What Is an HHA (Home Health Agency)?
A Home Health Agency (HHA) is a healthcare organization that provides skilled clinical services to patients in their homes. HHAs deliver services such as skilled nursing, physical therapy, occupational therapy, speech-language pathology, and medical social work—often for patients who are recovering from hospitalization, managing chronic conditions, or needing ongoing clinical support without facility-based care.
In Medicare, home health is a major part of the post-acute care continuum and is governed by specific coverage and documentation requirements. Home health services are intended to support patients who need skilled care at home and who meet eligibility criteria, including being under a physician’s plan of care and needing intermittent skilled services.
From an operational and business standpoint, HHAs are documentation-sensitive and compliance-driven. Payment depends on accurate eligibility determination, timely certification and recertification, and consistent clinical documentation that supports medical necessity. Because home health is frequently reviewed for program integrity, HHAs must maintain strong workflows for scheduling, care coordination, and audit readiness—especially for Medicare and Medicare Advantage populations.
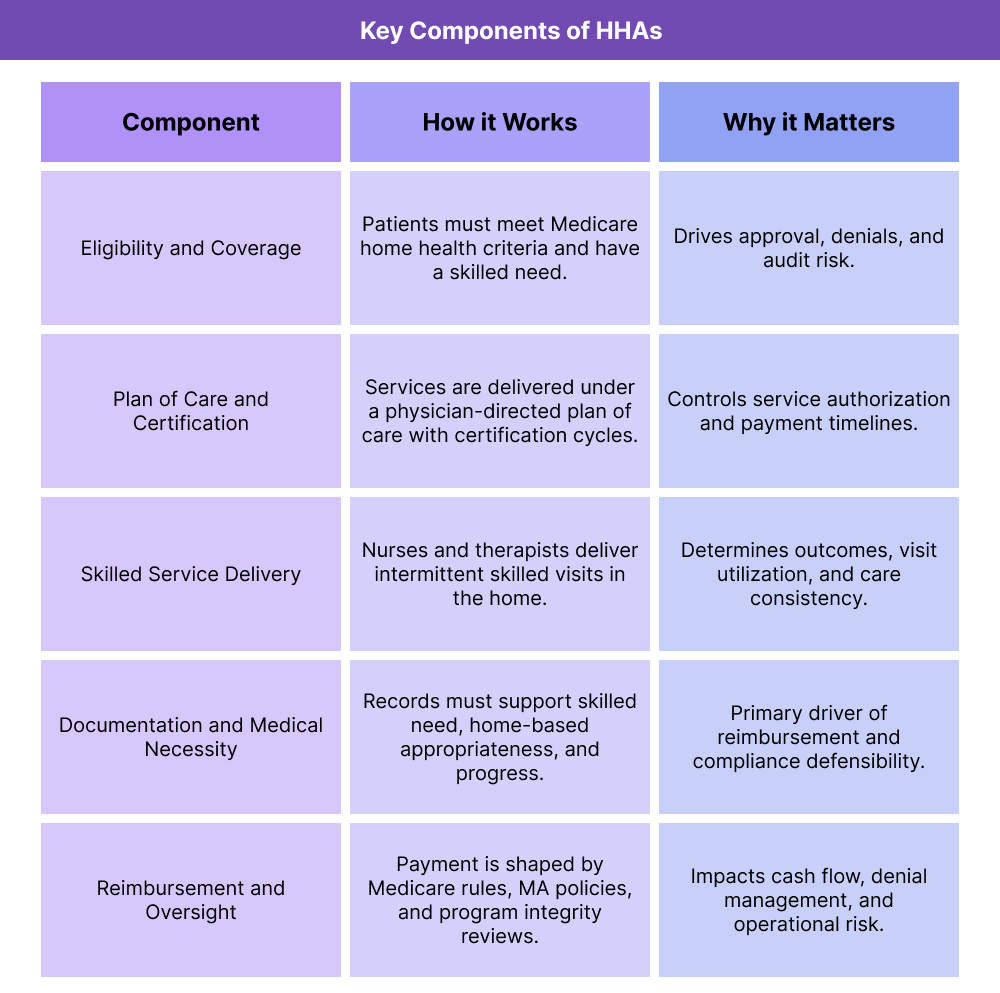
Key Components of HHAs
HHAs operate through a structured framework that ties together eligibility, physician oversight, service delivery, and reimbursement. These components shape how home health is delivered and how organizations manage risk, quality, and payment.
