CPT 99202 Description, Billing Rules, & Use Cases
CPT 99202 is used to bill for an office or other outpatient visit with a new patient that requires straightforward medical decision making and/or at least 15 minutes of total time spent on the date of the encounter
This code applies when a physician or qualified healthcare professional evaluates and manages a patient in an office or outpatient setting, typically involving low-complexity conditions or concerns.
The visit may include:
- Taking a patient history and performing a medically appropriate exam
- Counseling or educating the patient or caregiver
- Reviewing and ordering tests
- Documenting the encounter
- Coordinating care with other healthcare professionals
What is CPT Code 99202?
CPT 99202 is an Evaluation and Management (E/M) billing code used for new patient office or outpatient visits that require straightforward medical decision making or at least 15 minutes of total time spent on the date of the encounter
This code applies when the provider:
- Reviews the patient’s medical history and performs a medically appropriate exam
- Addresses problems of low complexity
- Spends a minimum of 15 minutes on the visit, including both face-to-face and non–face-to-face activities (such as reviewing records, ordering tests, or documenting)
Examples of services covered under CPT 99202 include:
- Evaluating new symptoms or minor conditions
- Counseling or educating the patient or caregiver
- Ordering and reviewing laboratory or diagnostic tests
- Coordinating care with other healthcare professionals
- Documenting the encounter and follow-up plan
Unlike higher-level codes (99203–99205), CPT 99202 is intended for simpler cases with limited complexity and relatively short visit times.
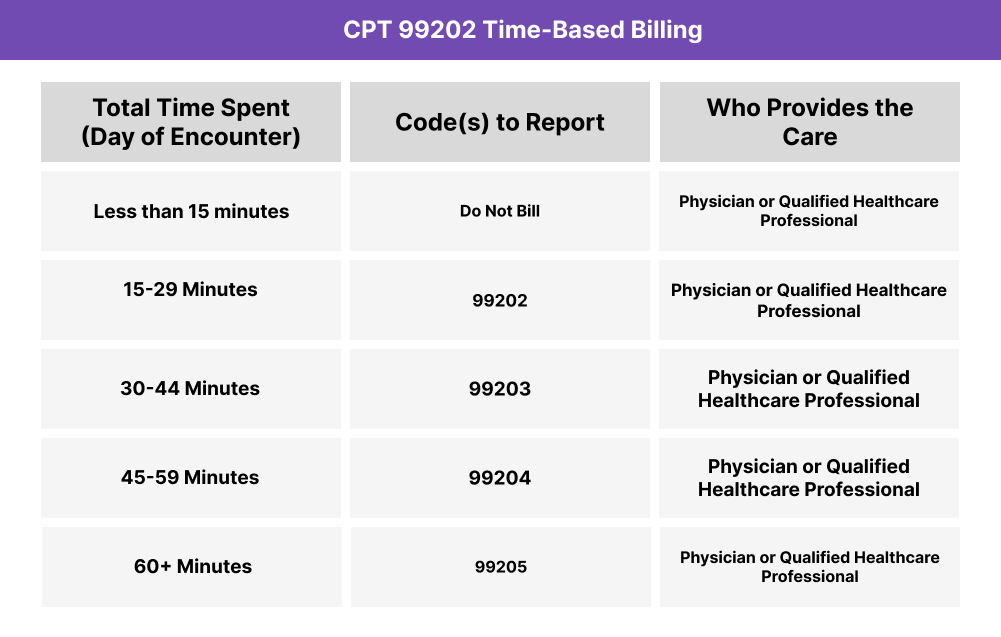
CPT 99202 Time Thresholds and Code Combinations
CPT 99202 is used to report a new patient office or other outpatient visit when the provider spends at least 15 minutes of total time on the date of the encounter, or when the level of medical decision making is straightforward
Important to Note:
- The 2024 revision specifies that “15 minutes must be met or exceeded” (replacing the old 15–29 minute range).
- Total time includes both face-to-face and non–face-to-face activities, such as reviewing patient records, documenting the visit, ordering tests, and communicating results.
