quality workflows. While the exact format varies by organization, most HRAs follow a consistent operational cycle: collect patient-reported risks, translate results into priorities, and close the loop with follow-up actions.
Step 1: Administer the HRA
HRAs may be completed by patients before a visit, during an encounter with staff support, or through digital intake workflows. In a Medicare Annual Wellness Visit (AWV), CMS requires an HRA as part of the visit, and practices can use an HRA of their choice as long as minimum domains are covered. Many organizations also use HRAs outside AWVs for routine risk screening in primary care and care management programs.
Step 2: Review Responses for Risk Signals
Care teams review HRA results to identify clinical risks, functional or safety concerns, behavioral drivers, and social barriers that may affect outcomes. This allows the organization to flag which patients need deeper assessment or more intensive follow-up, even if they have not yet presented with an acute issue.
Step 3: Translate Results Into Risk Stratification and Care Planning
HRA findings often feed a broader risk stratification approach. Patients with higher risk indicators may be prioritized for care coordination, chronic disease follow-up, medication review, or referral to supportive services. In AWVs, HRA results help shape a personalized prevention plan.
Step 4: Close the Loop With Follow-Up and Documentation
Effective HRA workflows do not stop at identification. Organizations document the findings in the medical record and assign follow-up actions, such as preventive screenings, lifestyle counseling, safety interventions, or referrals for social support. Tracking whether these actions are completed is what turns HRA data into measurable care improvement.
HRA in Billing, Reimbursement, and System Limitations
An HRA is not a billable code by itself, but it is a required or enabling input for several reimbursable and compliance-sensitive workflows. Most notably, an HRA is a required component of the Medicare Annual Wellness Visit (AWV), and its findings often support risk adjustment, preventive care documentation, and care management targeting.
How HRA Supports Reimbursable Workflows
HRAs influence reimbursement by improving the accuracy and completeness of the clinical picture used for billing and payer evaluation. In practice, HRA results help providers:
- Document preventive needs and risk factors that support AWV delivery and personalization
- Identify conditions or risk drivers that should be addressed in the care plan and medical record
- Inform risk stratification used in longitudinal care programs such as Chronic Care Management
- Strengthen audit readiness by showing systematic risk screening and follow-up
When HRA findings are captured clearly and acted on, they reduce missed preventive opportunities and improve the defensibility of billed care management services.
HRA and Risk Documentation Quality
Many organizations use HRA outputs to surface conditions, functional risks, or social needs that may otherwise go undocumented. This improves documentation integrity by ensuring:
- Risks discussed with the patient are reflected in the record
- Care plans connect directly to identified barriers
- Follow-up actions are traceable to a documented need
- Better documentation reduces downstream billing friction and strengthens quality reporting.
- System Limitations and Operational Watch-Outs
Common limitations with HRAs usually come from workflow or data handling issues rather than the tool itself. These include:
- Treating the HRA as a checkbox without tying results to follow-up
- Collecting HRA data but not integrating it into the clinical record
- Using inconsistent questionnaires that make trend tracking difficult
- Failing to update HRAs regularly, causing risk profiles to go stale
- Capturing social or functional risks without having a pathway to address them
Technology can streamline HRA administration and tracking, but reimbursement value comes only when results drive documented care actions.
How HRAs Influence Quality, Access, and Equity in Healthcare
HRAs are a practical lever for improving outcomes because they surface risk early, identify care gaps before they escalate, and highlight barriers that patients may not otherwise disclose in a routine clinical encounter.
How HRA Improves Care Quality and Safety
HRAs strengthen quality by making risk detection systematic instead of incidental. When organizations use HRAs consistently, they can:
- Identify high-risk patients sooner
- Catch functional or safety issues like fall risk before harm occurs
- Detect behavioral or mental health risks that affect treatment success
- Improve care plan alignment with real patient needs
Over time, this leads to better preventive uptake, fewer avoidable escalations, and more consistent longitudinal care.
How HRA Supports Patient Access and Continuity
Access problems often show up as missed screenings, delayed follow-ups, or unaddressed barriers that keep patients from engaging in care. HRAs help by revealing why patients are not accessing care consistently and by triggering structured outreach or referrals.
This is especially useful for care management teams who need a repeatable way to decide which patients require additional continuity support.
Equity Benefits of HRA-Based Screening
HRAs can improve equity when they include social, environmental, and functional risk domains and when organizations review results across populations. This helps care teams identify patterns such as:
- Higher unmet needs in specific patient groups
- Disproportionate barriers to follow-up or preventive care
- Unequal access to transportation, nutrition, or support services
When improvement actions target these patterns, HRAs become a tool for reducing disparity-driven outcome gaps.
Frequently Asked Questions about HRAs
1. What is an HRA (Health Risk Assessment)?
A Health Risk Assessment (HRA) is a structured questionnaire that captures patient-reported health status, behavioral risks, functional concerns, and social factors so care teams can identify risk early and tailor preventive or care management plans.
2. Is an HRA required for Medicare Annual Wellness Visits?
Yes. An HRA is a required component of the Medicare Annual Wellness Visit (AWV). Practices can use an HRA of their choice as long as it covers the minimum CMS risk domains.
3. What kind of questions are included in an HRA?
HRAs typically include questions about current health conditions, medications, lifestyle behaviors, safety and fall risk, mood or cognition concerns, functional status, and social or environmental barriers that may affect care.
4. How is an HRA used in primary care?
In primary care, HRAs help detect emerging risks, guide preventive screening priorities, support risk stratification, and inform care plans or referrals before issues escalate.
5. How often should HRAs be updated?
HRAs should be updated regularly, especially for patients with changing health conditions or care needs. Many organizations refresh HRAs annually, and more frequently for higher-risk populations.
6. Does an HRA affect billing or reimbursement?
An HRA is not billable on its own, but it supports reimbursable workflows such as AWVs and care management by strengthening risk documentation, care planning, and audit readiness.
7. What is the difference between an HRA and risk stratification?
An HRA is the data collection tool that captures patient-reported risks. Risk stratification is the process of using HRA findings (plus clinical and claims data) to categorize patients by risk level and prioritize follow-up.
