CPT 98009 Description, Billing Rules, & Use Cases
CPT 98009 is used to bill for a synchronous audio-only evaluation and management (E/M) visit with a new patient, requiring a medically appropriate history and/or examination and low level medical decision making (MDM).
This code is part of the 2025 audio-only telemedicine E/M series (98008 – 98011), which replaced the deleted telephone E/M codes (99441 – 99443). CPT 98009 represents a longer new-patient audio-only encounter than 98008 and requires at least 30 minutes of total provider time on the date of service.
The visit typically includes:
- Gathering a detailed history and performing a focused audio-based assessment of the patient’s condition
- Managing one or more low-complexity problems or self-limited illnesses
- Counseling the patient on treatment options and self-care
- Reviewing or ordering tests as appropriate to the case
- Coordinating follow-up care and documenting the interaction in the EHR
Billing Notes:
- Applies only to audio-only encounters conducted in real time (no video).
- Must involve ≥30 minutes of provider time if time is the basis for code selection.
- Requires low MDM — more involved than 99408 but below moderate (99203/98010) thresholds.
- Cannot be reported the same day as a video or in-person E/M service.
- Patient consent, identity verification, and communication method must be documented.
What is CPT Code 98009?
CPT 98009 is an evaluation and management (E/M) code used to report audio-only telemedicine visits with new patients that involve low-complexity medical decision making (MDM) or at least 30 minutes of total provider time on the date of the encounter.
This code, introduced in 2025, is part of the new audio-only E/M range (98008–98011) for new patient encounters. It replaces the deleted telephone codes (99441–99443) and supports the growing role of telemedicine for patients who lack access to video technology.
Key points about CPT 98009:
- Used for new patient audio-only visits requiring more in-depth evaluation than CPT 98008.
- The provider must spend a minimum of 30 minutes in real-time audio communication.
- The encounter must include a medically appropriate history and/or exam, and low-level MDM.
- Synchronous communication is required — asynchronous messaging or store-and-forward exchanges do not qualify.
- The call must include meaningful medical discussion and result in an assessment or plan.
- May not be billed on the same day as an in-person or audio-video E/M visit.
In summary: CPT 98009 captures extended, low-complexity audio-only visits with new patients — bridging the gap between brief triage encounters (98008) and longer or more complex evaluations (98010–98011).
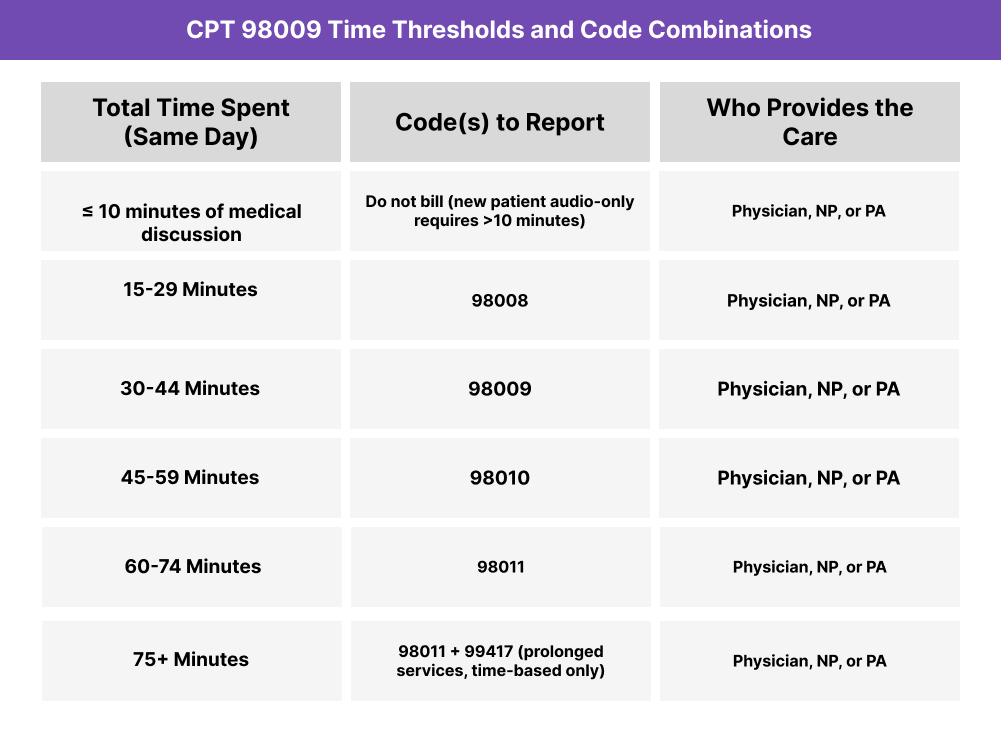
CPT 98009 Time Thresholds and Code Combinations
CPT 98009 represents a synchronous audio-only evaluation and management (E/M) service for a new patient requiring low medical decision making (MDM) and at least 30 minutes of total provider time on the date of service.
Understanding the Time Component
When coding by time, the provider must spend a minimum of 30 minutes in direct medical discussion with the patient. Time includes only provider-performed activities, such as:
- Reviewing relevant history and documentation before or during the call
- Conducting the patient interview via audio-only connection
- Making clinical decisions and formulating a care plan
- Counseling the patient or caregiver about next steps
- Documenting the encounter in the EHR on the same date
If total time exceeds 44 minutes, the next-level code (CPT 98010) should be reported. If the visit lasts less than 30 minutes, CPT 98008 should be used instead.
