What are CoPs (Conditions of Participation) in Healthcare?
Conditions of Participation (CoPs) are the core health, safety, and operational standards that healthcare providers must meet to participate in the Medicare and Medicaid programs. CoPs establish the minimum requirements CMS uses to determine whether an organization is eligible to receive federal reimbursement. They apply across a wide range of provider types, including hospitals, skilled nursing facilities, home health agencies, and hospices.
CoPs are designed to ensure that organizations deliver care in a way that protects patients and supports consistent quality. They cover areas such as patient rights, quality assessment and performance improvement, infection prevention, staffing, governance, medical records, and emergency preparedness. Because CoPs are tied to participation, failure to meet them can result in citations, corrective action plans, or loss of certification.
In practice, CoPs function as the baseline compliance framework for Medicare reimbursement. They guide how providers structure policies, manage clinical operations, document care, and prepare for CMS surveys. For healthcare SaaS buyers, CoPs matter because they shape the operational and documentation standards that technology must support to keep reimbursement stable and audit exposure low.
Key Components of CoPs in Healthcare
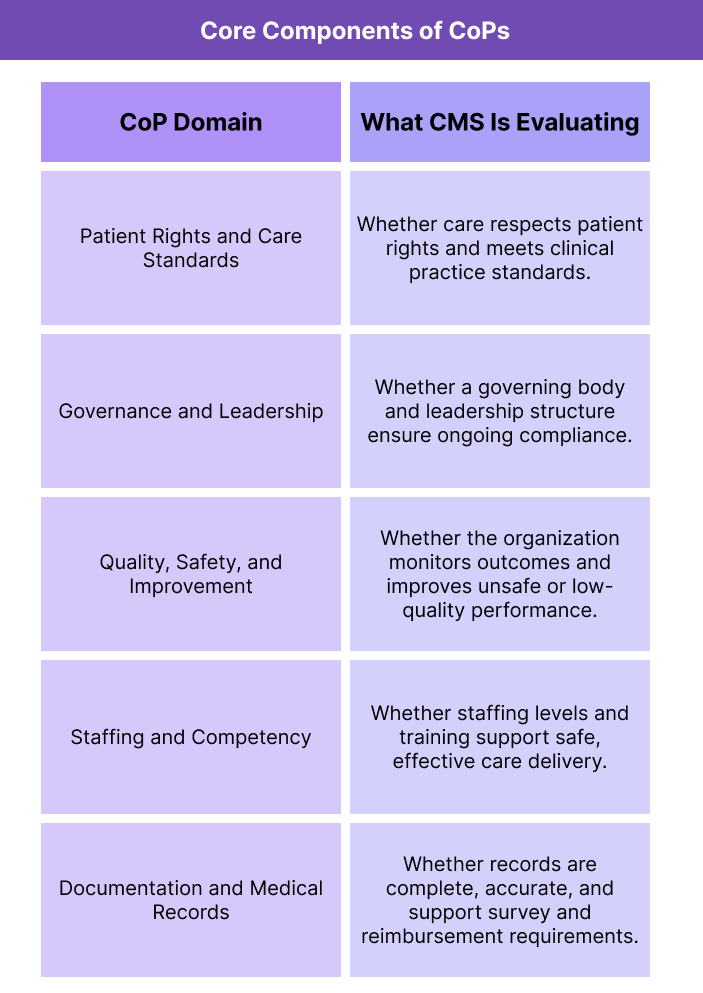
CoPs are designed to create a consistent national baseline for safe, high-quality care before Medicare or Medicaid reimbursement is allowed. CMS uses CoPs to evaluate whether providers have the structure, staffing, and clinical systems needed to deliver care reliably across settings. Because the standards are broad, CoPs apply to both direct patient care and the operational infrastructure that supports it.
While each provider type has its own CoP set, most CoPs share the same core domains.
Patient Rights and Care Standards in CoPs
CoPs require providers to protect patient rights and deliver care that meets professional standards. This typically includes informed consent practices, nondiscrimination, respect for patient autonomy, and clinically appropriate assessment and treatment.
Governance, Leadership, and Accountability Under CoPs
CMS expects clear leadership oversight and accountability for compliance. CoPs often require governing bodies to approve policies, ensure resources are available, and monitor whether the organization is meeting participation standards consistently.
Quality, Safety, and Continuous Improvement Expectations
CoPs include quality and safety requirements that push organizations to measure performance, prevent harm, and improve outcomes. This is where CoPs frequently intersect with programs like Quality Assurance and Performance Improvement (QAPI) in regulated settings.
Staffing, Competency, and Scope Requirements
CoPs specify that providers must have sufficient qualified staff to meet patient needs and that competency is maintained through training and oversight. Staffing expectations vary by setting but remain a core compliance requirement across provider types.
Documentation, Medical Records, and Operational Controls
CoPs require complete, accurate medical records and operational documentation to support continuity of care, survey readiness, and reimbursement integrity. This domain often drives B2B software requirements around charting, care plans, and audit trails.
How CoPs Work in Practice
CoPs operate as the practical rulebook CMS uses to decide whether a provider can bill Medicare and Medicaid. They are enforced through surveys and ongoing oversight, and they shape day-to-day clinical and operational workflows long before a claim is ever submitted.
Step 1: CoPs Define Participation Eligibility
Before a provider can participate in Medicare or Medicaid, it must show that it meets the CoPs for its provider type. CMS (or a delegated survey agency) evaluates whether the organization has the policies, staffing, clinical systems, and governance structure needed to safely deliver care.
