CPT 98015 Description, Billing Rules, & Use Cases
CPT 98015 is used to bill for a synchronous audio-only evaluation and management (E/M) service with an established patient that involves high-complexity medical decision making (MDM) or at least 40 minutes of total provider time on the date of the encounter.
Introduced in 2025 as the highest level in the audio-only telehealth E/M code set (98008–98015), CPT 98015 replaced the upper tier of the discontinued telephone codes (99441–99443). It is used for encounters requiring extended time, intensive clinical reasoning, and management of serious or unstable conditions.
The service typically includes:
- Management of multiple or worsening chronic conditions with significant risk
- Review and synthesis of extensive medical data and test results
- Adjustment or initiation of complex treatment plans or medication regimens
- Care coordination involving multiple specialists or care settings
- Patient or caregiver counseling for high-risk clinical scenarios
- Documentation of in-depth medical reasoning and follow-up planning
Billing Notes:
- Use for established-patient audio-only E/M visits requiring high-complexity MDM or ≥40 minutes of provider time.
- The provider must personally perform the entire service using real-time, two-way audio-only communication.
- The visit cannot overlap with an in-person or audio-video E/M service on the same date.
- Documentation must include patient consent, audio-only modality, and total time or MDM level used for code selection.
- Encounters lasting 61 minutes or longer should include CPT 99417 (prolonged services).
What Is CPT Code 98015?
CPT 98015 is an evaluation and management (E/M) code for audio-only telemedicine visits with established patients that require high-complexity medical decision making (MDM) or at least 40 minutes of total provider time on the date of service.
Introduced in 2025, CPT 98015 is part of the audio-only E/M series (98008–98015), which replaced the deleted telephone codes (99441–99443). This code represents the highest level of complexity for established-patient audio-only encounters, reserved for cases that require comprehensive data review, significant clinical judgment, and management of serious or unstable conditions.
Key points about CPT 98015:
- Used for established-patient audio-only visits requiring high-complexity MDM or ≥40 minutes of provider time.
- Must include a medically appropriate history and/or examination as determined by the provider.
- Communication must be real-time and synchronous (not prerecorded or message-based).
- Appropriate for patients with multiple uncontrolled or life-impacting conditions requiring complex management.
- The visit must be personally performed by a qualified healthcare provider (physician, NP, or PA).
- Cannot be billed on the same date as an in-person or audio-video E/M encounter.
In summary: CPT 98015 captures high-complexity audio-only telehealth visits for established patients, where the provider spends at least 40 minutes performing in-depth evaluation, medical decision-making, and care coordination using real-time verbal communication.
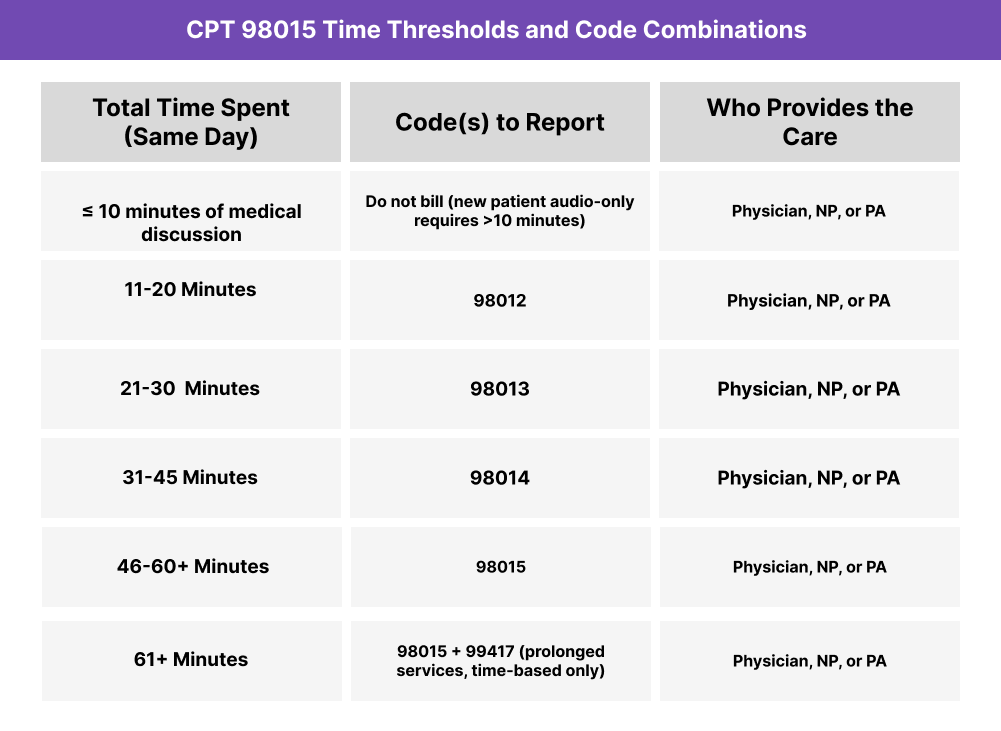
CPT 98015 Time Thresholds and Code Combinations
CPT 98015 represents a synchronous audio-only evaluation and management (E/M) service for an established patient that involves high-complexity medical decision making (MDM) or at least 40 minutes of total provider time on the date of service.
