What are What are LCDs (Local Coverage Determinations) in Healthcare?
Local Coverage Determinations (LCDs) are regional Medicare coverage policies issued by Medicare Administrative Contractors (MACs) to clarify when specific services, procedures, or technologies are considered reasonable and medically necessary for reimbursement. LCDs supplement national Medicare policy by interpreting federal rules within the clinical, demographic, and utilization patterns of each MAC jurisdiction.
LCDs apply to Medicare Part A and Part B services and outline the coverage criteria, clinical indications, documentation standards, coding requirements, and limitations that providers must follow when billing for certain CPT® or HCPCS codes.
While National Coverage Determinations (NCDs) apply uniformly across the U.S., LCDs provide region-specific guidance, allowing MACs to address variations in medical practice and emerging technologies that may not yet be covered by national policy.
An LCD can:
- Define which diagnoses support medical necessity.
- Identify required documentation or test results.
- Specify appropriate CPT/HCPCS codes and modifiers.
- Outline frequency limitations or patient eligibility criteria.
- Clarify non-covered indications.
Although LCDs do not override federal law, they play a central role in daily billing operations, claims adjudication, and audit risk management. Providers must comply with both national policy and their jurisdiction’s LCDs to ensure accurate reimbursement and avoid denials.
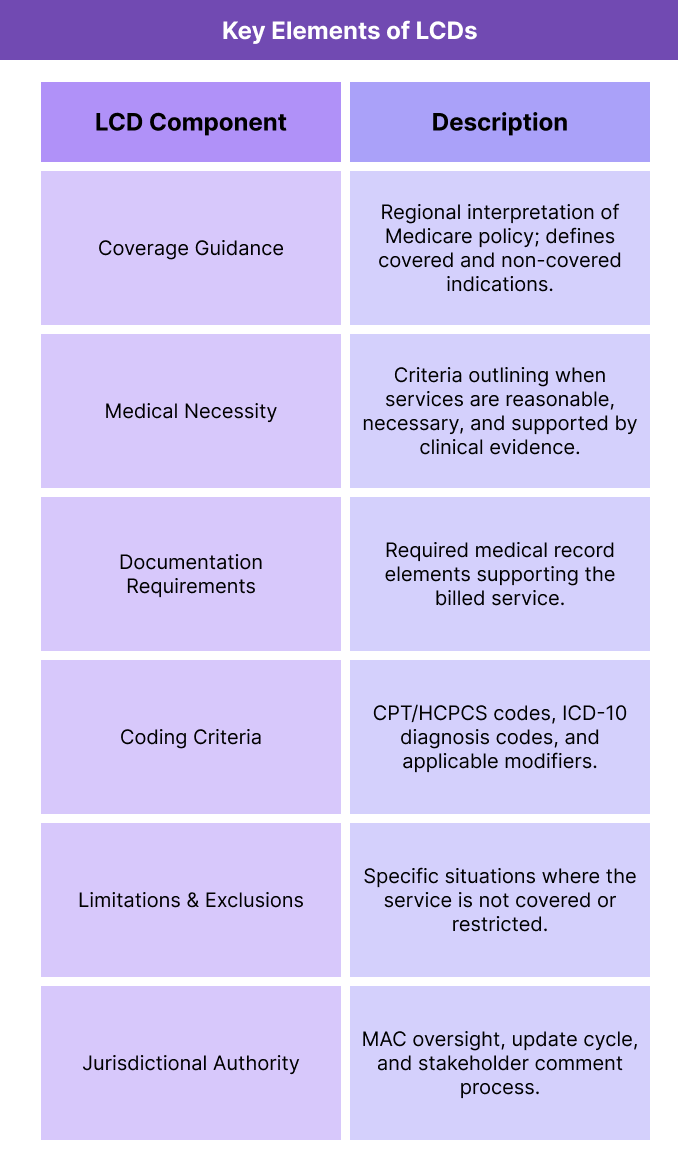
Key Components of Local Coverage Determinations (LCDs)
Local Coverage Determinations (LCDs) outline the specific Medicare coverage rules that apply within each Medicare Administrative Contractor (MAC) jurisdiction. They shape how MACs interpret federal regulations, determine medical necessity, and adjudicate claims for services that lack a National Coverage Determination (NCD).
