CPT 99458 Description, Billing Rules, & Use Cases
CPT 99458 is used to report each additional 20-minute block of provider-delivered remote care management under a Remote Physiologic Monitoring (RPM) or Remote Therapeutic Monitoring (RTM) program.
It serves as an add-on code to CPT 99457, extending reimbursement when treatment management exceeds the initial 20-minute threshold.
What is CPT Code 99458?
CPT 99458 represents incremental treatment management time beyond the first 20 minutes billed under CPT 99457.
It may be used in RPM or RTM programs when a physician or qualified healthcare professional (QHP) spends an additional 20 minutes or more providing remote care management during a 30-day period.
This code applies to:
- Continued monitoring and clinical decision-making
- Follow-up communication or patient coaching
- Reviewing extended data streams, symptom trends, or therapy adherence
- Adjusting care plans or coordinating with other providers
Important: CPT 99458 may only be billed in conjunction with 99457 — it cannot be reported as a standalone code.
There is no hard limit on how many units of 99458 may be used per month, but time must be clearly documented and medically necessary.
CPT 99458 Time Thresholds and Code Combinations
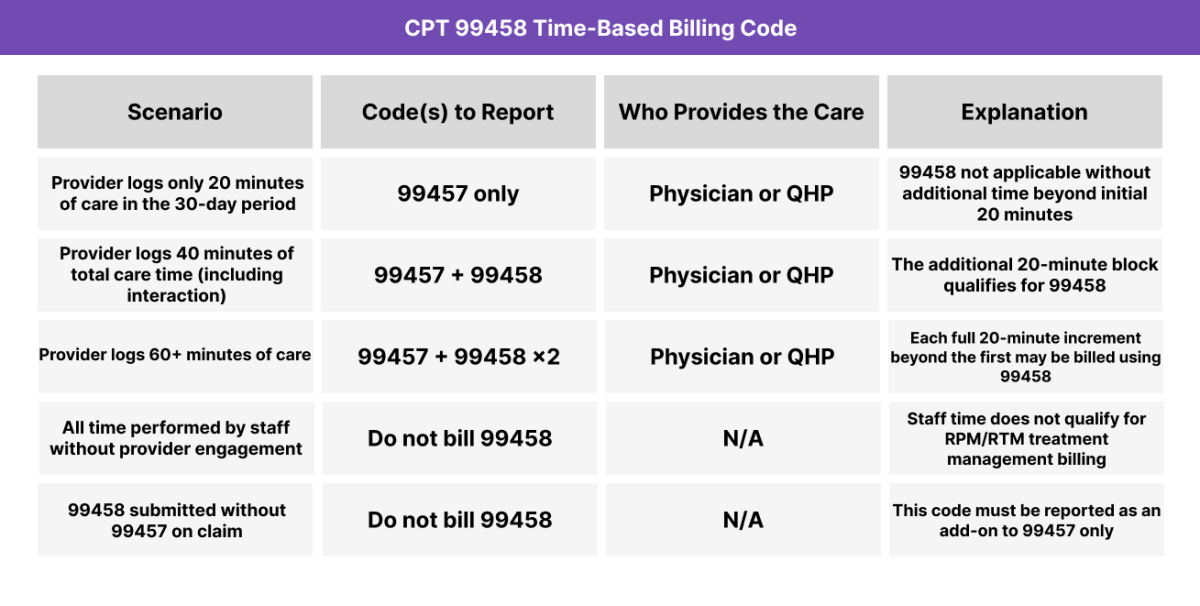
CPT 99458 may be reported for each additional 20-minute block of treatment management time that follows the first 20 minutes billed under CPT 99457. It is a stackable code, meaning multiple units may be billed if medically necessary — as long as time is documented and linked to actionable provider activity.
Important to Note:
- 99458 cannot be billed unless CPT 99457 is also reported in the same month
- Each unit of 99458 must reflect a full 20-minute increment of provider-performed care
- There is no absolute limit to the number of times it may be used, but time and medical necessity must be clearly documented
When to Use CPT 99458: Common Scenarios and Use Cases
CPT 99458 is used when a provider delivers extended remote treatment management as part of RPM or RTM, exceeding the first 20-minute threshold billed under CPT 99457. Each additional 20-minute block must be medically necessary and clearly documented.