Medicare Home Health Eligibility and Coverage Requirements
Medicare home health coverage depends on defined eligibility criteria and the presence of a skilled need. Coverage decisions often hinge on:
- Whether the patient meets Medicare home health eligibility requirements
- Whether the services are skilled and medically necessary
- Whether care is intermittent and delivered under a physician-directed plan of care
- Whether documentation supports the clinical need for home-based services
In practice, eligibility determination is one of the biggest drivers of denials and audits, making front-end screening and documentation critical.
Home Health Plan of Care and Physician Certification
Home health services must be delivered under a formal plan of care established and reviewed by a physician or allowed practitioner. Certification and recertification workflows are central to home health operations because they establish medical oversight and authorize services over defined time periods.
This component is also a common operational bottleneck: delays in signatures, incomplete documentation, or misaligned certification timelines can create payment disruption.
Skilled Nursing and Therapy Services in Home Health
HHAs provide a mix of skilled services, including nursing visits and therapy sessions. Service delivery must match the plan of care and be documented consistently, including:
- Visit notes tied to measurable goals
- Progress toward clinical improvement or stabilization
- Patient response and ongoing skilled need
Because home health care is delivered in the community, scheduling logistics and workforce capacity also strongly influence service consistency and quality.
Home Health Documentation and Medical Necessity Standards
Home health reimbursement is documentation-driven. HHAs must clearly document:
- The patient’s condition and functional limitations
- Why skilled services are necessary
- Why the home setting is appropriate
- Ongoing need for skilled care and measurable progress
Documentation standards are closely tied to audit risk and FWA monitoring, especially when utilization is high or patterns appear inconsistent with clinical need.
Home Health Reimbursement, Oversight, and Program Integrity
Home health reimbursement is governed by Medicare payment structures and payer policies. Operationally, HHAs must manage:
- Coverage rules and payer edits
- Authorization requirements (especially in Medicare Advantage)
- Medical review and audit exposure
- Denials, appeals, and documentation remediation workflows
Home health is also frequently included in oversight and enforcement activity, creating a strong linkage to OIG priorities and broader compliance expectations.
How Home Health Agencies (HHAs) Work in Practice
Home Health Agencies (HHAs) operate as a core part of the post-acute and chronic-care continuum by delivering skilled care in the patient’s home. In practice, HHAs sit downstream of hospitals, IRFs, and SNFs and often serve Medicare and Medicare Advantage patients who need skilled clinical support but do not need facility-based care.
Because home health is highly documentation- and eligibility-driven, day-to-day success depends on aligning clinical workflows, certification timelines, and billing rules from the beginning of the episode.
Step 1: Referral Intake and Patient Eligibility Screening
Home health episodes often start with a referral—commonly from a hospital discharge planner, physician office, or post-acute facility. HHAs evaluate whether the patient is appropriate for home health and whether coverage criteria are likely to be met.
Key operational tasks include:
- Confirming payer coverage and benefits (Medicare FFS or Medicare Advantage)
- Verifying that services requested are skilled and intermittent
- Ensuring the home setting is safe and appropriate for care delivery
- Collecting documentation needed to support eligibility and medical necessity
- Identifying any DME needs that could affect home safety and outcomes
Early intake is where many downstream denials originate. If eligibility logic is weak at intake, the agency may deliver care that later fails medical review.
Step 2: Plan of Care Development and Physician Certification
Home health services must be delivered under a physician-directed plan of care. The agency develops the plan based on the referral information and initial assessment, then secures physician certification.