- Do not bill CPT 99202 if less than 15 minutes is spent or if medical decision making does not reach the threshold for this code.
- For more complex visits, report CPT 99203–99205 instead, based on time or medical decision making.
When to Use CPT 99202: Common Scenarios and Use Cases
CPT 99202 is appropriate when a physician or qualified healthcare professional sees a new patient in the office or outpatient setting, spends at least 15 minutes on the encounter, and the visit involves straightforward medical decision making.
Here are examples of how CPT 99202 is used in practice:
CPT 99202 Billing Requirements and Eligibility
CPT 99202 is used to report office or other outpatient visits with a new patient when the provider spends at least 15 minutes on the encounter or the visit involves straightforward medical decision making.
These services must meet documentation and eligibility standards for time, medical necessity, and provider qualifications.
Patient Eligibility Criteria
The patient must:
- Be a new patient (not seen by the same provider group in the past three years)
- Present with problems of low complexity that require straightforward medical decision making
- Receive care in an office or other outpatient setting (not inpatient, observation, or emergency department)
Provider Requirements
The billing provider must be a:
- Physician (MD or DO)
- Nurse Practitioner (NP)
- Physician Assistant (PA)
The provider must:
- Personally perform the visit
- Determine the medical decision making or total time spent
- Document all services rendered during the encounter
Service Requirements
The encounter must include either:
- At least 15 minutes of total time on the date of service (including both face-to-face and non–face-to-face activities such as history review, ordering tests, documenting, and communicating results)
OR - Straightforward medical decision making as defined by CPT guidelines
Additional requirements:
- Time and activities must be distinct from other billed services
- All elements performed (history, exam if done, counseling, documentation, coordination) must be clearly recorded in the patient’s medical record
CPT 99202 Billing Documentation Checklist
To support compliant billing for CPT 99202, your records should include the following:
- A clear record of at least 15 minutes spent on the date of service, or documentation that straightforward medical decision making was performed
- Detailed time logs (if coding by time) that specify:
- Date of encounter
- Activities performed (e.g., reviewing history, ordering tests, counseling, documenting)
- Total duration of provider time
- Patient status as a new patient, confirming no face-to-face professional service by the same provider group within the past three years
- Medical decision making documentation that demonstrates:
- The number and complexity of problems addressed were low
- The amount/complexity of data reviewed was minimal
- The risk of morbidity or complications was minimal
- Elements of the encounter performed, such as:
- Medically appropriate history and/or examination
- Counseling or education of the patient or caregiver
- Ordering or reviewing laboratory or diagnostic tests
- Care coordination or referrals as appropriate
- Provider attestation confirming that the services were personally performed by a physician, nurse practitioner, or physician assistant and that all documentation is accurate and complete
- A note that reported time was distinct from any other billed services, such as preventive visits or other E/M encounters on the same date
Common CPT 99202 Billing Mistakes (and How to Avoid Them)
❌ Billing Without 15 Minutes of Documented Time
CPT 99202 requires at least 15 minutes of qualifying provider time on the date of service. Anything less is not billable, even if the service was medically appropriate.
❌ Using 99202 for Established Patients
This code may only be used for new patients. Established patient visits must be billed with CPT 99211–99215.
❌ Under-Documenting Medical Decision Making
When billing by MDM instead of time, the documentation must clearly support straightforward medical decision making (low complexity problems, minimal risk, limited data). Missing this detail may trigger denials.
❌ Overlapping With Preventive Services
Do not bill 99202 in place of or in addition to a preventive service (e.g., annual wellness exam) unless distinct and separately identifiable services are documented.
❌ Counting Non-Provider Time
Only time personally spent by a physician, nurse practitioner, QHP, or physician assistant counts toward the 15-minute requirement. Medical assistant or nursing staff time cannot be included.
❌ Incorrect Setting of Service
CPT 99202 is for office or outpatient visits only. Do not use it for inpatient admissions, observation services, or emergency department visits — those have separate E/M codes.