Step 2: Surveys Measure Real-World Compliance
CoPs are not just policy standards — they are measured in practice through CMS surveys. Surveyors review medical records, observe care delivery, interview staff and patients, and test whether the provider’s workflows match CoP requirements.
If gaps are found, CMS may issue citations that require corrective action and future follow-up.
Step 3: CoPs Drive Operational and Documentation Systems
Because CoPs cover areas like care planning, patient rights, staffing oversight, infection control, and emergency readiness, they influence how organizations design workflows and documentation. This is why technology platforms supporting regulated care programs need to align with CoP expectations.
For example, software used in regulated environments often must support:
- Audit-ready documentation and clinical traceability
- Standardized care planning and follow-up workflows
- Clear role-based accountability and escalation paths
- Performance monitoring that feeds improvement work
Step 4: Ongoing Compliance Protects Billing Continuity
Once certified, providers must continuously meet CoPs to keep participation status active. CoP failures don’t just create survey citations — they can trigger payment suspensions, termination risk, or loss of certification if unresolved.
That’s why CoPs function as a living compliance framework, not a one-time licensing checkpoint.
CoPs in Billing, Reimbursement, and System Limitations
CoPs are not billing rules, but they are a prerequisite for billing because Medicare and Medicaid reimbursement depends on maintaining active participation status. If a provider fails to meet CoPs, CMS can issue citations, require corrective action, or in more serious cases suspend payments or terminate certification. That makes CoPs a direct driver of reimbursement stability.
How CoPs Affect Medicare and Medicaid Payment
CoPs establish the baseline operational and clinical standards a provider must maintain to remain eligible for federal reimbursement. When survey findings show CoP noncompliance, downstream billing impacts can include:
- Delayed or suspended payments while deficiencies are corrected
- Heightened oversight that increases audit exposure
- Risk to certification status that can stop Medicare billing entirely
- Payer confidence issues that affect commercial contracting
Because of this, organizations often treat CoPs as a revenue-protection framework. Stable compliance ensures claims can flow without participation interruptions.
How CoPs Shape Regulated Workflow Requirements
CoPs influence how providers must document and deliver care. Systems that support Medicare-funded services need to align with CoP expectations around documentation quality, care planning, staffing accountability, and safety processes. If workflows or records cannot demonstrate CoP compliance, survey risk increases, even if billing is otherwise accurate.
- System Limitations and Compliance Watch-Outs
- CoPs are broad standards, and organizations often struggle with implementation because:
- CoP requirements vary by provider type and service setting
- Policies may be written to CoPs but not practiced consistently
- Documentation systems may not capture proof of compliance cleanly
- Improvement work may be siloed instead of organization-wide
Technology can help operationalize and track CoP-driven workflows, but compliance ultimately depends on consistent real-world execution, not just documentation.
How CoPs Influences Quality, Access, and Equity in Healthcare
CoPs are designed to protect patient safety and ensure a minimum standard of care across all Medicare and Medicaid participating providers. Because they govern quality, staffing, patient rights, and operational readiness, CoPs shape the daily conditions under which care is delivered, which directly affects outcomes and access.
How CoPs Improve Care Quality and Safety
CoPs enforce standardized expectations for safe, effective care. Requirements around infection control, care planning, medication oversight, emergency preparedness, and patient rights help reduce preventable harm and ensure organizations maintain reliable clinical systems.
CoPs also reinforce continuous quality improvement by requiring providers to track performance, respond to safety events, and correct systemic issues.
How CoPs Support Patient Access
Participation in Medicare and Medicaid is a core access pathway for many patients. When providers maintain CoP compliance, they preserve certification and remain available to serve covered populations. When CoP failures lead to payment suspensions or certification loss, access can shrink quickly, especially in settings where alternatives are limited.
Equity Implications of CoP Compliance
CoPs help reduce variation in care quality across regions and provider types by setting universal participation standards. This is especially important for communities that rely heavily on Medicare and Medicaid coverage. When CoPs are enforced consistently, they help ensure that vulnerable populations receive care in environments that meet basic safety and quality expectations.
Frequently Asked Questions about CoPs
1. What are CoPs (CMS Conditions of Participation)?
CMS Conditions of Participation (CoPs) are the minimum health, safety, and operational standards providers must meet to participate in Medicare and Medicaid and receive reimbursement.
2. Who do CoPs apply to?
CoPs apply to Medicare- and Medicaid-participating provider types such as hospitals, skilled nursing facilities, home health agencies, hospices, and other certified organizations. Each setting has its own CoP set.
3. How are CoPs enforced?
CoPs are enforced through CMS surveys. Surveyors review records, observe care, and interview staff to determine whether real-world workflows meet CoP requirements. Deficiencies can lead to citations and corrective action.
4. What happens if a provider is out of compliance with CoPs?
Noncompliance can result in survey citations, required corrective plans, increased oversight, payment suspensions, or termination of Medicare or Medicaid certification in severe cases.
5. Are CoPs the same as Conditions for Coverage (CfCs)?
No. CoPs apply to provider participation standards, while Conditions for Coverage (CfCs) apply to certain supplier or facility types under different regulatory structures. Both affect reimbursement eligibility, but they are distinct CMS frameworks.
6. How do CoPs relate to QAPI?
CoPs often include quality and safety requirements that expect providers to monitor outcomes and improve performance. In many settings, CoPs explicitly require an active QAPI program to demonstrate continuous quality improvement.
7. Why do CoPs matter for billing?
CoPs are not billing rules, but they are a prerequisite for billing because Medicare and Medicaid reimbursement depends on maintaining participation status. CoP failures can disrupt payment.
