What Are ICD-10 Codes?
ICD-10 codes, part of the International Classification of Diseases, Tenth Revision, are a globally standardized set of alphanumeric codes used to document diagnoses, symptoms, and medical conditions. These codes are essential in US healthcare for claim submission, risk adjustment, and quality reporting.
Maintained by the Centers for Medicare & Medicaid Services (CMS) and the National Center for Health Statistics (NCHS), ICD-10 codes must accompany CPT or HCPCS codes on every insurance claim. They help tell the “why” behind a service—identifying the reason a patient was seen, treated, or referred. From chronic illnesses to screenings and social determinants, ICD-10 codes form the diagnostic backbone of billing and care documentation.
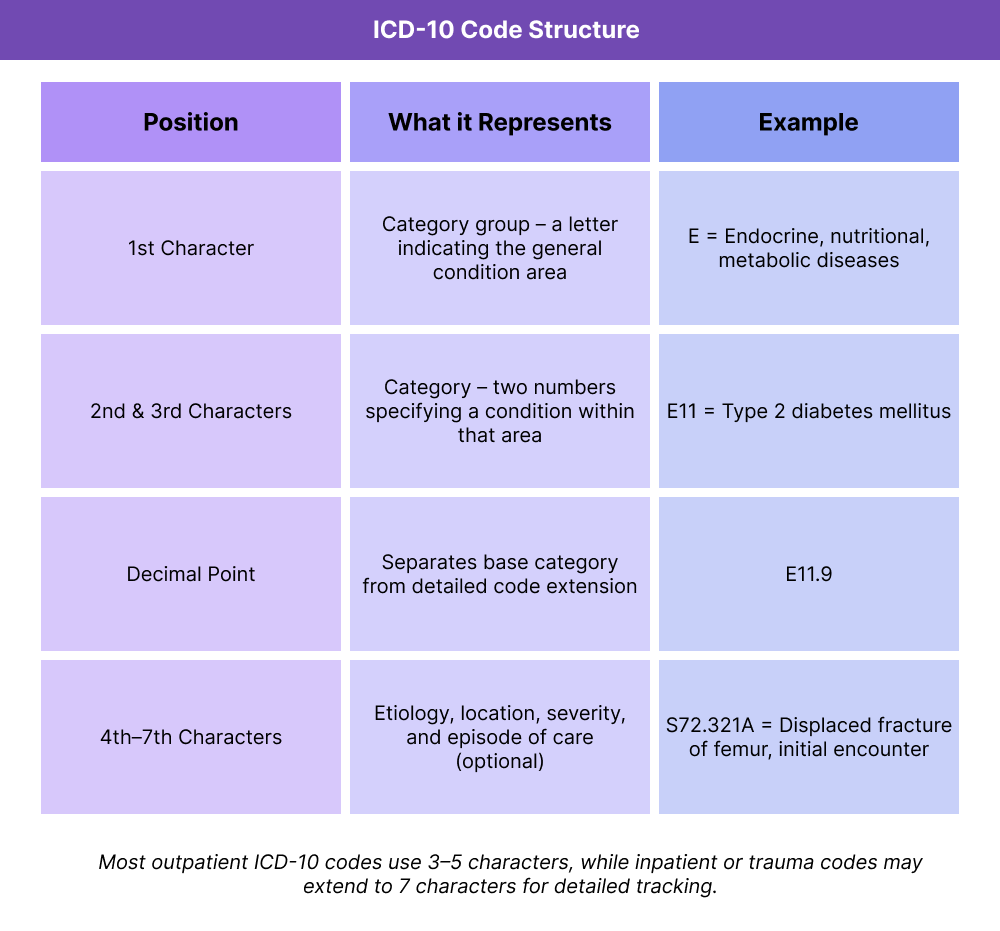
Key Components of ICD-10 Codes
- Stands for: International Classification of Diseases, 10th Revision
- Required for documenting diagnoses, symptoms, and conditions
- Maintained by CMS and NCHS in the United States
- Replaced ICD-9 as of October 1, 2015
- Codes are alphanumeric, starting with a letter and followed by numbers (e.g., E11.9)
- Must appear on insurance claims alongside CPT/HCPCS codes
- Used in billing, audits, quality tracking, and population health analytics
- Supports value-based care and risk stratification (e.g., HCC coding)
How ICD-10 Codes Work in Practice
In healthcare settings, ICD-10 codes serve as the diagnostic counterpart to CPT and HCPCS codes. While CPT describes what was done, ICD-10 codes explain why—capturing the patient’s condition, symptoms, or reason for treatment.
Here’s how they fit into daily workflows:
1. Clinical Documentation
During or after a patient encounter, the provider documents any diagnoses, conditions, or reasons for the visit in the electronic medical record (EMR). These details are then used to assign appropriate ICD-10 codes.
2. Code Selection
ICD-10 codes are either:
- Auto-suggested by the EMR based on charting inputs
- Manually selected by providers or coding staff
For example, a patient with poorly controlled diabetes might be assigned E11.65, not just E11.9 — indicating a higher complexity level.
3. Claims and Risk Scoring
On insurance claims, ICD-10 codes:
- Justify the CPT/HCPCS codes being billed
- Determine medical necessity
- Contribute to Hierarchical Condition Category (HCC) scoring for Medicare risk adjustment
4. Quality Programs and Reporting
ICD-10 codes feed into:
- HEDIS measures
- CMS quality reporting
- Public health tracking
- Population health tools
Billing and Documentation Rules for ICD-10 Codes
ICD-10 codes are essential for validating reimbursement. Every medical claim — whether submitted to Medicare, Medicaid, or a private payer — must include at least one diagnosis code from the ICD-10 system. These codes justify the medical necessity of the procedures or services being reported with CPT or HCPCS codes.
Key Billing Guidelines for ICD-10s:
- ICD-10 codes are required on all institutional (UB-04) and professional (CMS-1500) claims.
- At least one ICD-10 diagnosis must be linked to each CPT/HCPCS code on the claim.
- Providers should assign the most specific code available (e.g., E11.65 instead of E11.9) to reflect disease complexity.
- Z codes can be used for social determinants of health (e.g., housing insecurity, caregiver strain) when relevant.
- HCC-relevant codes (e.g., diabetes with complications, CHF, COPD) affect risk adjustment and may trigger care management eligibility.
- Common documentation gaps include unspecified codes, mismatched diagnoses, or missing laterality — all of which can lead to denials or downcoding.
Important to Note: Proper ICD-10 usage isn’t just about billing — it also improves patient targeting for CCM, PCM, TCM, and other reimbursable care programs.
Frequently Asked Questions about ICD-10 Codes
1. What are ICD-10 codes?
ICD-10 codes are alphanumeric codes used to classify medical diagnoses, symptoms, and conditions. They are required for billing and quality reporting across U.S. healthcare systems.
2. What does ICD-10 stand for?
ICD-10 stands for International Classification of Diseases, Tenth Revision. It’s the global standard for diagnostic coding, maintained in the U.S. by CMS and NCHS.
3. What’s the difference between ICD-10 and CPT codes?
ICD-10 codes explain why a patient was seen (their condition or diagnosis), while CPT codes describe what was done during the visit (procedures or services).
4. Are ICD-10 codes used in outpatient billing?
Yes. ICD-10 codes are used in both inpatient and outpatient billing, including primary care, specialty clinics, and care management programs like CCM or PCM.
5. Do ICD-10 codes affect reimbursement?
Yes. ICD-10 codes are used to justify billed services and can impact claim approval, risk adjustment scoring, and quality measure performance. Accurate diagnosis coding is essential for getting paid — especially under value-based care models.
