What is CMP (Civil Monetary Penalty)?)
A Civil Monetary Penalty (CMP) is a financial fine CMS can impose on a nursing home when a survey identifies noncompliance with federal participation requirements. CMPs are one of the primary enforcement tools CMS uses to correct serious deficiencies, deter repeat violations, and protect resident health and safety.
CMPs are issued when a facility’s failures are significant enough to warrant monetary enforcement rather than (or in addition to) corrective action alone. The penalty amount is tied to the scope and severity of the deficiency, and CMS can apply CMPs for a single incident or on a per-day basis until the problem is resolved.
In practice, CMPs function as both a compliance consequence and a signal of regulatory risk. They often follow issues such as harm-level care failures, repeat survey citations, or systemic quality breakdowns. For Skilled Nursing Facilities (SNFs), CMP exposure creates direct financial impact and can also trigger heightened oversight, reputational risk, and increased urgency around quality improvement.
Key Components of an CMPs
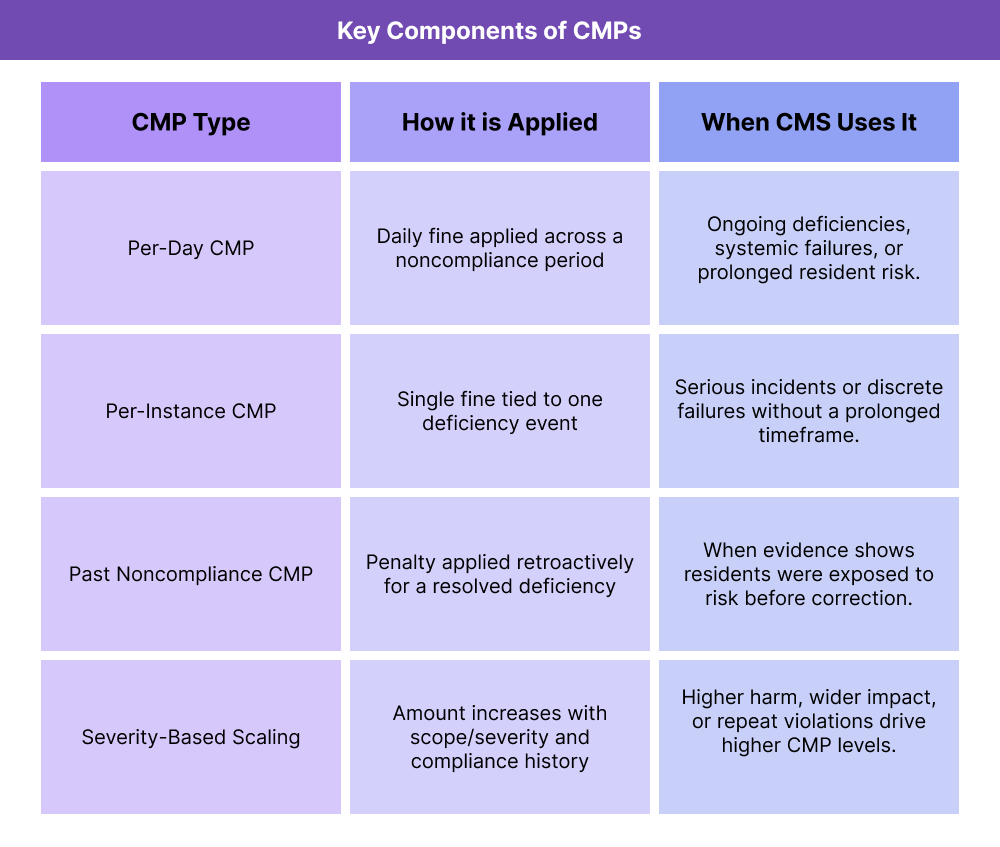
Civil Monetary Penalties (CMPs) are structured enforcement fines CMS uses to address nursing home noncompliance. The CMP framework is designed to tie the penalty amount and method to the seriousness of the deficiency and the length of time residents were exposed to risk. Understanding how CMPs are categorized helps facilities anticipate exposure, respond appropriately after surveys, and avoid repeat enforcement.
Per-Day CMPs
Per-day CMPs are applied when a deficiency exists over a period of time. CMS sets a daily penalty amount and applies it for each day the facility is not in substantial compliance, starting from when the noncompliance began until it is corrected or CMS determines compliance has been restored.
Per-day CMPs are most often used when deficiencies reflect ongoing systemic failures or prolonged risk to residents.
Per-Instance CMPs
Per-instance CMPs are a one-time penalty applied to a specific deficiency event. CMS uses this approach when a violation is serious but does not require a daily penalty to reflect prolonged noncompliance.
Per-instance CMPs may be used even when immediate jeopardy is not present, depending on the severity and scope of the incident.
Scope and Severity Drives CMP Level
CMP amounts are not random. CMS ties CMP level to the survey scope-and-severity grid, which considers:
- The level of actual harm or jeopardy to residents
- How widespread the deficiency was
- Whether the problem reflects a pattern or an isolated incident
- The facility’s compliance history
Facilities with repeat or harm-level deficiencies face higher CMP exposure.
CMPs for Past Noncompliance
CMPs can also be imposed for deficiencies that were corrected before surveyors arrived but are determined to have existed previously. CMS can apply penalties retroactively when evidence shows residents were at risk during a defined period before correction.
How CMPs Work in Practice
CMPs follow a structured enforcement pathway tied to the CMS survey process. While the exact timeline can vary by state and deficiency type, the operational flow is consistent across Skilled Nursing Facilities (SNFs).
Step 1: Survey Identifies a Deficiency
CMPs begin with a survey finding. Surveyors identify deficiencies during standard, complaint, or follow-up surveys and assign each citation a scope-and-severity level based on resident risk and facility impact. Higher-severity or repeat deficiencies are more likely to trigger CMP enforcement.
