What is (CPC+) Comprehensive Primary Care Plus?
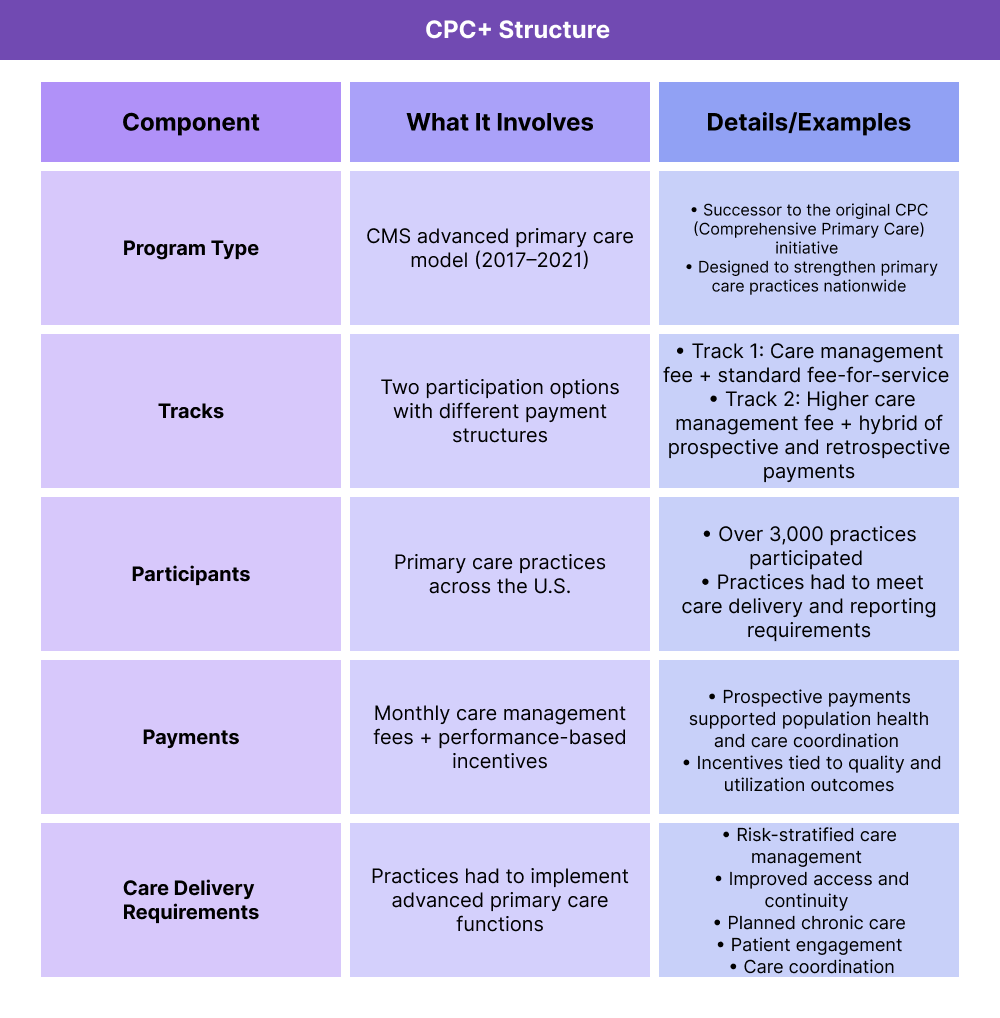
Comprehensive Primary Care Plus (CPC+) was a CMS advanced primary care medical home model launched in 2017 to strengthen primary care delivery and support value-based payment reform. CPC+ provided participating practices with care management fees, performance-based incentive payments, and optional payment redesigns to encourage more proactive, coordinated patient care.
The program operated across two tracks, each with different payment structures and care delivery requirements. Practices in CPC+ focused on areas such as care management for high-risk patients, improved access, population health management, and integration of behavioral health.
CPC+ concluded in 2021, but its lessons and framework continue to inform CMS efforts to advance value-based care in primary care, including newer models like Primary Care First (PCF).
Key Components of CPC+
CPC+ was structured around two participation tracks that combined financial support with care delivery requirements. Practices received enhanced payments in exchange for delivering more proactive, coordinated, and patient-centered primary care.
