What is a Federally Qualified Health Center (FQHC)?
A Federally Qualified Health Center (FQHC) is a community-based healthcare provider that receives federal funding to deliver primary care services in underserved areas. FQHCs offer care to patients regardless of their ability to pay and operate on a sliding fee scale based on income.
Recognized by the Health Resources and Services Administration (HRSA), FQHCs serve as a safety net for medically underserved communities — including rural populations, low-income individuals, and the uninsured. The term FQHC also appears frequently in Medicare and Medicaid billing guidance, particularly in reference to reimbursement rules, scope of practice, and provider qualifications.
Key Components of a Federally Qualified Health Center
- Must be designated by HRSA and meet federal guidelines
- Provides comprehensive primary care, including preventive, dental, mental health, and substance use services
- Operates under a sliding fee scale based on patient income
- Serves medically underserved populations, including rural and urban communities
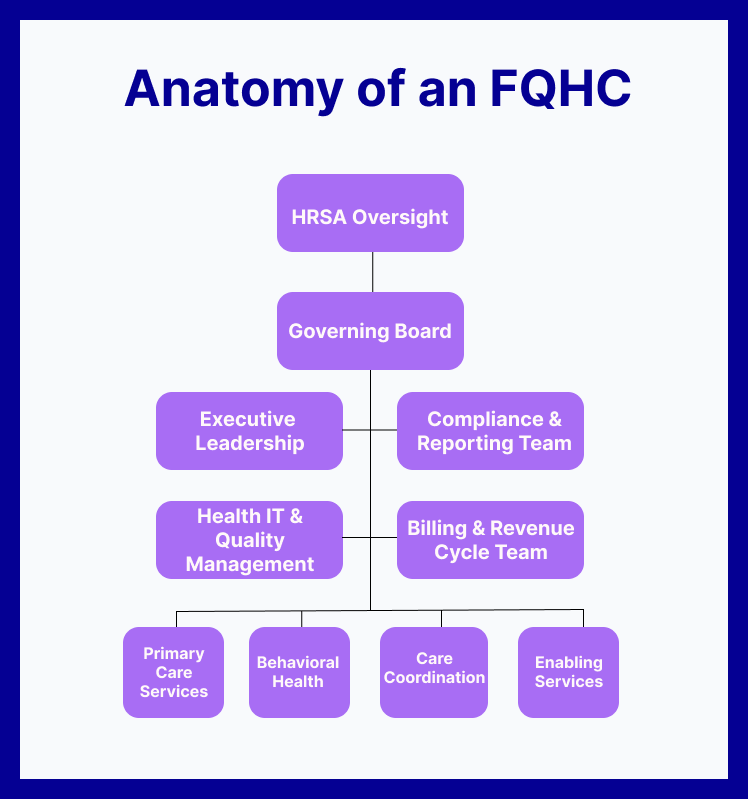
- Required to have a governing board with majority patient representation
- Eligible to receive enhanced Medicare/Medicaid reimbursement rates and participate in federal programs (e.g., 340B Drug Pricing)
How FQHCs Work in Practice
Federally Qualified Health Centers (FQHCs) operate as full-service healthcare providers that deliver comprehensive, community-based care to medically underserved populations. Unlike traditional private practices, FQHCs are structured to meet federal access and equity standards, and they follow specific requirements to maintain their funding and designation.
Common FQHC Features in Day-to-Day Operations:
-
Provide integrated care: primary care, dental, behavioral health, preventive services, and often specialty referrals
-
Use sliding fee scales to reduce financial barriers for uninsured or low-income patients
-
Serve as essential care access points in rural areas, inner cities, and high-need communities
-
Employ multidisciplinary care teams, including physicians, nurse practitioners, social workers, and care coordinators
-
Participate in value-based programs like Chronic Care Management (CCM), CoCM, and Medicaid managed care
-
Report quality metrics to HRSA and undergo routine compliance reviews
FQHCs may operate multiple service sites, including school-based health centers, mobile clinics, or satellite offices — but all locations must align with HRSA standards.
Benefits and Challenges of FQHCs
Benefits of FQHCs
-
Expanded Access to Care: Serve as critical safety nets for low-income, rural, and marginalized populations
-
Sliding Fee Scale: Offers affordable services based on patient income
-
Integrated Care Model: Combines primary care, behavioral health, dental, and support services under one roof
-
Enhanced Reimbursement Rates: Receive Prospective Payment System (PPS) rates under Medicare and Medicaid
-
Eligibility for Federal Support: Access to 340B drug pricing, HRSA grant funding, and malpractice protection (FTCA)
-
Community Representation: Patient-majority governing boards ensure local needs guide services
Challenges of FQHCs
-
Heavy Regulatory Burden: Must meet strict HRSA and Uniform Data System (UDS) reporting requirements
-
Workforce Shortages: Often face recruitment and retention issues for physicians and behavioral health staff
-
Complex Billing Environment: Navigating enhanced Medicaid/Medicare rules, grants, and sliding fee income
-
Funding Volatility: Dependent on continued federal appropriations and performance metrics
-
Technology & Compliance Gaps: Many FQHCs struggle with health IT, EHR integration, or quality reporting infrastructure
-
Burnout Risk: High patient volumes and social determinants of health complexity increase strain on care teams
How Federally Qualified Health Centers Are Reimbursed
Federally Qualified Health Centers (FQHCs) follow a unique billing model that differs significantly from standard fee-for-service (FFS) providers. Instead of billing individual CPT codes for most encounters, FQHCs are reimbursed through the Prospective Payment System (PPS) — a bundled, per-visit rate set by CMS.
