CPT 98016 Description, Billing Rules, & Use Cases
CPT 98016 is used to bill for a brief, patient-initiated audio-only communication between a physician, nurse practitioner (NP), or physician assistant (PA) and an established patient that lasts 5–10 minutes.
Introduced in 2025, CPT 98016 replaced HCPCS code G2012 as part of the broader expansion of the audio-only telehealth code set (98008–98016). It covers short, real-time verbal interactions that do not require the complexity, duration, or documentation of a full evaluation and management (E/M) visit.
The service typically includes:
- Follow-up on a recent issue that does not require an in-person or telehealth E/M visit
- Medication management or response check after a recent adjustment
- Guidance or triage related to a minor concern that can be resolved verbally
- Clarification of test results or care instructions previously discussed
- Determination of whether a full E/M service is necessary
Billing Notes:
- Use CPT 98016 for audio-only communications lasting 5–10 minutes, initiated by the patient or caregiver.
- The patient must be established, and the conversation must be direct, real-time, and verbal (not text or asynchronous messaging).
- The call cannot originate from a related E/M visit within the prior 7 days and cannot result in an in-person or telehealth visit within 24 hours or the next available appointment.
- Documentation must include patient consent, audio-only modality, and total time spent.
- This service may not be billed concurrently with audio-only E/M codes (98008–98015).
What Is CPT Code 98016?
CPT 98016 is a communication technology-based service (CTBS) code for brief audio-only interactions with established patients that last 5–10 minutes and are initiated by the patient or caregiver.
Introduced in 2025, CPT 98016 replaced the now-deleted HCPCS code G2012 as the official CPT descriptor for brief, real-time telecommunication between a qualified healthcare provider and an established patient. Unlike the audio-only E/M codes (98008–98015), this service does not require MDM documentation and is time-based only.
Key points about CPT 98016:
- Used for audio-only, real-time communications lasting 5–10 minutes.
- Applies only to established patients.
- The call must be patient-initiated (not scheduled or provider outreach).
- The encounter must not be related to an E/M visit within the previous 7 days or lead to one within 24 hours (or the next available appointment).
- May be used for minor concerns, medication questions, or care clarifications.
- Cannot be billed concurrently with 98008–98015 or other E/M services for the same patient on the same day.
In summary: CPT 98016 captures short, patient-initiated audio-only check-ins that allow a provider to determine if further evaluation or treatment is required, replacing HCPCS G2012 as the streamlined 2025 CPT option for brief, non-complex telehealth communication.
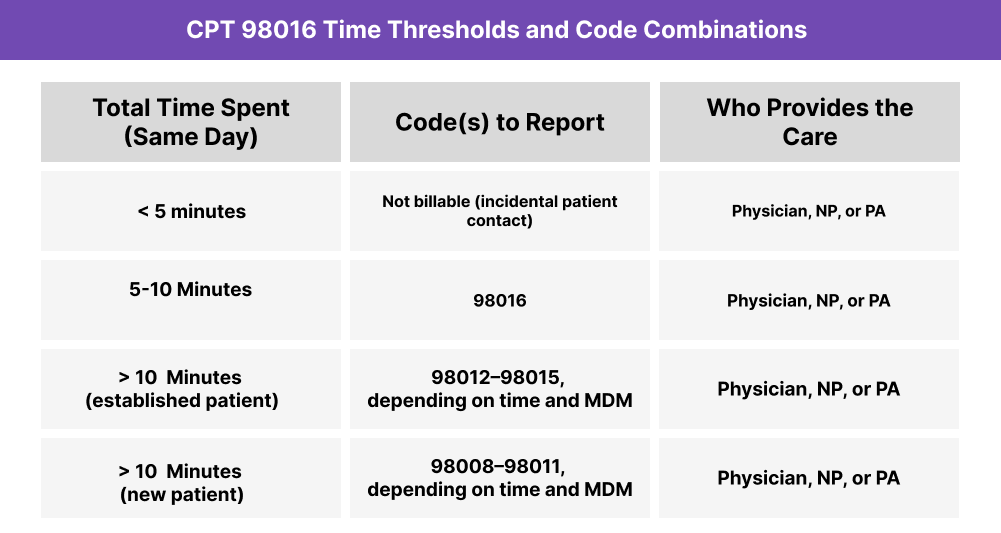
CPT 98016 Time Thresholds and Code Combinations
CPT 98016 represents a brief, patient-initiated audio-only communication between a qualified healthcare provider and an established patient, lasting 5–10 minutes. It is time-based and does not require medical decision making (MDM) documentation.
Understanding the Time Component
When billing by time, the provider must personally spend at least 5 minutes but not more than 10 minutes communicating with the patient in real time.
