CPT 99213 Description, Billing Rules, & Use Cases
CPT 99213 is used to bill for an office or other outpatient visit with an established patient that requires low level medical decision making (MDM) and/or at least 20 minutes of total provider time spent on the date of the encounter.
This code applies when a physician, nurse practitioner (NP), or physician assistant (PA) evaluates and manages a patient with a low-complexity condition that demands more provider involvement than CPT 99212, but does not rise to the moderate complexity of CPT 99214.
The visit may include:
- Reviewing and updating a detailed history of the patient’s condition
- Performing a focused but more in-depth exam than 99212
- Managing one or more low-complexity problems
- Counseling the patient or caregiver on treatment or lifestyle adjustments
- Ordering or reviewing laboratory or diagnostic tests
- Documenting the encounter and updating the care plan
What is CPT Code 99213?
CPT 99213 is an evaluation and management (E/M) code for established patient office or outpatient visits that require low-complexity medical decision making (MDM) or at least 20 minutes of total provider time on the date of the encounter.
Key points about CPT 99213:
- It is used when the patient presents with one or more stable chronic conditions or an acute problem of low severity.
- The provider must personally deliver the service — unlike CPT 99211, which may be staff-only, and CPT 99212, which is briefer.
- The 2024 guideline update specifies “20 minutes must be met or exceeded” for time-based reporting.
- Total time includes both face-to-face and non–face-to-face activities performed on the date of service (chart review, documentation, counseling, ordering/interpreting tests, etc.).
- If the encounter involves more time or higher complexity, CPT 99214 or higher may be appropriate.
In summary: CPT 99213 is the most commonly used established patient E/M code, covering routine visits for stable chronic conditions or low-complexity acute problems that require direct provider involvement.
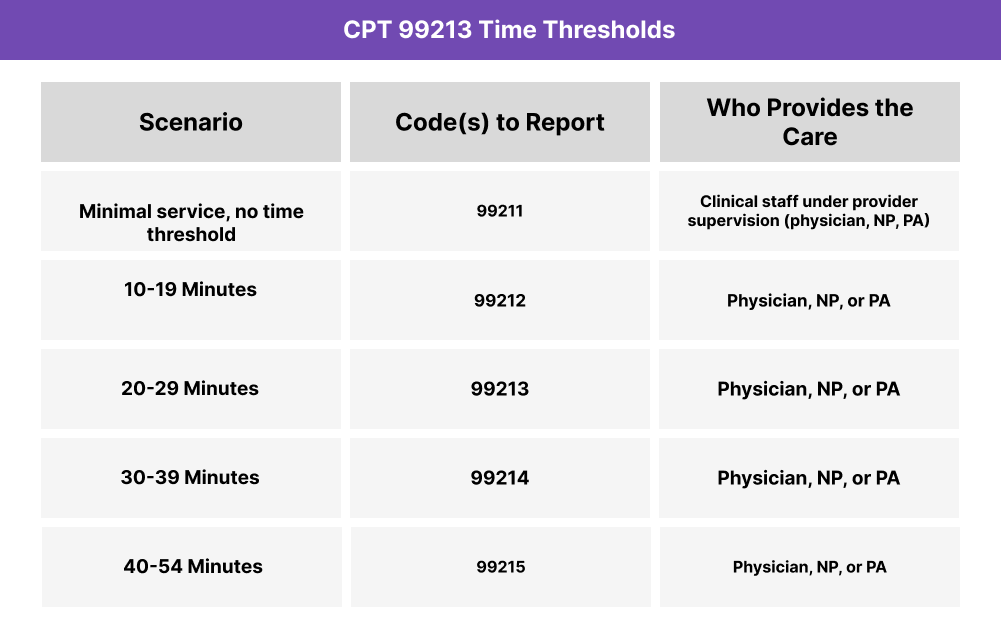
CPT 99213 Time Thresholds and Code Combinations
CPT 99213 applies when an established patient office or outpatient visit requires at least 20 minutes of provider time or low-complexity medical decision making (MDM).
Important to Note:
- 2024 guidelines specify: 20 minutes must be met or exceeded.
- If less than 20 minutes or only straightforward MDM is involved, bill 99212 instead.
- If the encounter requires moderate or high complexity, consider 99214 or 99215.
When to Use CPT 99213: Common Scenarios and Use Cases
CPT 99213 is appropriate when a physician, nurse practitioner (NP), or physician assistant (PA) provides a visit with an established patient that requires at least 20 minutes of provider time or low-complexity MDM.
Here are examples of how CPT 99213 is used in practice:
CPT 99213 Billing Requirements and Eligibility
To bill CPT 99213, the following conditions must be met:
Patient Eligibility
- The patient must be an established patient (seen by the practice within the last three years).
- The presenting problem is typically a stable chronic illness or low-severity acute issue.
Provider Eligibility
- The service must be personally performed by a physician, nurse practitioner (NP), or physician assistant (PA).
- Staff-only visits (without provider involvement) should be billed under 99211, not 99213.
Service Requirements
- Time-based option: At least 20 minutes of total provider time must be documented.
- MDM-based option: Visit must reflect low-complexity medical decision making, including:
- 1–2 self-limited or stable chronic problems
- Limited data to review (labs, imaging, notes)
- Low risk of complications or morbidity
- Total time may include pre-visit chart review, patient counseling, ordering/reviewing tests, documentation, and care coordination.
- If provider time is less than 20 minutes or MDM is only straightforward, bill 99212 instead.
- If more time or moderate complexity is involved, bill 99214.
Code Comparison
- 99212 vs 99213: 99212 is for 10–19 minutes or straightforward MDM. 99213 is for 20–29 minutes or low-complexity MDM.
- 99213 vs 99214: 99213 covers stable conditions or low-severity problems. 99214 applies when 30+ minutes or moderate complexity MDM is required.
CPT 99213 Billing Documentation Checklist
To support compliant billing for CPT 99213, documentation should include:
- Established patient status confirmed (seen by the practice within the past three years).
- Reason for the encounter (e.g., stable chronic condition management, minor acute problem).
- Provider involvement clearly noted (physician, NP, or PA personally performed the service).
- Time documentation (if coding by time):
- At least 20 minutes of total provider time
- Activities included (chart review, exam, counseling, ordering tests, documentation)
- Medical decision making (if coding by MDM):
- Low-complexity MDM
- Problem type: 1–2 stable chronic or low-severity acute issues
- Data: limited review of tests/records
- Risk: low risk of complications, morbidity, or mortality
- Exam and history details supporting the care provided.
- Counseling or education documented if applicable.
- Provider attestation confirming accuracy and personal performance of the encounter.
- Non-duplication statement if other services are billed on the same date.
Common CPT 99213 Billing Mistakes (and How to Avoid Them)
❌ Billing Without 20 Minutes of Documented Time
If coding by time, at least 20 minutes must be recorded. Encounters under this threshold should be billed as 99212.
❌ Using 99213 for Staff-Only Visits
This code requires direct provider involvement. Staff-supervised visits without provider evaluation fall under 99211.
❌ Under-Documenting Low-Complexity MDM
If coded by MDM, the note must reflect low-complexity criteria (1–2 problems, limited data, low risk). Missing detail risks downcoding.
❌ Confusing 99213 With 99214
99213 is for 20–29 minutes or low-complexity MDM. 99214 applies to 30+ minutes or moderate-complexity encounters.
❌ Billing Administrative Work as 99213
Tasks like prescription refills or form completion without an evaluation do not meet requirements for 99213.
❌ Incorrect Service Setting
99213 is only for office or outpatient visits. Hospital, observation, or ED services must use the appropriate E/M codes.