Step 2: CMS Determines CMP Type and Amount
After the survey, CMS (often through the state agency) determines whether a CMP is appropriate and whether it should be applied per-day, per-instance, or for past noncompliance. The amount is calibrated to the severity level and the facility’s compliance history.
Step 3: Facility Receives Notice and Responds
The facility receives a formal enforcement notice outlining:
- The deficiency citation(s)
- CMP type and duration (if per-day)
- Penalty amount and calculation logic
- Required correction expectations and deadlines
At this stage, facilities typically submit a Plan of Correction (PoC) and begin remediation. If they believe the citation is incorrect, they may begin the appeal process.
Step 4: CMP Stops When Compliance Is Restored (Per-Day Only)
For per-day CMPs, the penalty continues until CMS determines the deficiency is corrected and the facility has returned to substantial compliance. Follow-up surveys or evidence reviews confirm correction.
Step 5: CMP Payment or Reinvestment Pathway
Once finalized, CMPs are either paid by the facility or handled through a structured reinvestment program in some states. CMP funds are pooled and later used for resident-benefit projects approved under the Civil Money Penalty Reinvestment Program.
CMPs in Billing, Reimbursement, and System Limitations
CMPs create direct financial risk for SNFs and can also trigger downstream reimbursement and oversight consequences. While CMPs are not claims-related penalties, they are tightly linked to Medicare participation status because they arise from survey findings tied to federal compliance standards.
How CMPs Affect Financial Stability
CMPs are paid out as fines, which can be substantial depending on severity and duration. Per-day CMPs can escalate quickly if deficiencies remain unresolved, creating a compounding cost burden. Facilities with multiple citations or repeat enforcement often face higher penalty levels and more frequent follow-up oversight.
In addition to the fine itself, CMPs can drive indirect costs such as staff time for corrective action work, legal or consulting support, and operational rework to stabilize compliance.
CMPs and Survey-Driven Reimbursement Risk
CMPs do not automatically stop Medicare billing, but they signal high regulatory risk. Severe citations tied to CMPs can result in:
- Heightened survey frequency and expanded oversight
- Additional enforcement actions if deficiencies persist
- Participation risk if compliance does not return to substantial levels
- Increased audit scrutiny due to documented quality failures
Because Medicare participation is the foundation for SNF billing, CMP exposure is treated operationally as a reimbursement-protection issue.
System Limitations and Compliance Watch-Outs
Common CMP risk drivers relate to system consistency, not isolated mistakes. Watch-outs include:
- Corrective actions that fix symptoms but not root causes
- Documentation that does not clearly support compliance claims
- Repeat deficiencies that CMS interprets as systemic failure
- Weak internal monitoring that misses risk before surveyors find it
Technology and workflow tracking can support early detection and remediation, but CMP avoidance depends on real, sustained compliance improvement.
How CMPs Influence Quality, Access, and Equity in Healthcare
CMPs exist to protect residents by forcing facilities to correct unsafe or low-quality conditions. Because CMPs are tied to survey scope-and-severity, they reinforce which care failures are most critical to resident well-being and safety.
Quality and Safety Impact
CMP enforcement pushes facilities to address high-risk care gaps such as preventable harm, unsafe staffing patterns, medication failures, infection control breakdowns, and resident rights violations. In practice, CMPs help drive:
- Faster remediation of serious deficiencies
- Stronger internal monitoring and risk detection
- More durable quality improvement systems to prevent repeat findings
Facilities that use CMP events as catalysts for root-cause correction often see measurable safety gains beyond compliance recovery.
Access and Continuity Effects
When CMPs lead to heightened oversight or participation risk, facilities may experience staffing disruption, reputational damage, or operational instability that affects resident continuity. In severe cases, enforcement can create transfer pressure or admission slowdowns, which reduces access in communities with limited SNF capacity.
Equity Considerations
Equity risks arise when enforcement instability leads to fewer high-quality SNF options in already underserved regions. If CMP-related operational strain causes closures or persistent quality gaps, vulnerable residents may face longer waits, farther travel, or fewer safe care choices.
Consistent improvement after CMP enforcement helps protect not only compliance, but equitable access to safe long-term care.
Frequently Asked Questions about CMP
1. What is a CMP (Civil Monetary Penalty)?
A CMP (Civil Monetary Penalty) is a financial fine CMS can impose on a nursing home when a survey identifies noncompliance with federal participation requirements that put residents at risk.
2. When does CMS issue CMPs to nursing homes?
CMS issues CMPs when deficiencies are serious enough to warrant monetary enforcement, such as harm-level findings, immediate jeopardy situations, or repeat violations showing systemic failure.
3. What is the difference between per-day and per-instance CMPs?
Per-day CMPs apply a daily fine for each day a facility remains out of compliance. Per-instance CMPs are a one-time penalty tied to a specific deficiency event.
4. How is a CMP amount determined?
CMP amounts are based on the survey scope-and-severity level, the duration of noncompliance (for per-day penalties), and the facility’s compliance history.
5. Can CMPs be applied for past noncompliance?
Yes. CMS can impose CMPs retroactively if survey evidence shows a deficiency existed and put residents at risk before it was corrected.
6. Can a nursing home appeal a CMP?
Yes. Facilities can appeal CMPs through the survey and enforcement appeal process, often beginning with an Informal Dispute Resolution (IDR) or other formal appeal pathways.
7. What is the Civil Money Penalty Reinvestment Program?
The Civil Money Penalty Reinvestment Program is a CMS-approved process in which collected CMP funds are pooled and later used for resident-benefit projects such as quality improvement initiatives, staff training, or safety upgrades.