Here are examples of how CPT 99458 is used in practice:
CPT 99458 Billing Requirements and Eligibility
CPT 99458 is a time-based add-on code used to extend reimbursement when a provider delivers more than 20 minutes of remote care management under RPM or RTM in a 30-day period. It cannot be billed on its own — it must always follow a claim for CPT 99457.
This code allows physicians and QHPs to be reimbursed for additional, medically necessary time, provided it’s properly tracked and documented.
Patient Eligibility Criteria
The patient must:
- Be enrolled in a qualified RPM or RTM program
- Be actively using a transmitting medical or therapeutic device
- Have data and care complexity that justify extended management time
- Receive ongoing treatment management from the billing provider or QHP
99458 is most often used when:
- A patient has high-risk or unstable clinical status
- There are frequent data anomalies or symptom reports
- Medication or therapy adjustments require multiple touchpoints
- Multiple communication sessions occur during a single billing cycle
Service and Time Requirements
To bill CPT 99458:
- The first 20 minutes must be reported with CPT 99457
- Each additional 20-minute increment may be reported with a unit of 99458
- Time must be:
- Personally performed by a physician or QHP
- Distinct from CPT 99457
- Cumulative, with exact time tracked and documented
Qualifying activities include:
- Data review and clinical interpretation
- Symptom or trend analysis
- Additional interactive communication
- Patient education, behavioral coaching, or lifestyle planning
- Coordination with external care providers
Who can Bill CPT 99458
CPT 99458 must be:
- Personally delivered by a physician or QHP
- Staff-only time is not billable under this code
- The total time must be distinct from general care coordination or messaging
Billing Frequency and Time Requirements
- CPT 99458 may be billed multiple times per 30-day cycle as justified
- It must follow a 99457 claim for the same billing period
- May be combined with:
- RPM setup and supply (99453, 99454)
- RTM setup and supply (98975–98977)
- Only one provider group may bill per patient per month
CPT 99498 Billing Documentation Checklist
To support proper billing of CPT 99458, the following must be documented in the patient’s medical record:
- A previously billed CPT 99457 for the same 30-day period:
- 99458 may not be reported alone
- Must clearly follow an eligible treatment management cycle
- Cumulative time tracking for each 20-minute increment beyond 99457:
- Personally performed by the physician or QHP
- May be tracked using cumulative logs or start/stop time documentation
- Clearly separated from non-billable administrative or clinical staff activity
- Description of billable care management services performed:
- Interpretation of transmitted physiologic or therapeutic data
- Communication of findings to the patient or caregiver
- Modification of the treatment or monitoring plan
- Care team coordination or patient behavioral coaching
- Documentation of interactive communication (if applicable to the additional time):
- Date, format (phone, video), and content summary
- Must reflect clinical relevance and time contribution
- Provider credentials and attestation:
- Billing limits and claim consistency:
- Only one provider or group may bill for RPM/RTM management during a 30-day cycle
- 99458 units reflect medically necessary extended care, not routine data monitoring
Common CPT 99458 Billing Mistakes (and How to Avoid Them)
❌ Billing Without CPT 99457
CPT 99458 is an add-on code and cannot be billed on its own. If 99457 is not also billed in the same month, the claim for 99458 is invalid.
❌ Underestimating the Time Threshold
Each unit of 99458 represents a full additional 20 minutes of provider-led care. Partial time (e.g., 35 total minutes) still qualifies for only 99457.
❌ Including Clinical Staff Time
Only time personally performed by a physician or QHP may count. Time spent by nurses, assistants, or technicians may not be included toward the threshold.
❌ Duplicate Billing or Overuse
Billing 99458 multiple times without supporting time logs or without clinical justification can raise red flags. Ensure documentation supports each unit as medically necessary.
❌ Lack of Distinct Documentation
Claims must clearly show:
- A full 20 minutes of additional care
- Specific tasks performed
- Date(s) of service and total time
- Separation from the time already counted under CPT 99457