LCDs contain detailed sections that help providers understand what must be documented, coded, and supported to ensure compliance and reimbursement accuracy.
1. Regional Coverage Guidance
- LCDs reflect jurisdiction-specific medical practice patterns, beneficiary health needs, and utilization trends.
- They supplement national policy when CMS has not issued an NCD for a particular service.
- Each MAC develops and maintains its own LCDs, which means coverage requirements can differ by region.
- When services cross jurisdictional boundaries (e.g., multi-site providers), LCD variation becomes a critical compliance factor.
2. Medical Necessity Requirements
- An LCD defines when and for whom a service is considered medically necessary. This section typically includes:
- Covered indications (diagnoses, severity, clinical rationale).
- Non-covered indications (lack of evidence, experimental use, inappropriate settings).
- Frequency guidelines (how often a service can be billed).
- Clinical decision parameters aligned with accepted standards of care.
- Medical necessity is central to LCD enforcement and drives both claim approval and audit focus.
3. Documentation and Coding Criteria
- LCDs specify the documentation elements that must appear in the medical record to support billing, such as:
- Physician orders, treatment plans, and progress notes.
- Diagnostic test results or clinical measurements.
- Evidence supporting signs, symptoms, or risk factors.
- Coding sections clarify:
- Required CPT®/HCPCS procedure codes.
- Associated ICD-10 diagnosis codes that support coverage.
- Applicable modifiers (e.g., -25, -59, -KX).
- Billing scenarios that require additional justification or attachments.
4. Limitations and Exclusions
- LCDs outline restrictions to ensure compliance and prevent misuse, including:
- Clinical situations where the service is not reasonable or necessary.
- Patient populations where evidence does not support benefit.
- Frequency or duration limits (per day, month, or episode).
- Situations where an NCD takes precedence over the LCD.
- These limitations often form the basis of denials, RAC findings, and TPE reviews.
5. Jurisdictional Authority and Update Process
- LCDs are developed under the authority of each MAC and reviewed through a public, evidence-based process.
- Providers, specialty societies, and stakeholders may submit comments during the LCD open meeting cycle.
- MACs update LCDs to reflect:
- New clinical evidence
- Coding changes
- CMS policy updates
- Audit or utilization trends
- Regular review ensures policies reflect current medical standards and Medicare requirements.
6. Relationship to NCDs, Audits, and Compliance Programs
- LCDs function within the broader CMS coverage ecosystem:
- NCDs override LCDs when national policy exists.
- RACs and UPICs use LCDs as a basis for medical necessity and coverage audits.
- TPE reviews heavily rely on LCD criteria for selecting claims and identifying documentation errors.
- MACs use LCDs to develop claim edits, prepayment validations, and denial messages.
- For providers, LCD compliance is fundamental to avoiding denials, payment delays, or audit findings.
How Local Coverage Determinations (LCDs) Work in Practice
Local Coverage Determinations (LCDs) function as operational rulebooks for Medicare coverage at the regional level.
Every provider billing Medicare Part A or Part B must follow their jurisdiction’s LCDs to ensure that services are covered, medically necessary, and properly documented.
LCDs are referenced at nearly every stage of the revenue cycle—from clinical decision-making to claim submission, denial management, and audits—making them essential tools for providers, coders, compliance officers, and RCM teams.
Step 1: Identifying Whether an LCD Applies
- Before furnishing a service or submitting a claim, providers must determine:
- Whether an LCD exists for the procedure, code set, or diagnostic category.
- Which MAC jurisdiction applies to their practice site.
- Whether a National Coverage Determination (NCD) supersedes local policy.
- Clinicians and coders typically access LCDs through:
- The CMS Medicare Coverage Database (MCD)
- MAC websites and policy libraries
- Internal compliance software or EHR-integrated alerts
- LCDs must be checked regularly because updates occur frequently.
Step 2: Applying Coverage Criteria and Clinical Indications
- If an LCD governs the service, the provider must ensure:
- The patient meets covered indications.
- Any exclusions or non-covered conditions do not apply.
- Clinical criteria (e.g., symptom threshold, failed conservative therapy, frequency limits) are met.
- These requirements guide clinical documentation and influence encounter structure, test ordering, and treatment planning.
