What are CTBS (Care Team-Based Services) in Healthcare?
Care Team-Based Services (CTBS) refer to a group of non–face-to-face, technology-enabled clinical services that can be provided by a physician or qualified healthcare professional with the help of clinical staff under general supervision. CTBS codes were developed by CMS (Centers for Medicare & Medicaid Services) to recognize and reimburse the collaborative work performed by care teams in support of remote monitoring, chronic care management, and patient engagement.
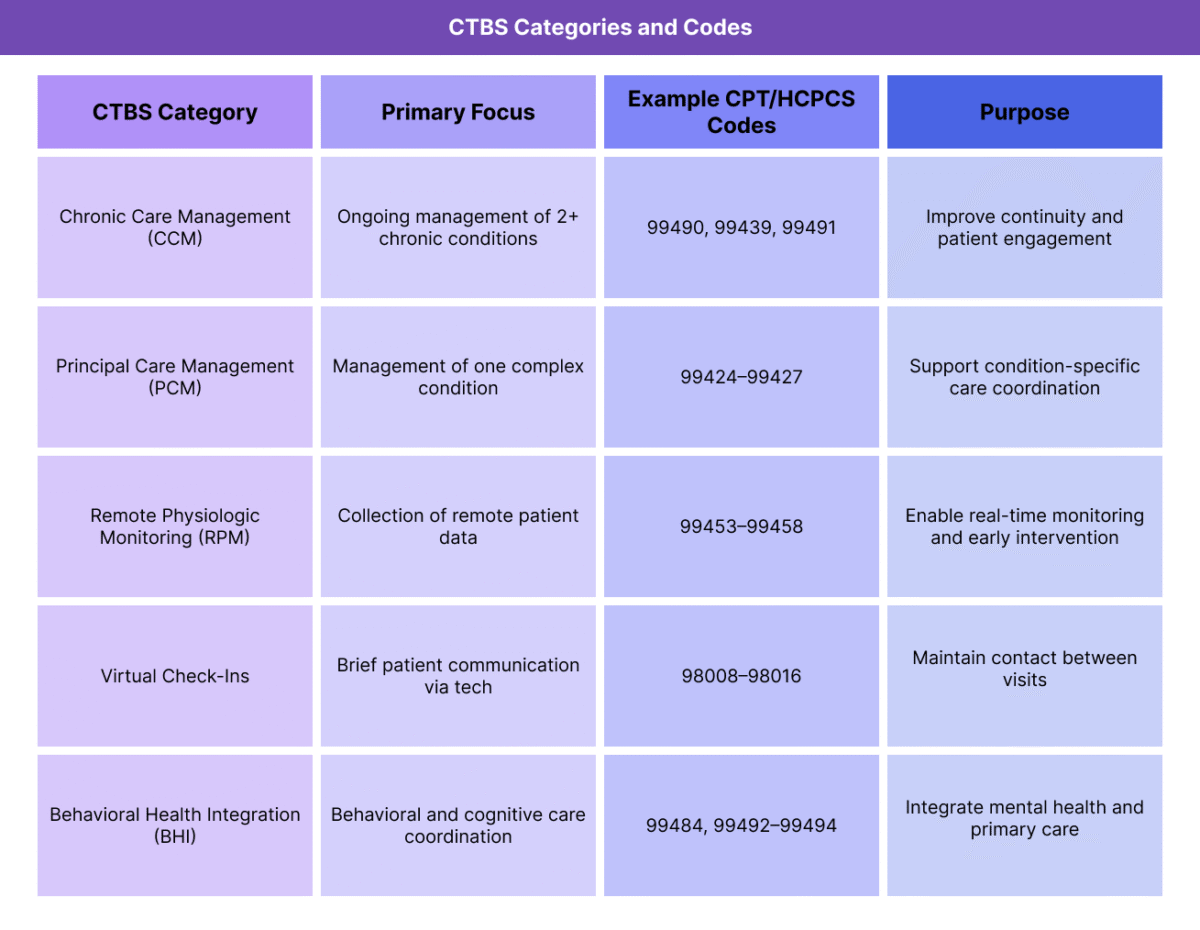
CTBS encompass several service types, including Chronic Care Management (CCM), Principal Care Management (PCM), Remote Physiologic Monitoring (RPM), and Virtual Check-Ins, among others. They allow physicians and clinical staff—such as nurses, medical assistants, and care coordinators—to deliver ongoing care between in-person visits, enhancing continuity, access, and patient outcomes.
From a billing standpoint, CTBS codes bridge the gap between traditional evaluation and management (E/M) visits and virtual care delivery models. They enable providers to document and receive reimbursement for time spent on coordination, communication, and follow-up activities that are essential to Value-Based Care but often go uncompensated in fee-for-service environments.
