What is Fee-for-Service (FFS) in Healthcare?
Fee-for-Service (FFS) is a traditional healthcare reimbursement model in which providers are paid separately for each individual service or procedure performed. Rather than receiving a bundled or outcome-based payment, clinicians bill for every appointment, test, treatment, or consultation—often using CPT or HCPCS codes to itemize services.
This model has historically dominated U.S. healthcare, especially in Medicare Part B, private commercial insurance, and early Medicaid programs. While straightforward and widely adopted, Fee-for-Service has drawn criticism for promoting volume over value—encouraging more frequent services rather than better patient outcomes.
Today, FFS is still used across many care settings, but it’s increasingly being blended with or replaced by value-based care models, especially in programs focused on chronic care, care coordination, and preventative services.
Key Components of the Fee-for-Service Model
Fee-for-Service (FFS) operates on a simple transactional basis: each medical service rendered generates a billable charge. This makes it easy to administer but can create incentives for overutilization or fragmented care. Below are the core components that define how FFS works:
- Itemized Billing: Each individual action—such as a patient evaluation, lab test, x-ray, or follow-up—is billed separately. Providers submit these itemized charges using standardized codes (e.g., CPT, HCPCS).
- Unbundled Payments: Unlike bundled payments or episode-based care, FFS treats each service as a discrete reimbursable unit, regardless of how related services are delivered or sequenced.
- Retrospective Reimbursement: Payers (e.g., Medicare, Medicaid, commercial insurers) reimburse providers after services are rendered and claims are processed. There is no up-front capitated amount.
- Minimal Outcome Linkage: Payment is not directly tied to whether care improved the patient’s condition, only that a qualifying service was delivered and documented properly.
- Billing Based on Volume: The more procedures or encounters documented, the higher the reimbursement—regardless of efficiency or patient satisfaction.
This model offers clarity and predictability for providers but often fails to reward coordination, preventative efforts, or long-term disease management—areas where alternative payment models are gaining ground.
Pros & Cons of Fee For Service
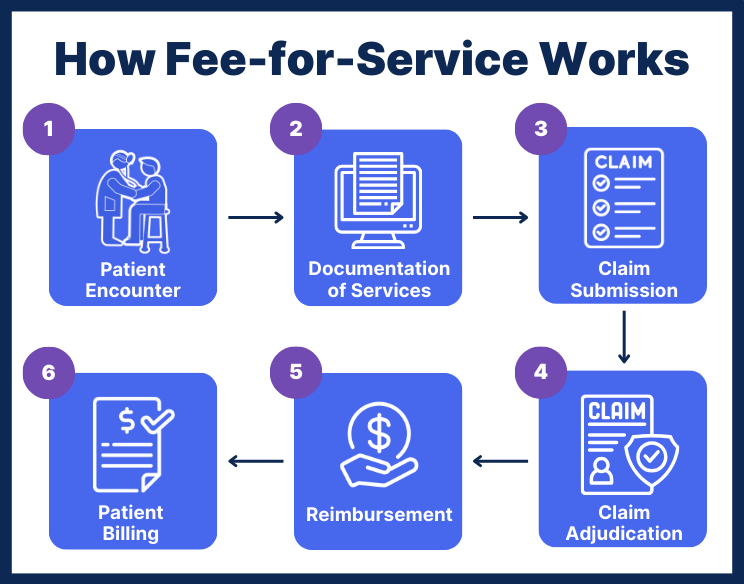
How Fee for Service Works in Practice
In a typical Fee-for-Service environment, the billing and reimbursement process follows a clear, linear progression. While details may vary slightly by payer (e.g., Medicare vs. private insurance), most workflows involve the following steps:
1. Patient Encounter
A patient receives medical care—this could be a routine office visit, lab draw, specialist consultation, or a diagnostic service like an X-ray.
2. Documentation of Services
The provider documents all services rendered, including clinical notes, diagnosis codes (ICD-10), and procedure codes (CPT/HCPCS). These become the basis for the bill.