Step 3: Documenting to LCD Standards
- LCDs specify the documentation elements required to substantiate medical necessity. Providers must include:
- Physician orders
- Exam findings or diagnostic results
- Clinical rationale supporting necessity
- Previous treatments or failed alternatives
- Time, frequency, or condition-specific evidence
- Coders and auditors rely on these elements to validate that the service meets LCD expectations.
Step 4: Coding and Billing According to the LCD
- LCDs inform the billing team how to code the service, including:
- Accepted CPT®/HCPCS procedure codes
- Required ICD-10 diagnosis codes supporting medical necessity
- Applicable modifiers (e.g., -25, -59, KX)
- Situations requiring additional paperwork or attachments
- When a diagnosis is not listed—or documentation does not justify necessity—claims will likely be denied.
Step 5: Claim Submission and MAC Adjudication
- Once submitted, the claim is processed by the MAC, which:
- Applies LCD criteria to determine coverage
- Validates coding, modifiers, and documentation
- Cross-checks NCD applicability
- Applies any jurisdiction-specific claim edits
- The LCD becomes the MAC’s reference point for approving or denying payment.
Step 6: Handling LCD-Based Denials
- Common LCD-related denial reasons include:
- Diagnosis code not covered
- Clinical indications not met
- Frequency exceeded
- Documentation missing or insufficient
- Non-covered indication
- Providers may respond through:
- Resubmission with corrected coding
- Redetermination with additional documentation
- Appeals if medical necessity was met but denied
- Understanding LCD logic is essential for successful denial overturns.
Step 7: Interpreting LCD Variation Across Regions
- Because each MAC creates its own LCDs:
- Coverage criteria may differ across states or regions.
- Multi-state or national provider organizations must maintain a jurisdiction-specific compliance matrix.
- Workflow engines in EHR/RCM systems often include MAC/LCD rulesets to prevent cross-jurisdictional errors.
- This variation is a major operational factor in large medical groups, specialty practices, and health systems.
Step 8: LCDs in Audits and Program Integrity Reviews
- LCDs are central to federal audit programs:
- For providers, LCD alignment is the single best defense against repeated denials, payment delays, and audit exposure.
LCDs in Billing, Reimbursement, and Compliance Limitations
Local Coverage Determinations (LCDs) play a defining role in Medicare reimbursement, shaping how medical necessity, coding accuracy, and documentation sufficiency are evaluated during claim adjudication.
Because MACs rely on LCDs to validate whether services meet coverage requirements, LCD compliance is central to avoiding denials, ensuring timely payment, and reducing audit exposure.
However, LCD variation across jurisdictions, rapid update cycles, and policy interpretation challenges can introduce administrative complexity—especially for multi-state healthcare organizations or specialties with heavy documentation needs.
How LCDs Influence Medicare Reimbursement
- LCDs directly determine whether a submitted claim is:
- Covered and payable
- Denied for lack of medical necessity
- Flagged for prepayment or postpayment review
- Subject to frequency limitations
- MACs use LCDs to apply:
- Diagnosis-to-procedure validation
- Coverage indications and exclusions
- Documentation expectations
- Bundling or utilization edits
- Even minor deviations from LCD requirements—such as missing test results, incomplete physician notes, or unsupported diagnosis codes—can delay or prevent payment.
Regional Variation and Jurisdictional Challenges
- Because LCDs are developed by individual MACs:
- Providers practicing across multiple states may face different coverage criteria for the same CPT®/HCPCS code.
- Some LCDs include extensive ICD-10 lists; others include only selective indications.
- Documentation or coding requirements may differ between regions.
- Changes in MAC contracts (e.g., jurisdiction shifts) can alter LCD applicability overnight.
- This variation creates operational complexity for:
- National health systems
- Multi-state provider groups
- Telehealth organizations
- DME suppliers and specialty practices
- Maintaining compliance requires ongoing monitoring of jurisdiction-specific LCD libraries.
Limitations in LCD Clarity and Interpretation
- While LCDs aim for consistency, practical limitations include:
- Ambiguous medical necessity language that leaves room for MAC interpretation.
- Frequent updates that may outpace provider education.
- Varying levels of detail—from highly prescriptive to broad and interpretive.
- Gaps where LCDs conflict with specialty guidelines or new evidence.
- Situations where LCDs become outdated relative to emerging clinical standards.
- These issues can lead to inconsistency in claim adjudication, provider confusion, and elevated denial rates.
