What is a CBA (Competitive Bidding Area)?
A Competitive Bidding Area (CBA) is a geographic region where the Medicare Competitive Bidding Program (CBP) applies to certain Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) items. CMS defines CBAs—typically by counties and ZIP codes within metropolitan or other designated areas—to determine where competitively bid pricing and contract supplier rules are in effect. If a beneficiary’s primary residence is located in a CBA, the DMEPOS items included in CBP for that area are subject to competitive bidding requirements.
CBAs function as the location-based mechanism that activates CBP rules. Within a CBA, Medicare generally requires beneficiaries to obtain competitively bid DMEPOS items from contract suppliers in order to receive full coverage. These geographic boundaries are therefore critical for ordering and discharge workflows, since supplier eligibility and reimbursement rates change depending on whether the patient lives inside or outside a CBA.
From an operational standpoint, CBAs can affect continuity of equipment access, referral routing, and claims outcomes. Providers and care teams must verify a beneficiary’s home address against current CBA definitions before directing them to a supplier, especially for high-volume equipment categories. Understanding how CBAs are defined and updated helps organizations avoid coverage disruptions, prevent denials tied to non-contract suppliers, and ensure Medicare patients receive equipment through compliant access pathways.
Key Components of CBAs (Competitive Billing Areas)
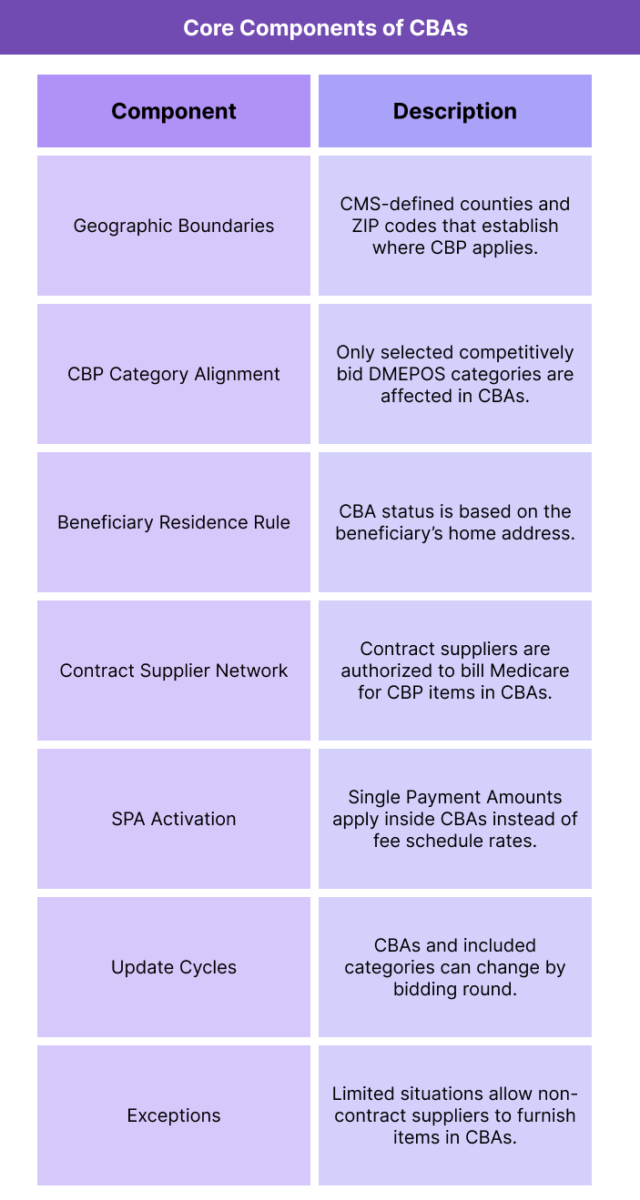
Competitive Bidding Areas are the geographic foundation of the Medicare Competitive Bidding Program. CBAs define where competitive bidding rules apply, determine which suppliers can furnish covered items, and trigger bid-based payment rates for selected DMEPOS categories. Understanding how CBAs are structured is essential for compliant ordering and supplier referral workflows.
CBAs operate through a combination of boundary definitions, product category alignment, supplier network requirements, and beneficiary residence rules that collectively determine whether competitive bidding applies to a given patient and item.
Geographic Boundary Definitions
CBAs are delineated by CMS using counties and ZIP codes, typically anchored to metropolitan statistical areas or other designated regional groupings. These boundaries specify where CBP pricing and contract supplier restrictions are activated.
Alignment With CBP Product Categories
CBAs apply only to the DMEPOS product categories included in CBP for that region. A beneficiary living in a CBA is subject to competitive bidding rules only for those selected item groups, not for all DMEPOS.
