What is a Behavioral Health Care Manager (BHCM)?
A Behavioral Health Care Manager (BHCM) is a licensed clinical professional who coordinates mental and behavioral health services as part of a collaborative care team. Often working in primary care or outpatient settings, the BHCM serves as the main point of contact for patients receiving behavioral health support—particularly within evidence-based care models like the Collaborative Care Model (CoCM).
BHCMs play a critical role in connecting patients with appropriate resources, tracking clinical progress, and communicating with both primary care providers and psychiatric consultants. The abbreviation BHCM is sometimes used interchangeably with job titles like Behavioral Health Care Coordinator or Behavioral Health Case Manager, depending on the organization.
Key Components of a BHCM Role
- Licensed mental health clinician (e.g., LCSW, LPC, LMFT, or RN with behavioral health experience)
- Serves as the liaison between patient, PCP, and psychiatric consultant
- Manages behavioral health registries and symptom tracking tools
- Provides brief interventions, care planning, and patient education
- Works under the Collaborative Care Model (CoCM) or similar team-based approaches
- Must have strong communication, documentation, and motivational interviewing skills
What BHCMs Do in Practice
Behavioral Health Care Managers (BHCMs) serve as the frontline coordinators of behavioral health services in primary care and collaborative care settings. Their role bridges the gap between patients, primary care providers, and psychiatric consultants—ensuring that mental health needs are tracked, addressed, and integrated into the broader care plan.
Key Responsibilities:
- Maintain a behavioral health registry to track caseload and monitor patient progress
- Conduct standardized assessments (e.g., PHQ-9, GAD-7) and monitor symptom changes
- Deliver brief evidence-based interventions, such as behavioral activation or problem-solving therapy
- Engage patients regularly via phone, telehealth, or in-person follow-up
- Coordinate treatment adjustments with psychiatric consultants and communicate recommendations to the primary care provider
- Document all encounters in alignment with CoCM billing and clinical quality standards
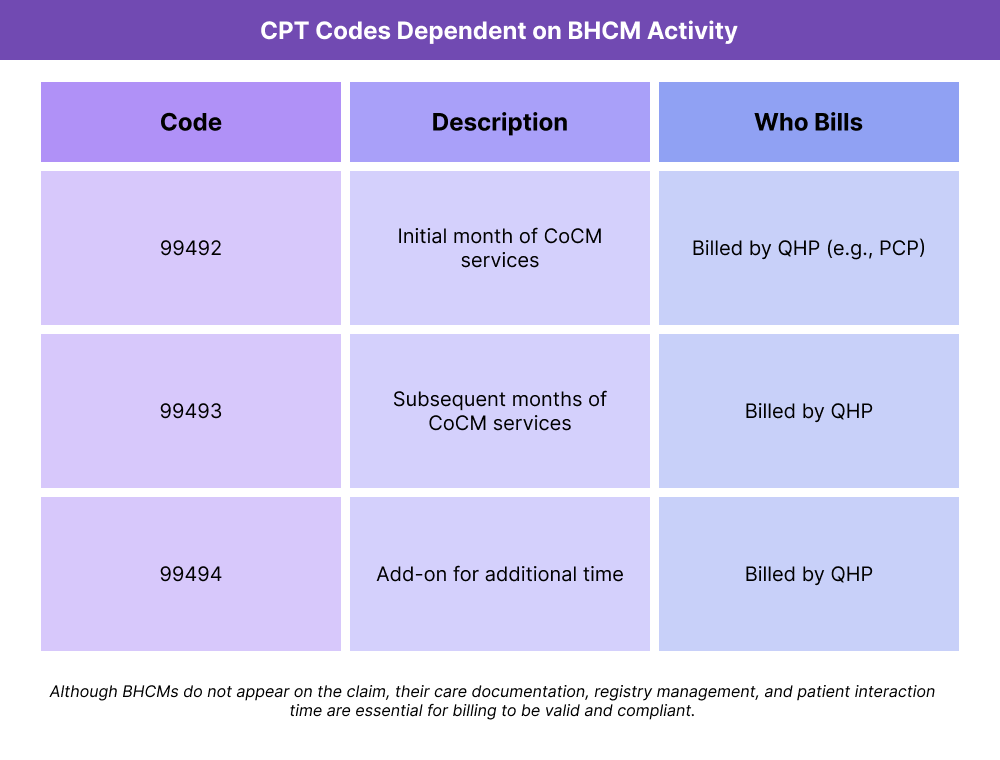
In a Collaborative Care Model (CoCM), BHCMs are essential for meeting the requirements of CPT codes 99492–99494, though they do not bill independently—a Qualified Health Professional (QHP) (usually the PCP or NP) must report the codes.