3. Claim Submission
The provider’s billing department or EHR system generates a claim and submits it to the payer. Claims must meet CMS or payer-specific requirements for coding, timing, and justification.
4. Claim Adjudication
The payer reviews the claim, checking it for accuracy, coverage, and medical necessity. They approve or deny reimbursement based on internal policies and fee schedules.
5. Reimbursement
If approved, the payer reimburses the provider for each billable unit (e.g., office visit, lab test) according to a predetermined rate. Payment is typically made within 30–60 days.
6. Patient Billing (if applicable)
If the service isn’t fully covered or is subject to co-insurance or deductibles, the provider may bill the patient for the balance.
This structure makes billing volume-sensitive, with no cap on the number of reimbursable services per patient or per month—unless explicitly restricted by the payer.
Fee-for-Service and Medicare
Medicare Fee-for-Service (FFS) remains one of the most prominent examples of this payment model in the U.S. healthcare system. Often referred to as Original Medicare, this structure reimburses providers based on a fee schedule that correlates directly with the number and type of services delivered.
Where It Still Applies
- Part B Outpatient Services: Routine office visits, diagnostic tests, and chronic condition management.
- Provider Types: Physicians, nurse practitioners, clinical psychologists, and other qualified health professionals.
- Billing Codes: Services must be submitted with valid CPT/HCPCS codes and often require a corresponding ICD-10 diagnosis.
FFS in Chronic Care Management (CCM)
While newer care management programs (e.g., CCM, BHI, CoCM) incorporate value-based goals, they still rely on the FFS billing structure to reimburse providers for time-based care delivered to patients with chronic conditions.
Reimbursement Characteristics
- Timely Filing Rules: Claims typically must be submitted within 12 months of service.
- Fee Schedules: CMS publishes annual updates to payment rates based on national conversion factors and relative value units (RVUs).
Even as Accountable Care Organizations (ACOs) and alternative payment models (APMs) gain traction, Medicare FFS remains the default reimbursement model for millions of providers and patients—especially in rural or solo practice environments.
Fee-for-Service vs. Value-Based Care
As healthcare costs rise and outcomes stagnate, many payers—including CMS—are moving away from Fee-for-Service (FFS) and toward value-based care (VBC) models that reward outcomes, coordination, and efficiency.
In practice, many healthcare organizations now operate in a hybrid model—receiving some revenue through FFS while participating in value-based initiatives such as MIPS, ACOs, or chronic care coordination programs. Understanding how FFS works is still critical, even as the system evolves.

Frequently Asked Questions about Fee-for-Service
1. What does "Fee-for-Service" mean in healthcare?
Fee-for-Service (FFS) refers to a payment model where healthcare providers are reimbursed for each individual service or procedure performed, rather than for overall care quality or patient outcomes.
2. Is Fee-for-Service still used in Medicare?
Yes. Original Medicare still operates largely under a Fee-for-Service structure, particularly for outpatient services under Part B. Providers bill for each qualifying service using CPT or HCPCS codes.
3. How does Fee-for-Service impact care delivery?
Because FFS links payment to volume, it can encourage overutilization of services and discourage coordination. However, it also allows providers flexibility in offering care without bundling restrictions.
4. What's the difference between Fee-for-Service and Value-Based Care?
Fee-for-Service rewards quantity—more services lead to more reimbursement. Value-Based Care, by contrast, ties payment to patient outcomes, quality benchmarks, and cost-efficiency.
5. Can Fee-for-Service be used in Chronic Care Management programs?
Yes. Many Medicare care management programs, such as Chronic Care Management (CCM) and Behavioral Health Integration (BHI), are billed using the FFS model but incorporate value-based principles.
6. Why is Fee-for-Service being phased out in some settings?
Because FFS doesn’t reward efficiency or improved outcomes, it’s gradually being supplemented or replaced by models that promote accountability, care coordination, and long-term patient value.