Understanding the Time Component
When selecting by time, the provider must personally spend 40 minutes or more performing the encounter and associated medical work on the same date of service.
Included time may involve:
- Reviewing extensive patient data, medical records, and test results prior to or during the encounter
- Conducting an in-depth audio-only evaluation with complex decision-making
- Coordinating with multiple specialists, facilities, or care teams
- Counseling patients or caregivers regarding treatment risks and next steps
- Documenting the encounter, assessment, and treatment plan in the medical record
If total time is less than 40 minutes, report CPT 98014.
Encounters that exceed 60 minutes may include CPT 99417 (prolonged services) to capture the additional time.
Understanding the MDM Component
When coding by medical decision making, documentation must demonstrate high complexity, including:
- Multiple chronic or severe conditions requiring intensive management
- Extensive data review and interpretation across multiple sources or modalities
- High risk of morbidity, mortality, or treatment complications due to decision-making or condition severity
When to Use CPT 98015: Common Scenarios and Use Cases
CPT 98015 is appropriate when a physician, nurse practitioner (NP), or physician assistant (PA) provides a synchronous audio-only evaluation and management (E/M) visit with an established patient that involves high-complexity medical decision making (MDM) or at least 40 minutes of total provider time on the same date.
Here are examples of how CPT 98015 is used in practice:
CPT 98015 Billing Requirements and Eligibility
CPT 98015 is used to report a synchronous audio-only evaluation and management (E/M) visit with an established patient that involves high-complexity medical decision making (MDM) or at least 40 minutes of total provider time on the date of service.
This code represents the highest level of established-patient audio-only E/M services introduced in 2025, replacing the upper tier of the discontinued telephone visit codes (99441–99443).
Patient Eligibility
To qualify for CPT 98015:
- The patient must be established (seen by the same provider or group within the past three years).
- The encounter must occur via real-time, two-way audio-only communication (no video).
- The patient must consent verbally to receiving telehealth services via audio-only technology.
- The visit must involve high-complexity MDM or ≥40 minutes of total provider time.
- The service must not occur on the same calendar day as an in-person or audio-video E/M encounter.
Provider Eligibility
The encounter must be personally performed by a physician, nurse practitioner (NP), or physician assistant (PA) qualified to bill E/M services.
The provider must:
- Conduct the entire encounter personally using real-time, audio-only communication.
- Document the total time spent or MDM level used for code selection.
- Record the modality (audio-only) and patient consent clearly in the note.
- Provide a comprehensive clinical assessment and plan aligned with E/M standards.
Service Requirements
- Minimum provider time: 40 minutes on the date of service.
- Countable time includes chart review, patient discussion, clinical reasoning, care coordination, and same-day documentation.
- Non-countable time includes scheduling, administrative work, or communications unrelated to the encounter.
- May be selected by time or MDM, but documentation must support the higher standard.
- Must include follow-up planning and care coordination as appropriate for high-risk or complex cases.