Beneficiary Residence Determination
Whether a beneficiary is considered “in a CBA” depends on their primary residence, not the location of the ordering provider or supplier. The beneficiary’s home address is the key factor in determining CBA applicability.
Contract Supplier Network Requirement
Within each CBA, CMS establishes a network of contracted suppliers for competitively bid categories. These suppliers are the only entities generally authorized to bill Medicare for CBP items furnished to beneficiaries living in the area.
Single Payment Amount Activation
CBAs are the regions where Single Payment Amounts replace standard fee schedule rates for competitively bid items. Outside CBAs, those same items revert to traditional fee schedule payment rules.
CBA Updates and Bidding Cycles
CMS updates CBAs through competitive bidding rounds. The list of CBAs, their boundaries, and the product categories included may change as the program evolves, requiring ongoing monitoring by suppliers and providers.
Exceptions and Special Access Rules
Certain exceptions may allow non-contract suppliers to furnish items in CBAs, such as grandfathering for capped rental items or special circumstances for complex equipment access. These exceptions are narrow and policy-dependent.
How CBAs Work in Practice
Competitive Bidding Areas affect DMEPOS ordering and reimbursement through a residence-based rule: whether a beneficiary lives inside or outside a CBA determines which suppliers can furnish certain items and which payment rates apply. In day-to-day operations, CBAs are the trigger point for competitive bidding compliance.
1. CMS Defines CBAs for a Bidding Round
CMS establishes CBA boundaries as part of each competitive bidding cycle. These areas are published in advance and specify the regions where competitive bidding rules will apply to selected DMEPOS categories.
2. A Beneficiary’s Home Address Determines CBA Status
When a Medicare patient needs a competitively bid item, the key question is where they live. If their primary residence is within a CBA, competitive bidding rules apply to CBP-covered categories. If they live outside a CBA, standard fee schedule and supplier rules apply.
3. Providers Verify CBA Status During Ordering
Ordering clinicians, discharge planners, and care teams must check whether the patient’s residence falls within a current CBA. This step is especially important for discharge-related equipment needs where delays or referral errors can disrupt transitions of care.
4. Referrals Are Routed to Contract Suppliers in CBAs
If the patient lives in a CBA and the ordered item is part of a competitively bid category, the referral must go to a contract supplier for Medicare to cover the item at the competitive rate. Using a non-contract supplier in a CBA usually results in claim denial or reduced coverage.
5. Claims Are Paid Using SPA Rates Inside CBAs
For competitively bid items furnished to CBA residents, Medicare pays the Single Payment Amount rather than the standard fee schedule rate. The supplier must bill correctly under their contract eligibility and item category designation.
6. Service Access Is Monitored Within CBAs
CMS monitors access adequacy within CBAs by tracking supplier performance, beneficiary complaints, delivery timelines, and network sufficiency. If access problems emerge, CMS may issue policy adjustments or exceptions.
7. CBAs Can Change Across Bidding Cycles
Because CBAs can be updated or redefined with new bidding rounds, providers and suppliers must continually monitor changes. A beneficiary who was outside a CBA in a previous cycle may fall within one after boundaries shift, altering referral and billing rules.
CBAs in Billing, Reimbursement, and System Limitations
Competitive Bidding Areas (CBAs) directly determine when competitive bidding pricing and supplier restrictions apply to DMEPOS claims. While CBAs are not billed independently, they are a core eligibility variable that Medicare contractors use to adjudicate claims, set allowed amounts, and validate supplier authority.
How CBAs Affect Reimbursement Rates
CBAs are the geographic trigger for Single Payment Amounts (SPAs). If a beneficiary’s residence is within a CBA and the item is in a competitively bid category, the SPA replaces the standard DMEPOS fee schedule rate. Outside CBAs, those same items are reimbursed using fee schedule rules, meaning payment can differ purely based on where the patient lives.
Billing Requirements Tied to CBA Status
Claims for CBP items furnished to CBA residents must be billed by contract suppliers that are authorized for that specific CBA and product category. If a non-contract supplier submits a claim for a competitively bid item to a CBA beneficiary, Medicare will typically deny or reduce payment. Correct billing therefore depends on verifying residence, item category inclusion, and contract eligibility before delivery.
Referral Accuracy as a Revenue Cycle Dependency
Because CBA rules are residence-based, provider referral workflows must be aligned to avoid misrouting. If a patient is referred to a non-contract supplier in a CBA, equipment delivery may be delayed and claims may be nonpayable. This creates operational risk during transitions of care, especially for discharge equipment needs.
Policy Variability Across Bidding Rounds
CBAs are updated through competitive bidding cycles, and boundaries can change. Supplier contracts may also shift round to round. These moving parts create billing risk if organizations rely on outdated maps or assume prior supplier eligibility still applies.