Impact on Audit Risk and Program Integrity Reviews
- LCDs are heavily used in audit environments:
- TPE reviews often use LCDs as the basis for selecting claims and identifying documentation failures.
- RACs assess medical necessity and coding accuracy against LCD criteria for improper payment identification.
- UPICs reference LCDs during fraud, waste, and abuse investigations.
- CERT audits use LCDs to validate error rates and national payment accuracy.
- Non-compliance with LCDs is one of the most common drivers of:
- Repetitive denials
- Medical record requests
- Postpayment recoupments
- Educational corrective action plans
- LCD alignment is therefore essential for audit readiness and risk mitigation.
- Payment Delays and Administrative Burden
- LCD-driven denials or prepayment edits can create:
- Cash flow delays
- Increased appeals workload
- Additional documentation requests
- Longer revenue cycle timelines
- Providers may need to allocate substantial staff resources to:
- Track varying LCD criteria
- Adjust EHR templates
- Modify clinical workflows
- Train providers on jurisdiction-specific rules
- This administrative burden is especially significant for specialties with intensive LCD coverage (e.g., radiology, laboratory medicine, cardiology, rehab therapy, DME).
Interactions with NCDs and Higher-Level Policy
- LCDs cannot contradict federal Medicare law or National Coverage Determinations (NCDs), but practical conflicts can arise when:
- NCDs are outdated or narrowly scoped.
- MACs interpret emerging clinical evidence differently.
- New technologies lack coordinated national policy.
- In such cases, claims may be approved in one jurisdiction and denied in another, creating inequity in reimbursement and patient access.
Key Takeaway
LCDs are essential tools for Medicare billing and compliance, but they also introduce regional variation, operational complexity, and elevated audit sensitivity.
Providers who embed LCD requirements into clinical workflows, documentation standards, and coding practices experience fewer denials, smoother reimbursement cycles, and significantly lower audit risk.
How LCDs Influence Quality, Access, and Equity in Healthcare
Although Local Coverage Determinations (LCDs) are primarily administrative policies, their real-world impact extends directly into clinical quality, beneficiary access, and regional equity.
By defining when services meet Medicare’s standard of medical necessity, LCDs shape which patients receive diagnostic testing, treatments, or technologies—and whether providers are reimbursed for delivering them.
LCDs therefore play a crucial role in ensuring consistent, evidence-based care, while also presenting challenges when regional variation results in unequal access.
Promoting Quality Through Evidence-Based Coverage
- LCDs are grounded in clinical evidence, specialty society guidelines, and peer-reviewed research.
- MACs are required to evaluate and document the evidence base during LCD development.
- This ensures that services covered under an LCD meet accepted standards for clinical effectiveness, patient safety, and medical necessity.
- Aligning reimbursement with evidence-based practice supports higher-value care and reduces inappropriate utilization.
- LCDs thus serve as a bridge between clinical science and coverage rules, reinforcing quality standards across Medicare.
Regional Variation and Its Impact on Access
- Because LCDs are issued independently by each MAC, their criteria may vary significantly by region. This can lead to:
- Differences in which patients qualify for certain tests or procedures.
- Variability in documentation or diagnosis requirements.
- Unequal utilization patterns for similar patient populations.
- Confusion among providers practicing across multiple states or MAC jurisdictions.
- These disparities may affect:
- Rural providers covered by MACs with more restrictive LCDs
- Multi-state health systems navigating conflicting coverage policies
- Specialty services with high geographic variability in clinical practice
- Regional variation is one of the most significant equity concerns associated with LCDs.
Consistency with National Policy and NCD Frameworks
- LCDs must defer to National Coverage Determinations (NCDs) when they exist, but:
- Many services lack an NCD, leaving coverage to MACs.
- NCDs are updated far less frequently than LCDs.
- Emerging technologies often enter Medicare through LCD pathways first.
- This creates a coverage landscape where national consistency is not always achievable, and beneficiaries in different regions may experience different levels of access for the same service.
Transparency and Public Engagement
- CMS requires MACs to follow a public, evidence-based process when developing new LCDs. This includes:
- Open meetings for stakeholders
- Public comment periods
- Publication of clinical evidence summaries
- Final LCDs posted in the Medicare Coverage Database
- This transparency supports:
- Provider trust
- Consistency in decision-making
- Accountability in coverage criteria
- Opportunities for specialists to influence policy
- Public engagement ensures that LCDs reflect contemporary clinical knowledge and stakeholder input.