Operationally, this step requires:
- Creating a plan that matches skilled needs and realistic visit frequency
- Ensuring required certification documentation is complete
- Aligning start-of-care timing and service initiation with certification timelines
- Building a workflow to obtain timely physician signatures and updates
This is often one of the biggest operational bottlenecks. Delays in certification workflows create payment delays, rework, and avoidable compliance exposure.
Step 3: Start of Care and Skilled Service Delivery in the Home
Once the episode begins, nurses and therapists deliver skilled services in the home. In practice, this includes:
- Skilled nursing visits (assessment, medication management, wound care, education)
- Therapy services (PT, OT, SLP) tied to functional goals
- Social work support where applicable
- Ongoing assessment of safety, adherence, and barriers to care
Because home health is delivered in the community, staff scheduling, geography, and workforce availability strongly influence service consistency. Missed visits and inconsistent sequencing can also weaken documentation narratives around medical necessity and progress.
Step 4: Documentation, Progress Tracking, and Care Coordination
Home health is documentation-driven. Each visit must support why skilled care is needed and demonstrate progress, stabilization, or clinical complexity requiring ongoing skilled oversight.
Operationally, agencies must:
- Document visit content with clear skilled rationale
- Track progress against measurable goals
- Adjust the plan of care as the patient improves or needs change
- Coordinate with physicians and referring providers on updates
- Identify escalation needs (ED risk, deterioration, medication issues)
This is where home health intersects with program integrity and FWA monitoring. Utilization patterns that are not well-documented can trigger reviews, even when care is clinically appropriate.
Step 5: Recertification, Discharge Planning, and Transitions of Care
Home health is episodic by nature. As the patient progresses, agencies either discharge the patient or recertify the plan of care when ongoing skilled need exists.
This step includes:
- Recertification documentation and physician approval
- Discharge planning and patient education
- Transition back to primary care, specialists, or outpatient therapy
- Coordination of long-term supports if needed
Strong discharge planning reduces readmissions and supports continuity—especially for high-risk Medicare populations.
HHAs in Billing, Reimbursement, and System Limitations
HHAs operate in one of the most compliance-sensitive reimbursement environments in healthcare. Payment is closely tied to eligibility, certification workflows, and documentation that supports skilled need and medical necessity.
How Home Health Billing and Reimbursement Works in Medicare
In Medicare home health, reimbursement is structured around defined episodes of care and clinical documentation rather than line-by-line billing for every service. This makes front-end accuracy and mid-episode documentation essential.
Operational drivers of reimbursement commonly include:
- Correct episode timing and coverage alignment
- Timely and complete physician certification and recertification
- Clinical documentation that supports skilled need and progress
- Payer-specific requirements (often stricter in Medicare Advantage)
Because reimbursement is tied to compliance, HHAs often invest heavily in documentation processes and internal QA to reduce denial risk.
Medicare Advantage Authorization and Policy Variability for Home Health
Medicare Advantage organizations (MAOs) frequently impose additional requirements beyond Medicare’s baseline rules, including:
- Prior authorization for home health episodes or specific services
- Network restrictions that affect referral routing
- More granular documentation or utilization review requirements
- Additional reviews for high utilization or long episode duration
This variability creates operational complexity. HHAs must often manage payer-by-payer workflows and maintain clear documentation narratives that satisfy different review standards.
Home Health Documentation Requirements and Program Integrity Risk
Home health denials and audits frequently hinge on documentation. Common risk areas include:
- Documentation that describes tasks but not skilled need
- Progress notes that lack measurable improvement or rationale for ongoing services
- Plan of care inconsistencies across disciplines
- Late or incomplete physician signatures
- Episode patterns that appear repetitive without clinical change
Because home health is often reviewed for program integrity, agencies need consistent templates and a strong clinical documentation culture.
System Limitations and Common Home Health Operational Challenges
Home health agencies routinely face system-level constraints that affect reimbursement and quality:
- Workforce shortages, leading to delayed starts of care or missed visits
- Fragmented documentation systems, especially across disciplines
- Physician coordination challenges, including slow signature turnaround
- Payer variability, creating admin burden and rework
- Limited interoperability with hospital and primary care systems, reducing continuity
These limitations increase the importance of standardized workflows and proactive denial prevention programs.