Exceptions, Grandfathering, and Complexity
Limited exceptions may allow non-contract suppliers to furnish items in CBAs, such as grandfathered capped rental items or special circumstances tied to complex equipment access. These exceptions are narrow and policy-specific, making them a frequent source of billing confusion if not clearly documented and verified.
System Limitations and Administrative Burden
CBA-related billing depends on accurate address data, up-to-date geographic definitions, and consistent supplier network information. For multi-region providers and suppliers, maintaining current CBA logic across referral and claims systems adds administrative overhead and increases the chance of avoidable denials when processes are not standardized.
How CBAs Influence Quality, Access, and Equity in Healthcare
CBAs shape beneficiary access to equipment by determining which suppliers can serve certain areas and what pricing rules apply. Their impact on quality and equity depends on whether competitive bidding regions maintain adequate supplier networks and service responsiveness.
Access to DMEPOS in CBAs
Within CBAs, beneficiaries must generally use contract suppliers for competitively bid items. When networks are sufficient, access is stable. When supplier coverage is thin or product needs are specialized, CBAs can contribute to longer delivery times, limited choice, or care-transition delays.
Quality of Supplier Networks
Because CBAs restrict supply to contracted vendors, the quality of contracted networks matters. If contracted suppliers are responsive and clinically aligned, CBAs can support standardized service delivery. If supplier capacity is limited, beneficiaries may experience reduced service support or difficulty securing specialized equipment.
Equity Implications Across Regions
CBAs are commonly centered on metropolitan areas, but when competitive bidding rules apply in regions with uneven supplier distribution, access burdens can fall more heavily on lower-resource communities. Beneficiaries with limited transportation, low health literacy, or less caregiver support may struggle more to find and coordinate with eligible suppliers.
Rural and Medically Underserved Effects
Patients in or near rural regions that overlap with CBAs may face access friction if contract supplier density is low. Even when rural areas are outside CBAs, nearby CBA boundaries can still create confusion in ordering workflows, affecting timely access for high-need patients.
Impact on High-Complexity Beneficiaries
CBAs can be challenging for beneficiaries who require complex mobility equipment, respiratory setups, or other high-touch services. If contracted suppliers do not provide adequate fitting, education, or follow-up, vulnerable patients may experience disproportionate care disruption.
Balancing Cost Control With Equitable Access
CBAs help Medicare contain costs through competitive pricing, but their equity impact depends on ongoing CMS monitoring of network adequacy, beneficiary complaints, and product availability. Cost savings translate into positive system outcomes only when access for high-need Medicare populations remains stable.
Frequently Asked Questions about Competitive Bidding Areas (CBAs)
1. What is a Competitive Bidding Area (CBA)?
A CBA is a CMS-defined geographic region where the Medicare Competitive Bidding Program applies to certain DMEPOS items. Beneficiaries living in a CBA must generally use contract suppliers for competitively bid items to receive full Medicare coverage.
2. How does Medicare decide what areas are CBAs?
CMS defines CBAs by counties and ZIP codes, typically tied to metropolitan or designated regional groupings. CBAs are established and updated through competitive bidding rounds.
3. What items are affected by CBAs?
Only DMEPOS items included in competitively bid product categories are affected in CBAs. Items not part of CBP remain under standard Medicare fee schedule and supplier rules.
4. How do I know if a patient lives in a CBA?
CBA status is determined by the beneficiary’s primary residence. Providers and suppliers must verify the home address against current CBA maps to confirm whether competitive bidding rules apply.
5. Do CBAs affect reimbursement rates?
Yes. For competitively bid items furnished to CBA residents, Medicare pays the Single Payment Amount instead of the standard fee schedule rate.
6. Who can supply CBP items to beneficiaries in CBAs?
Only contract suppliers authorized for that CBA and product category can bill Medicare for competitively bid items delivered to beneficiaries living in the area.
7. What happens if a CBA beneficiary uses a non-contract supplier?
In most cases, Medicare will deny or reduce payment for competitively bid items from non-contract suppliers in CBAs, potentially increasing the beneficiary’s out-of-pocket cost.
8. Do CBAs apply if the provider is outside the area?
Yes. CBA rules are based on where the beneficiary lives, not where the ordering provider or supplier is located.
9. Can CBA boundaries change over time?
Yes. CBAs can be redefined with new competitive bidding rounds, and product categories and contract suppliers can change as well.
10. Are there exceptions to contract-supplier requirements in CBAs?
Limited exceptions exist, such as grandfathering for certain capped rental items or special access circumstances. These exceptions are narrow and must be documented and verified.
11. How do CBAs affect hospital discharge equipment planning?
Discharge teams must confirm CBA status before routing referrals. Misrouting to a non-contract supplier can delay delivery and make the claim nonpayable.
12. Why do CBAs exist within Medicare?
CBAs are used to apply competitive bidding rules in areas where market-based pricing is expected to lower costs while maintaining access and quality standards.