Key Components of Care Team-Based Services (CTBS)
Care Team-Based Services (CTBS) include a set of non–face-to-face, time-based services that recognize the collaborative work of healthcare teams in managing patient care outside traditional office visits. These services are billable when performed by clinical staff under general supervision of a physician or qualified healthcare professional, meaning the provider does not need to be physically present while the care team delivers the service.
CTBS codes align with CMS’s broader goal of expanding access, promoting care continuity, and compensating interdisciplinary work that supports patients with chronic or complex conditions.
Chronic Care Management (CCM)
- Focuses on ongoing management of patients with two or more chronic conditions.
- Includes structured care plans, patient follow-up, and coordination with other providers.
- CPT examples: 99490, 99439, 99491, 99437.
Principal Care Management (PCM)
- Designed for patients with a single serious or complex chronic condition.
- Recognizes management of that condition by the primary or specialist provider.
- CPT examples: 99424–99427.
Remote Physiologic Monitoring (RPM)
- Covers collection and interpretation of physiologic data (e.g., blood pressure, glucose, weight) from connected devices.
- CPT examples: 99453, 99454, 99457, 99458.
Virtual Communication and Check-Ins
- Includes brief, technology-enabled interactions between the patient and provider (e.g., phone, video, portal message).
- CPT and HCPCS examples: G2010, G2012, 98970–98972 (legacy); 98008–98016 (new CTBS communication codes introduced for 2024–2025).
Behavioral and Cognitive Support Services
- Some CTBS codes also extend to behavioral health integration (BHI) and cognitive assessment interventions.
- Supports care models that combine physical and mental health management.
How Care Team-Based Services (CTBS) Work in Practice
Care Team-Based Services (CTBS) are designed to operationalize collaborative, ongoing care delivery between office visits. These services recognize the time and effort clinical teams spend monitoring, communicating with, and supporting patients — especially those with chronic or complex conditions.
The workflow for CTBS typically follows a five-step process, from patient enrollment through documentation and billing.
Step 1: Identify and Enroll Eligible Patients
- Patients qualify for CTBS when they have chronic or serious conditions that require ongoing management outside of in-person visits.
- Providers must obtain verbal or written consent before initiating CTBS, informing patients of program details, copayments, and opt-out rights.
- Enrollment is usually tracked in the EHR and confirmed monthly for billing eligibility.
Step 2: Care Planning and Coordination
- The care team creates or updates a comprehensive care plan, documenting diagnoses, medications, treatment goals, and self-management instructions.
- Team members coordinate across specialists, pharmacies, and community resources, ensuring all care decisions are documented.
- These interactions form the foundation for billable time under CCM, PCM, or related CTBS categories.
Step 3: Service Delivery and Patient Engagement
- Clinical staff provide non–face-to-face services such as follow-up calls, medication checks, vital sign review, and patient education.
- For RPM and virtual communication codes, data from connected devices or digital tools are monitored and interpreted regularly.
- Providers supervise under general supervision, meaning care team members may deliver services independently while the physician remains accountable.
Step 4: Documentation and Time Tracking
- Each CTBS service must be documented in the EHR, including total time spent, personnel involved, and activities performed.
- Time-based thresholds vary by code (e.g., 20, 30, or 60 minutes).
- Accurate documentation ensures compliance with CMS and commercial payer requirements.
Step 5: Billing and Reimbursement
- Once monthly activity thresholds are met, the appropriate CPT or HCPCS code is billed.
- Claims include the supervising provider’s NPI, even if care team members performed the majority of the work.
- CTBS reimbursement is typically per patient per month, making it a predictable revenue stream that supports population health management.
CTBS in Billing, Reimbursement, and Compliance Limitations
Care Team-Based Services (CTBS) are reimbursable under Medicare Part B and, increasingly, through commercial payers adopting value-based and remote care models. These services bridge the gap between traditional evaluation and management (E/M) encounters and continuous virtual care, allowing providers to receive payment for the work of clinical teams in between patient visits.
Billing and Reimbursement Structure
- CTBS codes are typically billed on a monthly, time-based cycle per enrolled patient.
- Each service category (CCM, PCM, RPM, etc.) has its own minimum time thresholds — most commonly 20, 30, or 60 minutes per month.
- The claim is billed under the supervising physician or qualified health professional’s National Provider Identifier (NPI), even though much of the work may be completed by clinical staff under general supervision.
- Only one provider or organization may bill for the same CTBS category per patient per month.
Supervision Requirements
- Most CTBS codes allow general supervision, meaning the supervising provider does not need to be physically present.
- Some services, like RPM and behavioral health integration (BHI), can also be performed “incident to” a physician’s service under remote supervision guidelines.