Documentation Requirements
The visit note must clearly include:
- Start and end time, or total provider time (≥40 minutes).
- Patient consent for audio-only telehealth care.
- Statement of modality (e.g., “audio-only synchronous communication, no video used”).
- Chief complaint or reason for visit.
- High-complexity MDM elements, including:
- Problems: Multiple chronic or acute conditions posing a high risk of morbidity or mortality.
- Data: Extensive review of tests, labs, specialist reports, or care coordination documentation.
- Risk: High risk from management decisions, diagnostic uncertainty, or treatment complexity.
- Clinical summary detailing findings, decisions, and next steps.
- Provider attestation confirming personal performance and documentation accuracy.
- Non-duplication statement verifying that no other E/M service (in-person or video) occurred on the same date.
Medicare and Payer Coverage Notes
- Medicare: CPT 98015 currently has a status indicator “I” (invalid for Medicare billing).
- Commercial payers: May adopt CPT 98015 for reimbursement under RBRVS valuation.
- Action: Verify payer-specific audio-only telehealth policies, as coverage and parity vary by state and insurer.
CPT 98015 Billing Documentation Checklist
To support compliant billing for CPT 98015, documentation must verify that the encounter was a real-time, audio-only telehealth visit with an established patient, requiring high-complexity medical decision making (MDM) or at least 40 minutes of total provider time.
Your encounter record should include:
- Patient consent for audio-only telehealth, documented at the start of the encounter.
- Verification of patient identity using at least two identifiers (e.g., name and date of birth).
- Provider credentials and role (physician, NP, or PA) clearly documented.
- Statement of modality confirming “audio-only synchronous communication” (no video used).
- Chief complaint or reason for visit describing the presenting condition(s).
- Total provider time documented as ≥40 minutes, including:
- Exact start and end times, or
- Total duration for all qualifying activities on the date of service.
- High-complexity MDM documentation, demonstrating:
- Problems: Multiple serious or unstable chronic conditions, or a high-risk acute issue.
- Data: Extensive review and interpretation of tests, labs, and external records.
- Risk: High risk of morbidity, mortality, or treatment complications.
- Summary of clinical discussion, including:
- Patient-reported findings and key information obtained via audio discussion.
- Provider’s assessment, decision-making rationale, and treatment plan.
- Coordination with other providers, facilities, or caregivers if applicable.
- Provider attestation confirming personal performance and accuracy of documentation.
- Non-overlap statement verifying that no other E/M (in-person or video) was billed on the same date.
- Follow-up plan documented, including next visit interval, labs, or care management activities.
Common CPT 98015 Billing Mistakes (and How to Avoid Them)
❌ Billing Without 40 Minutes of Documented Time
When coding by time, providers must clearly record at least 40 minutes of total provider time on the date of service. Encounters lasting less than this threshold should be billed as CPT 98014 (31–45 minutes) or a lower code.
❌ Missing High-Complexity MDM Justification
If coding by MDM instead of time, documentation must show high complexity — such as multiple serious or unstable conditions, extensive data review, or high-risk management decisions.
❌ Failing to Specify Audio-Only Modality
Each note must explicitly state that the encounter was performed via audio-only synchronous communication. Missing this statement is a common cause of claim denials.
❌ Omitting Patient Consent or Identity Verification
Providers must document verbal consent for telehealth and confirm patient identity at the start of every audio-only visit.
❌ Using CPT 98015 for New Patients
CPT 98015 applies only to established patients. New-patient audio-only E/M visits should be billed under CPT 98008–98011, depending on MDM complexity and time.
❌ Counting Non-Billable Time
Administrative work, scheduling, or tasks not directly related to the encounter cannot be counted toward billable time. Only provider-performed, medically necessary activities on the same date are eligible.
❌ Reporting 98015 With Same-Day E/M Codes
Audio-only codes (98008–98015) may not be billed alongside in-person or audio-video E/M services for the same patient on the same date.
❌ Incomplete Clinical Narrative
Even though the visit is conducted via audio-only communication, documentation must include a complete clinical summary — history, assessment, plan, and follow-up. Missing this level of detail can result in payer audits or denials.