What Were the CPC+ Tracks?
- Track 1: Retained traditional fee-for-service payments but added care management fees and performance-based incentives.
- Track 2: Offered larger care management fees and partially replaced fee-for-service with population-based payments.
How Did CPC+ Payments Work?
Practices received a monthly per-patient care management fee, earned performance-based incentive payments, and — in Track 2 — received prospective payments instead of some fee-for-service billing.
What Care Delivery Changes Did CPC+ Require?
Practices had to expand services such as 24/7 access, risk-stratified patient management, comprehensive care planning, and behavioral health integration to qualify for enhanced payments.
How Comprehensive Primary Care Plus Worked in Practice
CPC+ was designed to support primary care practices in delivering more proactive and coordinated care. The program combined financial support with care delivery expectations, following a structured workflow from application to performance evaluation.
Step 1 — Practice Application and Selection
Eligible primary care practices applied to join CPC+. CMS selected participants across 18 regions, prioritizing practices ready to adopt advanced care delivery functions.
Step 2 — Upfront and Ongoing Payments
Practices received monthly care management fees to support services like care coordination and patient outreach. Track 2 practices also received prospective population-based payments in place of some fee-for-service revenue.
Step 3 — Enhanced Care Delivery
Practices implemented changes such as risk-stratified patient management, 24/7 access, behavioral health integration, and improved care coordination.
Step 4 — Performance Measurement
CMS tracked outcomes through quality, utilization, and patient experience metrics. Practices could earn additional performance-based incentives if they met targets.
Step 5 — Program Evaluation
CMS evaluated CPC+ on its ability to improve outcomes, reduce costs, and inform future primary care models. Lessons from CPC+ shaped newer initiatives like Primary Care First (PCF).
CPC+ and its Impact on Billing and Reimbursement
The Comprehensive Primary Care Plus (CPC+) program restructured how primary care practices were paid. Instead of relying solely on fee-for-service billing, CPC+ introduced a mix of care management fees, prospective payments, and performance incentives to better align reimbursement with value.
Monthly Care Management Fees
- Practices received per-patient payments to support enhanced services like care coordination and patient outreach.
- Fees were larger in Track 2, reflecting higher expectations for care delivery transformation.
Prospective Payments (Track 2)
- In Track 2, some traditional fee-for-service revenue was replaced with population-based prospective payments.
- This shift encouraged practices to focus on patient outcomes rather than volume of visits.
Performance-Based Incentives
- Practices could earn additional payments by meeting CMS targets for quality, utilization, and patient experience.
- Incentives ensured that financial rewards aligned with better care delivery.
Comparison to Fee-for-Service
- Under fee-for-service, practices are paid for each visit or service.
- Under CPC+, practices were paid for managing patient populations and achieving outcomes, moving toward value-based care.
Why CPC+ Matters in Billing and Reimbursement
By blending upfront fees, prospective payments, and performance incentives, CPC+ created a payment model that reduced reliance on visit-based billing. It qualified as an Advanced Alternative Payment Model (APM) under QPP, giving participants the opportunity to earn additional Medicare incentives.
Frequently Asked Questions about CPC+
1. What is CPC+ in healthcare?
Comprehensive Primary Care Plus (CPC+) was a CMS advanced primary care model launched in 2017. It provided participating practices with new payment structures and care delivery requirements to improve quality and reduce costs.
2. How did CPC+ payments work?
Practices received monthly care management fees, had opportunities to earn performance-based incentives, and — in Track 2 — received prospective population-based payments in place of some fee-for-service billing.
3. What were the CPC+ tracks?
- Track 1: Practices received care management fees, continued fee-for-service billing, and performance incentives.
- Track 2: Practices received larger care management fees and partial prospective payments, with higher expectations for care transformation.
4. How is CPC+ different from Primary Care First (PCF)?
CPC+ concluded in 2021, and CMS replaced it with Primary Care First (PCF). PCF builds on CPC+ by offering simpler participation options and stronger financial incentives for outcomes.
5. Is CPC+ still active?
No. CPC+ ended in 2021. However, its lessons continue to shape CMS models like PCF and future efforts to strengthen value-based primary care.