How HHAs Influence Quality, Access, and Equity in Healthcare
Home health is a critical access layer for patients who struggle to attend clinic visits due to mobility, transportation barriers, or clinical fragility. HHAs often determine whether patients recover safely at home or cycle back into hospitals.
Home Health Quality Outcomes and Readmission Prevention
High-quality home health can reduce preventable readmissions by:
- Catching complications early
- Improving medication adherence and education
- Supporting wound care and post-surgical recovery
- Coordinating follow-up with physicians and specialists
- Identifying social barriers affecting recovery
Quality in home health often depends on timely start of care, consistent visit delivery, and effective transitions after discharge.
Home Health Access Challenges for Medicare Patients
Access to home health is not uniform. Barriers often include:
- Limited agency capacity in rural or underserved areas
- Workforce shortages for nursing and therapy disciplines
- Payer restrictions, especially in Medicare Advantage networks
- Administrative barriers in authorization and intake processes
When capacity is limited, patients may face delays in starting services—raising risk of complications and hospital returns.
Equity Implications of Home Health Delivery
Home health can reduce inequities by bringing care to patients who face barriers to traditional access. But equity challenges still exist, including:
- Housing instability or unsafe home environments
- Language and health literacy barriers
- Limited caregiver support
- Technology gaps affecting remote monitoring or communication
- Geographic disparities in provider supply
Equity-centered home health operations often include culturally appropriate education, strong care navigation, and coordination with community resources to address barriers beyond clinical need.
Frequently Asked Questions about HHAs
1. What is an HHA (Home Health Agency) in healthcare?
A Home Health Agency (HHA) is a healthcare organization that provides skilled clinical services to patients in their homes. HHAs commonly deliver skilled nursing and therapy services under a physician’s plan of care and are a key part of Medicare post-acute care.
2. What services do Home Health Agencies provide for Medicare patients?
HHAs may provide skilled nursing, physical therapy, occupational therapy, speech-language pathology, and medical social work, depending on the patient’s needs and plan of care. Services must be medically necessary and documented to support coverage and reimbursement.
3. What are Medicare home health eligibility requirements for HHA services?
Medicare home health coverage generally requires that the patient needs intermittent skilled services, is under a physician-directed plan of care, and meets Medicare’s coverage criteria. Eligibility is documentation-sensitive, and incomplete records are a common cause of denials.
4. What is the home health plan of care and why is physician certification important?
Home health services must be delivered under a formal plan of care that is certified and periodically recertified by a physician or allowed practitioner. Certification is essential because it authorizes services and establishes medical oversight for the home health episode.
5. How do Medicare Advantage plans affect HHA authorization and coverage?
Medicare Advantage organizations (MAOs) often require prior authorization for home health services and may apply additional utilization management rules. HHAs typically need payer-specific workflows and strong medical necessity documentation to avoid delays and denials.
6. What documentation is required for Home Health Agency billing and reimbursement?
HHA documentation must support medical necessity, skilled need, the plan of care, and patient progress. Visit notes should clearly explain why skilled services are required and demonstrate measurable improvement, stabilization, or complexity that justifies continued skilled care.
7. Why is home health considered high-risk for audits and program integrity reviews?
Home health is frequently reviewed because reimbursement depends heavily on eligibility and documentation rather than visible facility-based services. Patterns such as high utilization, long episodes, or weak progress narratives can trigger audits and FWA monitoring.
8. How do HHAs help reduce hospital readmissions and improve outcomes?
HHAs can reduce readmissions by monitoring patients after discharge, supporting medication management, detecting complications early, providing therapy to restore function, and coordinating follow-up care with physicians and specialists.
9. What are common operational challenges for Home Health Agencies?
Common challenges include workforce shortages, delayed starts of care, fragmented documentation across disciplines, slow physician signature turnaround, payer variability (especially in MA plans), and limited interoperability with hospital and primary care systems.
