What Are Current Procedural Technology (CPT) Codes?
Current Procedural Terminology (CPT) codes are a standardized system used to describe and document medical procedures, diagnostic services, and outpatient care. Maintained by the American Medical Association (AMA), CPT codes play a critical role in how healthcare providers report services, bill payers, and track performance across clinical and administrative workflows.
CPT codes are required for billing Medicare, Medicaid, and commercial insurers, and they form the foundation of medical coding systems used in electronic medical records (EMRs), revenue cycle management (RCM) tools, and quality reporting programs. Each code corresponds to a specific service — such as an office visit, lab test, or care management activity—and includes accompanying rules, modifiers, and classifications.
Key Components of CPT Codes
- Developed and maintained by the American Medical Association (AMA)
- Standardized 5-digit codes for reporting medical services and procedures
- Required on insurance claims for Medicare, Medicaid, and private payers
- Used across clinical documentation, billing, auditing, and analytics
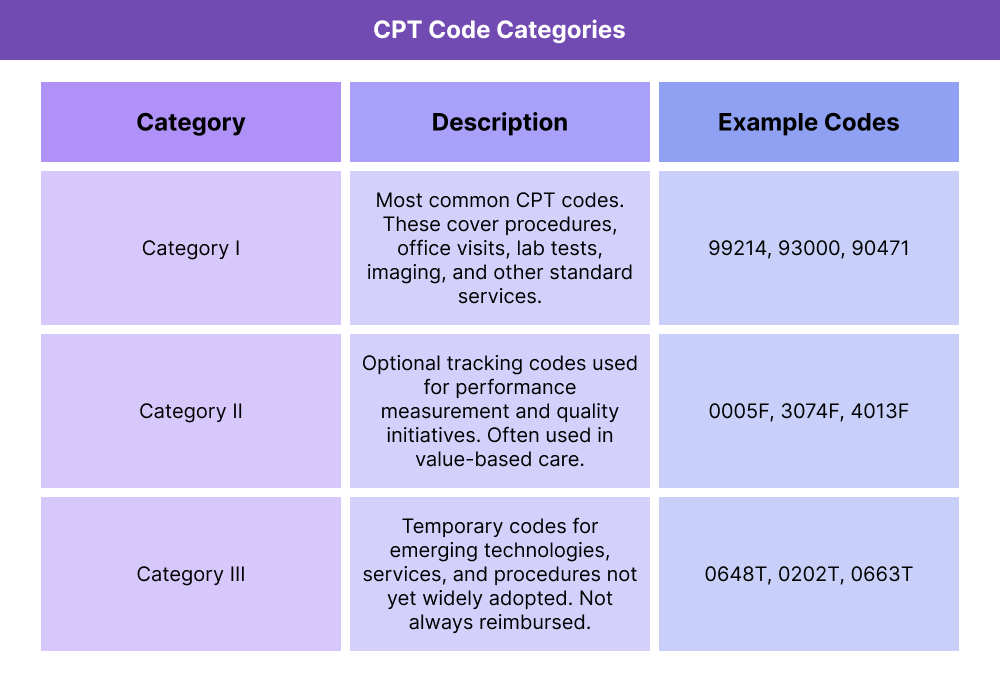
- Organized into three code categories:
- Category I – Routine services and procedures (e.g., 99214)
- Category II – Quality and performance tracking (optional)
- Category III – Emerging or experimental technologies
- Codes may be modified using two-digit suffixes (e.g., -25, -59) to describe unique circumstances
- Updated annually to reflect clinical and regulatory changes
How CPT Codes Work in Practice
In everyday healthcare settings, CPT codes are the linchpin of how clinical services get documented, billed, and reimbursed. While they may seem administrative, these codes drive a large portion of how providers get paid — especially in outpatient and ambulatory care settings.
Here’s how CPT codes function in real-world workflows:
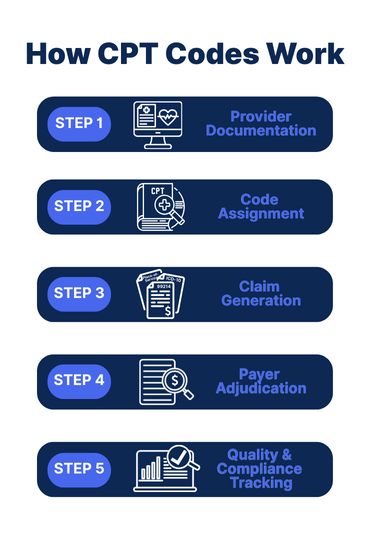
1. Provider Documentation
After a patient encounter, a provider (or their care team) documents the services rendered in the electronic medical record (EMR). This includes the visit type, any procedures performed, screenings ordered, and care management delivered.