- Clear documentation of roles, tasks, and oversight is required to maintain compliance.
Reimbursement Considerations
- Payment amounts vary by service type and total time billed, adjusted by the RBRVS formula (RVUs × GPCI × Conversion Factor).
- Medicare updates CTBS reimbursement rates annually in the Medicare Physician Fee Schedule (MPFS).
- Many commercial payers mirror CMS policies but may require specific modifiers or prior authorization for virtual or asynchronous care.
Common Limitations and Challenges
- Documentation Burden: Tracking time, activities, and staff contributions can be administratively heavy, especially without automated EHR workflows.
- Overlap Rules: CTBS codes cannot overlap in time with other time-based services (e.g., CCM and TCM billed concurrently).
- Patient Awareness: Some patients decline enrollment due to copays or lack of understanding about ongoing virtual services.
- Payer Variability: Coverage and payment for new codes (98008–98016) are still inconsistent across commercial plans as of 2025.
CTBS and Its Impact on Quality, Access, and Equity in Healthcare
Care Team-Based Services (CTBS) were designed to address gaps in traditional healthcare delivery by expanding how, when, and by whom patient care is provided. By reimbursing non–face-to-face services, CTBS directly supports care continuity, patient engagement, and health equity across diverse populations — particularly those managing chronic conditions or limited by geography.
Improving Care Quality and Continuity
- CTBS programs foster continuous engagement between patients and care teams, improving adherence to treatment plans and early identification of clinical issues.
- Ongoing touchpoints through CCM, PCM, and RPM ensure that patients receive timely interventions before conditions worsen or escalate to emergency visits.
- The structured documentation and follow-up required under CTBS enhance accountability and coordination across care settings.
Expanding Access to Care
- By recognizing virtual and asynchronous care, CTBS removes barriers associated with in-person scheduling, travel, and provider availability.
- Patients in rural or underserved areas gain access to consistent follow-up and clinical oversight through remote communication and monitoring.
- The general supervision model allows practices to extend capacity, leveraging nurses, medical assistants, and care coordinators to reach more patients efficiently.
Advancing Health Equity
- CTBS facilitates proactive care management for Medicare beneficiaries and high-risk populations who may struggle to access traditional care.
- When paired with Social Determinants of Health (SDOH) screening and documentation, these services help identify unmet social needs that drive inequities.
- By compensating for the often-unpaid work of care coordination, CTBS helps sustain primary care practices that serve vulnerable or low-income communities.
Challenges to Equity and Adoption
- Not all patients have reliable internet or technology access, limiting the reach of virtual CTBS programs.
- Providers serving low-income or rural areas may face lower reimbursement rates or limited payer coverage for newer CTBS codes.
- Sustained equity requires continued CMS policy updates to ensure reimbursement keeps pace with the complexity of multidisciplinary, community-based care.
Frequently Asked Questions about Care Team-Based Services (CTBS)
1. What are Care Team-Based Services (CTBS)?
CTBS are non–face-to-face, time-based services that recognize the collaborative work of physicians and clinical staff in managing patient care between visits. They include programs like Chronic Care Management (CCM), Principal Care Management (PCM), Remote Monitoring (RPM), and Virtual Check-Ins.
2. Who can bill for CTBS?
Physicians and qualified healthcare professionals (QHPs) such as nurse practitioners, physician assistants, and clinical nurse specialists can bill for CTBS.
Most codes allow general supervision, meaning care team members can perform much of the work while the billing provider oversees and remains responsible.
3. What are the new CTBS communication codes for 2024–2025?
New CPT codes 98008–98016 were introduced to replace and expand legacy codes G2010, G2012, and 98970–98972.
These new codes encompass broader asynchronous and multimodal communication methods, such as text, audio, or recorded media, allowing providers to capture more types of digital patient interactions.
4. What is the difference between CTBS and CCM?
- CTBS is the umbrella category that includes multiple service types — CCM, PCM, RPM, and digital communications.
- CCM specifically refers to the management of two or more chronic conditions over time, while CTBS extends to virtual and single-condition care coordination.
5. How are CTBS services reimbursed?
CTBS codes are billed per patient per month, based on total time documented for eligible non–face-to-face activities.
Payment amounts are determined using the RBRVS formula and vary based on service category, provider type, and geographic adjustment.
6. Can multiple providers bill CTBS for the same patient?
No. Only one provider or organization can bill for the same CTBS category (e.g., CCM, PCM) per patient per month.
If multiple specialties are involved, they must clearly define who holds care coordination responsibility.
7. Why are CTBS important for Value-Based Care?
CTBS codes operationalize care coordination and remote engagement, two pillars of value-based care.
They ensure providers are reimbursed for proactive outreach and team-based management that improves outcomes, reduces hospitalizations, and supports population health goals.
