What is a Certified Nursing Assistant (CNA)?
A Certified Nursing Assistant (CNA) is a trained healthcare support professional who provides basic patient care under the supervision of licensed clinical staff. CNAs assist with daily activities such as bathing, mobility, feeding, and vital sign monitoring, and are most commonly employed in long-term care, skilled nursing facilities, and hospital systems.
While CNAs are essential members of many care teams, they are not classified as Qualified Health Professionals (QHPs) under CMS definitions. This means they cannot independently bill Medicare, supervise clinical staff, or lead documentation for programs like Chronic Care Management (CCM) or Principal Care Management (PCM).
However, CNAs play a crucial support role in team-based care delivery, helping licensed providers track patient changes, manage non-clinical needs, and maintain continuity across settings—especially in older adult populations or post-acute care environments.
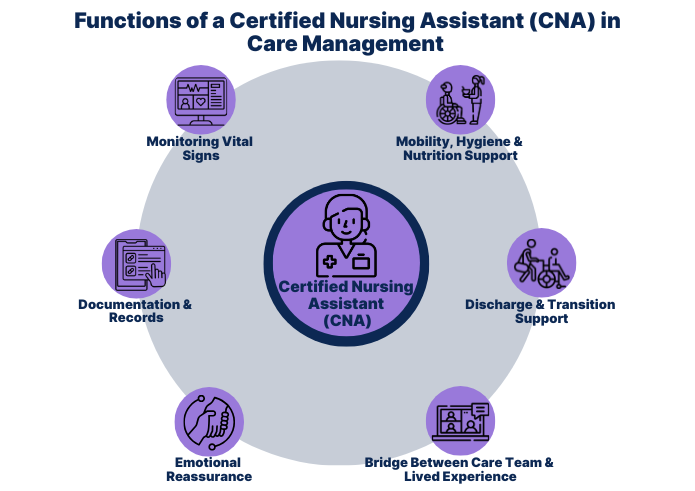
Key Functions of a CNA in Care Management Teams
Certified Nursing Assistants help extend the reach of care teams by managing essential daily tasks that support clinical care, reduce provider burden, and improve patient quality of life. While not authorized to diagnose or prescribe, CNAs are often the first point of contact in daily care routines—especially for patients with chronic conditions.
Typical CNA functions within a care management context include:
- Monitoring vital signs and reporting changes to licensed clinical staff
- Providing mobility assistance, hygiene support, and nutrition oversight
- Documenting daily observations for integration into electronic health records
- Supporting discharge preparation and home care transitions
- Offering emotional reassurance and establishing long-term rapport with patients
- Serving as the bridge between the care team and patients’ lived experience
These responsibilities make CNAs an important part of any chronic care delivery ecosystem, even if they are not eligible to initiate or bill care plans themselves.
The Role of a CNA in Care Delivery
Certified Nursing Assistants play a hands-on, patient-facing role that is foundational to high-quality care delivery—particularly in settings that serve patients with chronic or long-term health needs. CNAs are not licensed to assess or treat conditions, but they create the conditions for licensed providers to succeed by maintaining daily patient stability, comfort, and continuity.
In practice, CNAs may:
- Act as daily observers, flagging health status changes to the RN, NP, or supervising clinician
- Support continuity of care across shifts, departments, or discharge pathways
- Enable care plan adherence by ensuring hygiene, mobility, and nutrition goals are met
- Assist with telehealth or remote monitoring prep, such as gathering vitals for virtual consults
- Help reduce care gaps in underserved or high-volume care settings
While CNAs do not independently contribute to CMS billing workflows like CCM or PCM, their role is critical to sustaining outcomes for chronically ill or high-risk patient populations.
Billing and Supervision Limitations for CNAs
Certified Nursing Assistants are not considered Qualified Health Professionals (QHPs) by CMS and therefore cannot bill Medicare directly for any services or serve as supervising clinicians under care management programs.
Limitations Under CMS Rules:
- CNAs cannot bill for CPT codes related to Chronic Care Management (CCM), Principal Care Management (PCM), Transitional Care Management (TCM), or Annual Wellness Visits.
- They may not supervise other clinical staff or serve as the designated provider of record for CMS programs.
- They cannot develop or approve care plans, even if they contribute observations.
However, CNAs can:
- Work under general supervision from a QHP (e.g., NP, PA, CNS, MD)
- Perform delegated tasks that support documentation, vitals monitoring, or patient communication
- Provide care that complements billable time tracked by a supervising provider (e.g., when contributing to 20-minute thresholds for CCM under general supervision)
While CNAs cannot generate revenue through direct billing, their presence allows QHPs to practice at the top of their license, and their involvement can improve patient engagement and satisfaction—important metrics in value-based care.
Frequently Asked Questions about CNAs
1. What is a CNA in healthcare?
A Certified Nursing Assistant (CNA) is a healthcare support professional trained to provide basic patient care such as hygiene, mobility, and vital signs monitoring under supervision from licensed providers.
2. Is a CNA a Qualified Health Professional (QHP)?
No. CNAs are not considered QHPs under CMS guidelines and therefore cannot bill Medicare or supervise staff in care management programs.
3. What’s the difference between a CNA and a medical assistant?
CNAs are typically trained for inpatient or long-term care settings and focus on daily living assistance. Medical assistants usually work in outpatient environments and support clinical tasks like rooming patients or handling paperwork.
4. Can a CNA contribute to Medicare billing for Chronic Care Management?
Indirectly, yes. CNAs may assist with supportive tasks—such as gathering vitals or reporting observations—but they cannot bill independently or document time toward billing thresholds unless under direct QHP supervision.
5. Who supervises a CNA on a care team?
CNAs typically report to registered nurses (RNs) or QHPs such as nurse practitioners, physician assistants, or physicians. Supervision requirements vary by state and care setting.
6. Are CNAs used in chronic care management programs?
Yes, but in a supportive role. They help implement the care plan developed by a licensed provider and are often key to maintaining daily patient stability in high-risk populations.