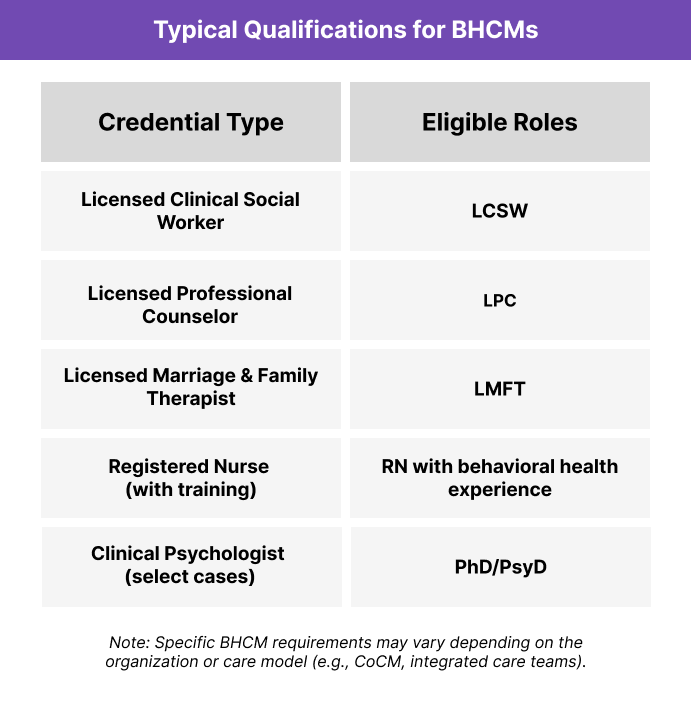
Credentialing and Eligibility for BHCMs
There’s no single, nationally standardized credential for becoming a Behavioral Health Care Manager (BHCM)—instead, eligibility is based on a combination of licensure, training, and the care model in use. Most organizations align their requirements with the needs of models like the Collaborative Care Model (CoCM) or broader integrated care initiatives.
Common Requirements for BHCM Roles:
- Master’s-level licensure in a mental health discipline (e.g., LCSW, LPC, LMFT)
- Behavioral health experience in clinical or care coordination settings
- Familiarity with evidence-based treatment approaches (e.g., behavioral activation, PST)
- Comfort using validated screening tools (e.g., PHQ-9, GAD-7)
- Experience working in team-based, interdisciplinary environments
- In some settings, Registered Nurses (RNs) may serve as BHCMs with additional behavioral health training
Note: Some organizations may refer to the BHCM role as a Behavioral Health Coordinator, Behavioral Health Case Manager, or Care Manager depending on their structure.
In CoCM implementations, BHCMs must also be trained in registry-based care and work under the supervision of a psychiatric consultant and a QHP to fulfill billing and documentation standards.
Billing and Reimbursement Involving BHCMs
Behavioral Health Care Managers (BHCMs) do not typically bill independently for their services, but they are instrumental to enabling reimbursement in care models like the Collaborative Care Model (CoCM). Under this model, BHCMs deliver many of the care components that are reported and reimbursed through CPT codes 99492, 99493, and 99494 — billed by a supervising Qualified Health Professional (QHP).
How BHCMs Support CoCM Billing:
- Track and document patient interactions and care coordination activities in a behavioral health registry
- Use validated screening tools (e.g., PHQ-9) to demonstrate clinical progress
- Provide evidence-based interventions under the supervision of a psychiatric consultant
- Collaborate regularly with the primary care provider to review caseloads and adjust treatment plans
Frequently Asked Questions about BHCMs
1. What is a BHCM?
A Behavioral Health Care Manager (BHCM) is a licensed clinical professional who coordinates behavioral health services as part of a collaborative care team. BHCMs work closely with patients, primary care providers, and psychiatric consultants to support mental health treatment and care continuity.
2. What qualifications are required to be a BHCM?
Most BHCMs are licensed mental health professionals such as:
- LCSWs (Licensed Clinical Social Workers)
- LPCs (Licensed Professional Counselors)
- LMFTs (Licensed Marriage and Family Therapists)
- Or Registered Nurses with behavioral health experience
Qualifications may vary based on the organization or care model in use.
3. What does a BHCM do in the Collaborative Care Model?
In CoCM, BHCMs:
- Manage behavioral health registries
- Track symptoms using tools like PHQ-9
- Deliver brief interventions
- Coordinate with a psychiatric consultant
- Support the primary care provider in updating care plans
They are the primary point of patient contact for behavioral health services.
4. Is 'BHCM' the same as a Behavioral Health Case Manager?
Sometimes. The terms BHCM, Behavioral Health Care Manager, and Behavioral Health Case Manager may be used interchangeably depending on the organization. However, BHCM is most often used in clinical care models like CoCM that require credentialed providers and structured workflows.
