What is an Accountable Care Organization (ACO)?
An Accountable Care Organization (ACO) is a group of doctors, hospitals, and other healthcare providers who voluntarily come together to deliver coordinated, high-quality care to patients. ACOs aim to ensure that patients—especially those with chronic or complex conditions—get the right care at the right time, while avoiding unnecessary duplication of services and preventing medical errors.
When an ACO succeeds in improving quality and reducing healthcare costs, it may share in the savings it generates for the payer, such as Medicare or a commercial insurer. This approach shifts the focus from volume-based care to value-based care, aligning financial incentives with patient outcomes.
Key Components of an Accountable Care Organization
Accountable Care Organizations are built around several foundational elements that enable collaborative, Value-Based Care:
- Participating Providers: ACOs are made up of doctors, hospitals, and other healthcare professionals who voluntarily join together to coordinate care.
- Care Coordination Infrastructure: ACOs use shared data systems and team-based workflows to reduce duplication of services and improve care transitions.
- Performance Measurement: ACOs track quality metrics such as hospital readmissions, preventive screenings, and patient experience to assess performance.
- Shared Financial Risk: Many ACOs operate under payment models where they can share in cost savings or take on risk for overspending—aligning incentives with outcomes.
- Accountability to a Payer: Most ACOs have formal agreements with Medicare or commercial insurers that define benchmarks, quality targets, and reporting requirements.
Together, these components aim to reduce unnecessary spending while improving patient health outcomes—especially in populations with chronic conditions or high complexity.
How Accountable Care Organizations Work in Practice
In a typical ACO, participating providers agree to take collective responsibility for the cost and quality of care for a defined patient population. Here’s how the model works in practice:
- Patient Attribution: Patients are assigned to an ACO based on where they receive the majority of their primary care—usually through claims data or EHR integration.
- Care Coordination: ACOs emphasize communication between providers, including shared care plans, referral tracking, and discharge follow-up to reduce fragmentation.
- Data Sharing and Analytics: ACOs rely on real-time access to clinical and claims data to identify care gaps, manage risk, and support population health strategies.
- Quality Reporting: Performance is measured using standardized metrics such as hospital readmissions, diabetes control, and preventive screening rates.
- Financial Incentives: If the ACO succeeds in improving outcomes and lowering costs compared to benchmark spending, it may receive a portion of the savings—shared among participants.
Benefits and Challenges of Accountable Care Organizations
Benefits of ACO Participation
- Improved Care Coordination: Shared infrastructure and incentives reduce fragmentation and encourage aligned treatment plans.
- Cost Savings Opportunities: ACOs can share in payer savings when they lower total cost of care while meeting quality benchmarks.
- Population Health Management: Access to claims and clinical data supports risk stratification and proactive outreach.
- Quality Performance Transparency: Standardized metrics allow providers to benchmark outcomes and improve over time.
- Regulatory Alignment: ACOs support Medicare quality initiatives and commercial value-based care contracts.
Challenges of ACO Participation
- Data Integration Complexity: Aggregating EHR, claims, and social data across entities requires significant infrastructure.
- Shared Risk Models: Downside risk contracts require strong financial and clinical oversight to avoid penalties.
- Care Standardization: Aligning workflows and practice patterns across independent providers can be difficult.
- Patient Attribution Gaps: Patients are not always aware they’re part of an ACO, which can affect engagement and outcomes.
How Accountable Care Organizations Are Reimbursed
Accountable Care Organizations participate in alternative payment models that reward performance rather than volume. Most ACOs operate under shared savings and shared risk agreements with payers like Medicare or commercial insurers. Under this model:
- The ACO is assigned a population of patients
- A spending benchmark is established based on historical costs and risk adjustment
- If the ACO delivers care for less than the benchmark while meeting quality standards, it may keep a portion of the savings
- In risk-bearing arrangements, the ACO may owe money back if it overspends or underperforms
Common ACO Payment Models:
- One-sided risk (upside only): Eligible for shared savings, but not liable for losses
- Two-sided risk (upside + downside): Greater potential rewards, but also financial penalties for exceeding targets
- Capitation/global budgets: Some advanced models provide fixed per-member-per-month payments tied to performance
These reimbursement approaches are core to value-based care and encourage providers to manage total cost of care across a full patient journey—not just within isolated encounters.
Frequently Asked Questions about ACOs
1. What is an Accountable Care Organization (ACO)?
An ACO is a group of healthcare providers who agree to work together to coordinate care and improve quality while reducing costs. They are rewarded based on performance, not volume.