2. Code Assignment
The appropriate CPT code(s) are assigned to match the services documented. This may be done:
- Automatically via EMR logic
- Manually by the provider
- Or by coding staff using supporting documentation
Modifiers (e.g., -25 for significant, separately identifiable services) may be added to clarify service details.
3. Claim Generation
The selected CPT codes are bundled with diagnosis codes (ICD-10) and place-of-service codes to create a complete claim.
This is submitted to:
- Medicare
- Medicaid
- Private payers
- Or clearinghouses on behalf of providers
4. Payer Adjudication
Payers use CPT codes to determine:
- Reimbursement amount
- Whether services were covered and medically necessary
- Whether additional documentation or prior authorization is required
5. Quality & Compliance Tracking
Beyond billing, CPT codes also feed into:
- Risk scoring models
- HEDIS and quality measures
- Population health analytics
- Audits and compliance reports
CPT Code Modifiers Explained
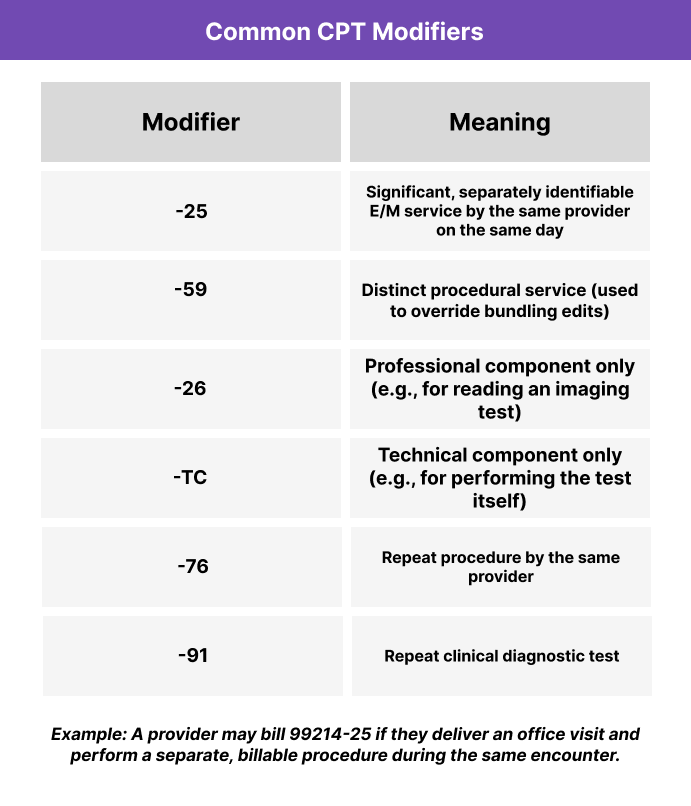
CPT modifiers are two-character suffixes (numeric or alphanumeric) that provide additional detail about a service or procedure. They help explain circumstances that may affect how a procedure was performed, why it was distinct, or why multiple services were reported together.
Modifiers ensure that the billing reflects the clinical reality — especially when:
- The same service was performed multiple times
- A procedure was altered due to patient condition
- Services were performed separately but on the same day
Frequently Asked Questions about CPT Codes
1. What are CPT codes?
CPT codes, or Current Procedural Terminology codes, are standardized five-digit codes developed by the American Medical Association (AMA) to document and bill medical procedures and services.
2. What does CPT stand for in healthcare?
CPT stands for Current Procedural Terminology. It is the most widely used coding system for reporting services to Medicare, Medicaid, and commercial payers.
3. Who uses CPT codes?
CPT codes are used by:
- Physicians and other healthcare providers
- Medical coders and billers
- Health IT platforms and EHRs
- Payers like Medicare, Medicaid, and insurance plans
4. What are CPT modifiers?
CPT modifiers are two-digit suffixes (e.g., -25, -59) added to CPT codes to indicate that a service was changed or delivered in a unique way. They provide more context for claims and help prevent billing denials.
5. Are CPT codes the same as ICD-10 codes?
No. CPT codes describe what was done (procedures/services), while ICD-10 codes describe why it was done (diagnosis or condition). Both are typically required on claims.