- Implications for Vulnerable and Underserved Populations
- LCD-driven variation may disproportionately affect:
- Rural beneficiaries with fewer provider options
- Patients with complex or rare conditions
- Populations served by smaller or resource-limited providers
- Medicaid-Medicare dual-eligibles when LCD rules interact with state Medicaid policies
- When coverage criteria differ across jurisdictions, inconsistent access to diagnostics or treatments can exacerbate regional health disparities.
- CMS monitors these patterns through:
- UPIC and CERT reporting
- MAC performance oversight
Equity-focused modernization initiatives
- LCDs are increasingly reviewed with attention to their equitable application to all Medicare beneficiaries.
- Modernization and Policy Improvement Efforts
- CMS is actively working to reduce coverage variation and improve LCD consistency through:
- Enhanced evidence-sharing across MACs
- Alignment with specialty society guidelines
- Standardized clinical template formats
- Ongoing stakeholder collaboration
- Integration with digital tools for coverage lookup in EHR systems
- These efforts aim to maintain regional flexibility while promoting greater national coherence and fairness in Medicare coverage.
The Equity Imperative for LCDs
LCDs exist at the intersection of clinical evidence, administrative enforcement, and patient access.
When applied consistently and updated regularly, they promote high-quality, medically necessary care.
When uneven or outdated, they can introduce coverage inequities that challenge CMS’s goals of transparency, fairness, and accessibility.
A modernized, evidence-aligned LCD framework is essential to ensuring equitable Medicare coverage for all beneficiaries, regardless of geography.
Frequently Asked Questions about Local Coverage Determinations (LCDs)
1. What is a Local Coverage Determination (LCD)?
A Local Coverage Determination (LCD) is a Medicare coverage policy issued by a Medicare Administrative Contractor (MAC) that defines when a service is considered reasonable and medically necessary within that contractor’s jurisdiction. LCDs outline covered indications, non-covered indications, documentation requirements, coding rules, and billing limitations for specific CPT®/HCPCS codes.
2. How do LCDs differ from NCDs?
National Coverage Determinations (NCDs) apply uniformly across all states and all MAC jurisdictions.
LCDs apply regionally and address services for which CMS has no national policy.
Key differences:
- NCDs override LCDs when both exist.
- LCDs allow for regional interpretation of medical necessity.
- LCDs are updated more frequently and may vary between MACs.
3. How do I find the LCDs that apply to my practice?
You can locate LCDs by searching:
- The CMS Medicare Coverage Database (MCD)
- Your MAC’s website (e.g., NGS, Noridian, WPS, Palmetto, Novitas)
- Internal EHR or compliance software with coverage integration
Always ensure you are viewing the LCD for your jurisdiction, as criteria differ across MACs.
4. How do LCDs impact claim approvals and denials?
MACs reference LCDs during claim adjudication to verify:
- Medical necessity criteria
- Diagnosis-to-procedure alignment
- Documentation sufficiency
- Frequency limits
- Coding and modifier requirements
Failure to meet these criteria will typically result in medical necessity denials or prepayment review requests.
5. How often do LCDs change?
LCDs are updated regularly based on changes in:
- Clinical evidence
- Coding (CPT, HCPCS, ICD-10)
- Utilization trends
- Audit findings
- Stakeholder feedback
Providers should monitor MAC updates frequently, as even minor LCD changes can affect billing workflows and claim outcomes.
6. Can I appeal a denial based on an LCD?
Yes. Providers may appeal LCD-related denials through the standard Medicare appeals process, beginning with a redetermination by the MAC.
Strong documentation—including clear clinical justification and alignment with LCD criteria—is essential for successful appeals.
In some cases, new evidence or specialty guidance may support overturning an LCD-driven denial.
7. Why do LCDs vary across states or regions?
Each MAC develops LCDs independently to reflect local practice patterns, beneficiary needs, and regional resource utilization.
This flexibility allows MACs to address emerging clinical areas, but it can also lead to coverage differences between jurisdictions, especially for newer technologies or specialty procedures.
CMS is working to improve cross-MAC alignment to reduce unnecessary variation.