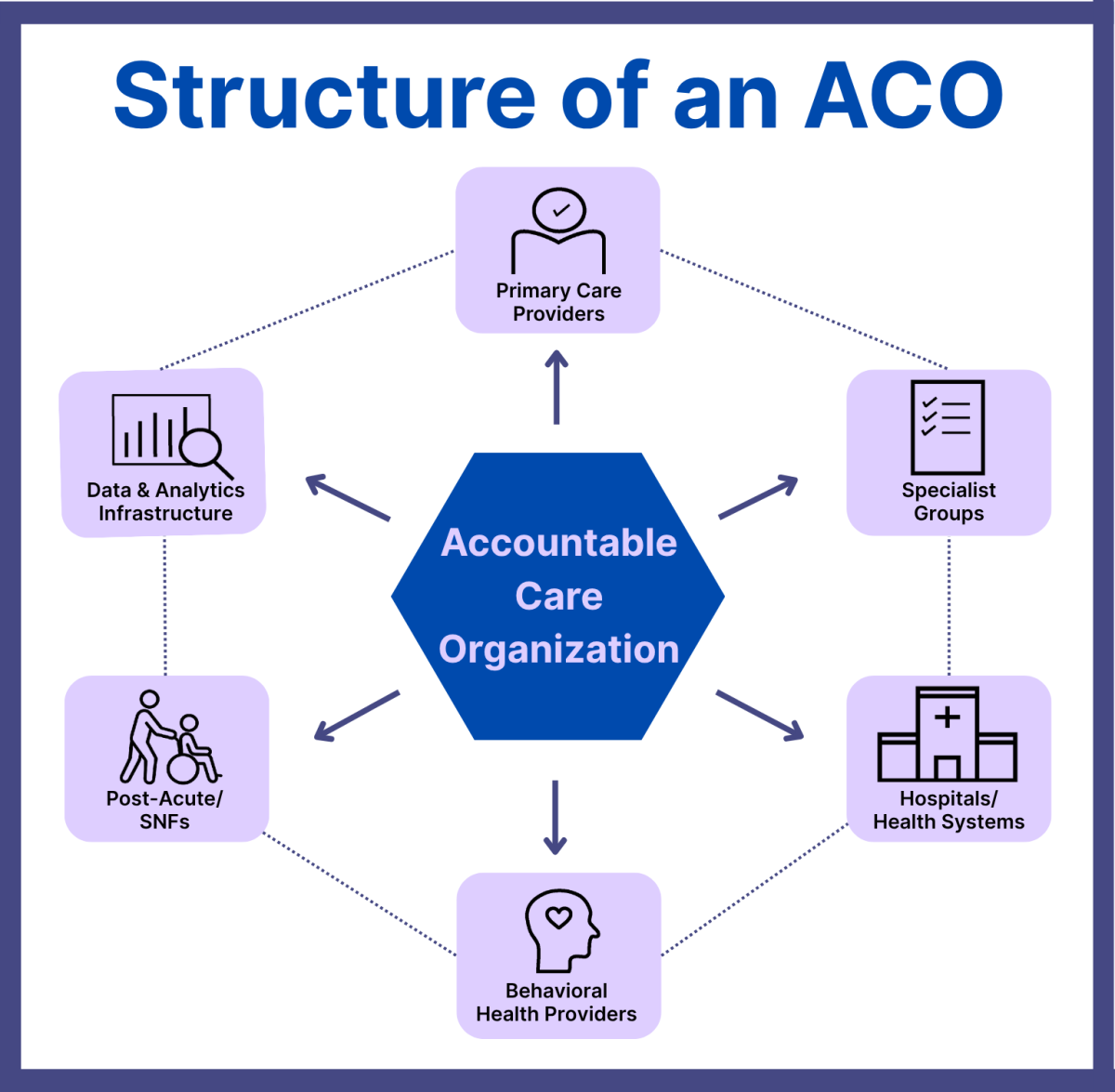
2. Who participates in an ACO?
ACOs typically include primary care providers, specialists, hospitals, behavioral health providers, post-acute care organizations, and data infrastructure partners.
3. How do ACOs save money?
By reducing unnecessary tests and procedures, improving care coordination, and avoiding hospital readmissions, ACOs can lower total cost of care. If they meet quality standards, they may keep a portion of those savings.
4. What is the Medicare Shared Savings Program (MSSP)?
The MSSP is Medicare’s flagship ACO program. It allows ACOs to share in savings (and sometimes losses) based on their performance compared to a defined spending benchmark.
5. Do patients know they are in an ACO?
Patients are attributed to ACOs based on where they get most of their primary care. They are notified but can continue seeing any Medicare provider—they are not locked into a network.