Understanding the MDM Component
When selecting by MDM rather than time, low-complexity decision making must be documented. This typically includes:
- One or more stable or self-limited conditions
- Limited data reviewed or ordered
- Low risk of morbidity, mortality, or treatment complications
When to Use CPT 98009: Common Scenarios and Use Cases
CPT 98009 is appropriate when a physician, nurse practitioner (NP), or physician assistant (PA) provides a synchronous audio-only evaluation and management (E/M) visit with a new patient that requires low-complexity medical decision making (MDM) or at least 30 minutes of total provider time.
Here are examples of how CPT 98009 is used in practice:
CPT 98009 Billing Requirements and Eligibility
CPT 98009 is used to report synchronous audio-only evaluation and management (E/M) visits for new patients that involve low medical decision making (MDM) or at least 30 minutes of total provider time. This code applies when the encounter includes real-time, interactive verbal communication but no video component.
To bill CPT 98009 compliantly, documentation must demonstrate:
Patient Eligibility Requirements
The patient encounter must meet the following criteria:
- The visit was audio-only and conducted in real time (not asynchronous or message-based).
- The patient consented to the telehealth format and understood it was an audio-only service.
- The service addressed a new patient’s health concern that required clinical assessment, treatment planning, or medication management.
- The encounter involved low-complexity medical decision making or at least 30 minutes of total time spent by the provider.
- The service was not performed on the same day as another E/M service.
Documentation Requirements
Your record should clearly include:
- Total time spent on the date of the encounter (minimum 30 minutes).
- Detailed notes describing the interaction, assessment, and any actions taken.
- Nature of communication — explicitly state that it was audio-only synchronous communication.
- Any care coordination or follow-up actions initiated during the call.
- Patient consent for telemedicine, including acknowledgment of the audio-only format.
Provider Requirements
CPT 98009 may be billed by:
- Physicians (e.g., family medicine, internal medicine, psychiatry)
- Nurse practitioners (NPs)
- Physician assistants (PAs)
- Other qualified healthcare professionals (QHPs) authorized to bill E/M services
Providers must personally perform the encounter and document the total time or MDM level used for code selection.
Telemedicine and Time Rules
- The minimum required time for CPT 98009 is more than 10 minutes, but at least 30 minutes must be documented for code selection.
- Total time includes reviewing records, conducting the call, documenting the encounter, and arranging follow-up.
- Overlapping time with other E/M or care management codes (e.g., CCM, PCM, BHI) may not be counted toward the same service.
- Services under 10 minutes should not be reported; those under 15 minutes may be billed with CPT 98008 instead.
CPT 98009 Billing Documentation Checklist
To ensure compliant billing for CPT 98009, documentation must confirm the audio-only format, new patient status, and that the encounter involved low-complexity MDM or at least 30 minutes of total provider time.
Your encounter record should include:
- Patient consent for telemedicine and confirmation that the encounter was audio-only, not video-enabled.
- Patient identity verification (name, date of birth, or other identifiers).
- Reason for the visit (chief complaint or presenting problem).
- Provider credentials and role (physician, NP, or PA) and confirmation that the provider personally conducted the service.
- Total duration of the encounter, including:
- Start and end times, or
- Total provider time documented as ≥30 minutes on the date of service.
- MDM documentation, if applicable:
- Problems addressed (low complexity, typically stable or self-limited).
- Data reviewed or ordered (minimal to limited).
- Risk level (low, minimal risk of complications or treatment changes).
- Summary of the medical discussion, including:
- Clinical findings or relevant history obtained by phone
- Assessment and care plan or follow-up instructions
- Any medications prescribed, tests ordered, or referrals made
- Follow-up plan (in-person, virtual, or with another provider).
- Provider attestation confirming the accuracy of the documentation and that services were personally performed.
- Statement of modality noting “synchronous audio-only encounter” to distinguish from audiovisual telehealth.
- Non-duplication statement confirming no overlapping or same-day in-person E/M service was provided.
Common CPT 98009 Billing Mistakes (and How to Avoid Them)
❌ Billing Without 30 Minutes of Documented Time
When coding by time, providers must document at least 30 minutes of total time spent on the date of the encounter. Calls shorter than this threshold should be billed as CPT 98008 or not at all if under 10 minutes.
❌ Failing to Note the Audio-Only Format
Documentation must explicitly state that the encounter was audio-only (no video). Payers frequently deny claims that lack this clarification or assume a video visit was attempted.
❌ Using CPT 98009 for Established Patients
CPT 98009 applies only to new patients. Use 98013–98015 for established patient audio-only encounters.
❌ Under-Documenting MDM Complexity
If coding by medical decision making (MDM) rather than time, the record must clearly show low-complexity decision making, such as limited data reviewed, one or more stable problems, and low risk of complications.
❌ Counting Non-Billable Time
Setup, scheduling, connection time, and administrative work before or after the call do not count toward total provider time. Only medically necessary, provider-performed activities on the date of service qualify.
❌ Omitting Patient Consent or Identity Verification
Patient consent for telehealth — and identity confirmation — must be recorded at each encounter, especially for first-time patients.
❌ Reporting With Other Same-Day E/M Codes
CPT 98009 cannot be reported in combination with in-person or audio-video E/M services on the same calendar day.