Key Billing Characteristics of FQHCs:
-
Medicare FQHC PPS Rate: Covers medically necessary, face-to-face visits by QHPs; updated annually by CMS
-
Medicaid Reimbursement: States may follow PPS or use Alternative Payment Methodologies (APMs)
-
Sliding Fee Adjustments: Patients are charged based on income and family size per federal guidelines
-
Wraparound Payments: In some cases, FQHCs receive additional payments to supplement managed care reimbursements
Important to Note:
-
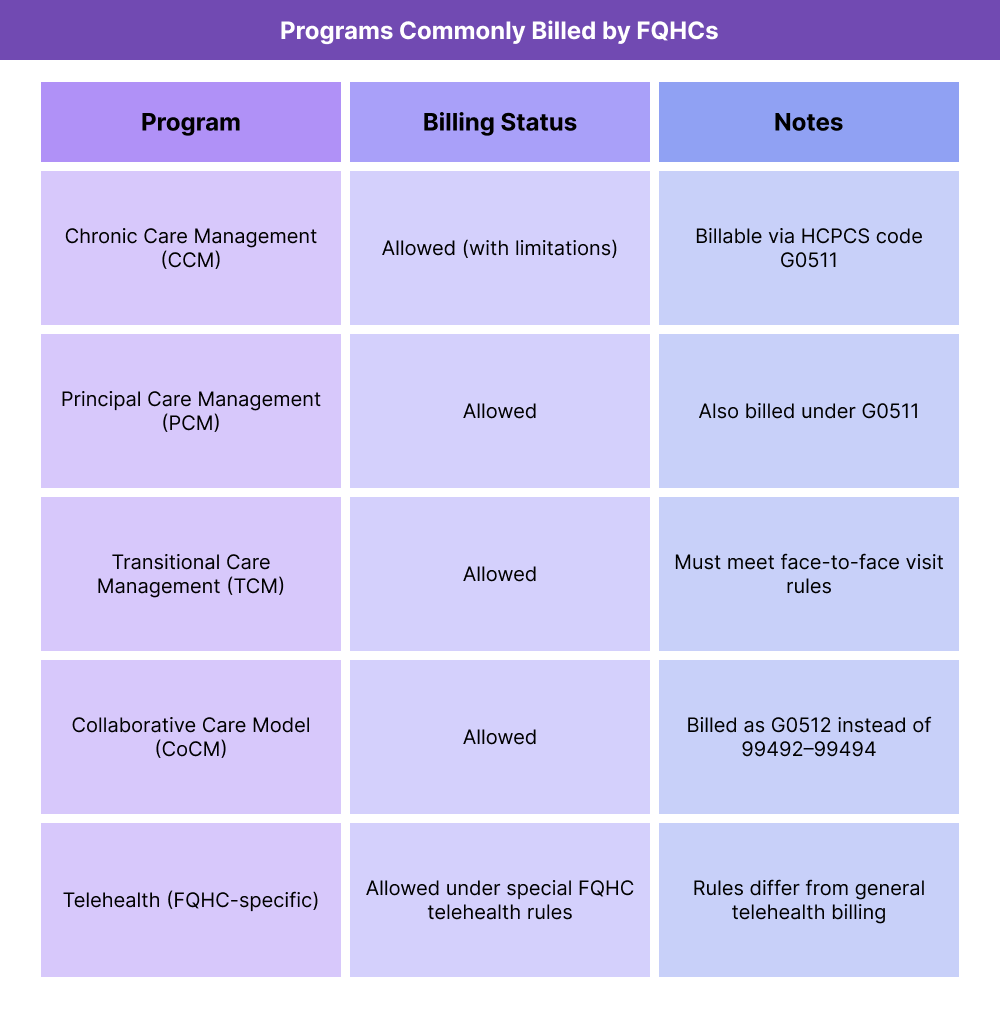
FQHCs cannot bill most standard CPT codes directly (e.g., 99490 for CCM) — instead, they use HCPCS G-codes designed for bundled service types.
-
All billing must be tied to a qualified visit and conducted by or under the supervision of a Qualified Health Professional (QHP).
-
CMS and Medicaid billing rules for FQHCs are program-specific and often differ by state.
Frequently Asked Questions about FQHCs
1. What is an FQHC?
A Federally Qualified Health Center (FQHC) is a community-based healthcare provider that receives federal funding to offer primary care services in underserved areas. FQHCs serve patients regardless of ability to pay and operate on a sliding fee scale.
2. How does an FQHC differ from a regular health center?
Unlike private clinics or hospitals, FQHCs must meet HRSA designation criteria, serve medically underserved populations, and report specific quality and compliance data. They also receive enhanced Medicare and Medicaid reimbursement rates.
3. What services do FQHCs provide?
FQHCs offer a wide range of services, including:
- Primary care
- Behavioral health
- Dental care
- Preventive screenings
- Care coordination
- Enabling services like translation or transportation
4. Can FQHCs bill for Chronic Care Management or CoCM?
Yes. FQHCs can bill for Chronic Care Management (CCM) and Collaborative Care Model (CoCM) services, but must use HCPCS codes G0511 and G0512 instead of standard CPT codes like 99490 or 99492–99494.
5. What is the difference between an FQHC and a Look-Alike?
An FQHC Look-Alike meets most of the same requirements as a full FQHC but does not receive Section 330 grant funding. Look-Alikes still qualify for enhanced Medicaid and Medicare payments but miss out on other benefits like malpractice coverage under the Federal Tort Claims Act (FTCA).