Included time may involve:
- Direct verbal communication addressing a clinical question or concern
- Reviewing the patient’s medical record as part of the same 5–10 minute call
- Providing brief advice, education, or clarification of prior care instructions
- Determining whether a full E/M service is required
Important to Note:
- Calls lasting under 5 minutes are considered incidental and not billable.
- Calls exceeding 10 minutes should be billed under the appropriate audio-only E/M code (98012–98015) based on time and MDM complexity.
- CPT 98016 cannot be billed within 7 days after a related E/M visit or if the call results in an in-person or telehealth E/M encounter within 24 hours (or the next available appointment).
When to Use CPT 98016: Common Scenarios and Use Cases
CPT 98016 is appropriate when a physician, nurse practitioner (NP), or physician assistant (PA) provides a brief, patient-initiated, audio-only communication with an established patient that lasts 5–10 minutes and does not require a full E/M visit.
Here are examples of how CPT 98016 is used in practice:
CPT 98016 Billing Requirements and Eligibility
CPT 98016 is used to report a brief, patient-initiated audio-only communication between a physician, nurse practitioner (NP), or physician assistant (PA) and an established patient that lasts 5–10 minutes.
This code was introduced in 2025 as part of the expanded audio-only telehealth family (98008–98016) and directly replaces HCPCS code G2012. Unlike audio-only E/M codes, CPT 98016 is a communication technology-based service (CTBS)—not a full E/M encounter—and is used for short, real-time check-ins rather than comprehensive evaluations.
Patient Eligibility
To qualify for CPT 98016:
- The patient must be established (seen by the same provider or group within the past three years).
- The communication must be initiated by the patient or caregiver.
- The service must be conducted using real-time, two-way audio-only communication.
- The encounter must last 5–10 minutes in total duration.
- The call must not relate to an E/M visit performed by the same provider within the previous 7 days.
- The call must not lead to an in-person or telehealth E/M visit within 24 hours or the next available appointment.
Note: There is no equivalent code for new patients. CPT 98016 applies only to established patients. New-patient audio-only communications must be billed as full E/M services (98008–98011) or treated as non-billable triage contact.
Provider Eligibility
The encounter must be personally performed by a physician, NP, or PA who is authorized to bill E/M services.
The provider must:
- Personally perform and document the entire audio-only interaction.
- Clearly record total time spent (5–10 minutes).
- Document the modality (audio-only) and patient consent for telehealth communication.
- Provide a brief clinical summary that reflects professional input or guidance offered during the call.
Service Requirements
- Duration: Must last at least 5 minutes but no more than 10 minutes.
- Countable time includes direct patient communication, record review during the call, and immediate documentation.
- Non-countable time includes administrative tasks, scheduling, or follow-up unrelated to the encounter.
- The service may not overlap with another E/M or telehealth code for the same patient on the same date.
- Patient consent and mode of communication must be explicitly documented.
Documentation Requirements
The visit note must clearly include:
- Patient consent for the audio-only telehealth encounter.
- Verification of patient identity (e.g., name and date of birth).
- Provider credentials and role (physician, NP, or PA).
- Modality statement confirming “audio-only synchronous communication.”
- Chief concern or reason for contact.
- Total time spent (5–10 minutes).
- Summary of clinical discussion, including guidance or recommendations.
- Provider attestation verifying personal performance and accuracy.
- Statements confirming:
- No related E/M service occurred within the previous 7 days.
- The call did not lead to a same-day or next-available E/M visit.
Medicare and Payer Coverage Notes
- Medicare: CPT 98016 currently carries a status indicator “I” (invalid for Medicare billing) pending policy adoption.
- Commercial payers: Many are expected to recognize CPT 98016 as the successor to G2012 for brief, audio-only communications.
- Action: Providers should verify payer-specific policies for 2025, as coverage for short-duration audio-only services may vary by insurer and state.
CPT 98016 Billing Documentation Checklist
To support compliant billing for CPT 98016, documentation must verify that the service was a real-time, audio-only communication with an established patient, initiated by the patient or caregiver, lasting 5–10 minutes, and unrelated to a recent or upcoming E/M encounter.
Your encounter record should include:
- Patient consent for the audio-only telehealth communication, documented before or at the start of the call.
- Verification of patient identity using at least two identifiers (e.g., name and date of birth).
- Provider credentials and role (physician, NP, or PA) clearly stated.
- Statement of modality confirming “audio-only synchronous communication” (no video used).
- Chief concern or reason for the call, such as a symptom update, medication clarification, or test result review.
- Total provider time documented as 5–10 minutes, including:
- Exact start and end times, or
- Total duration of communication on the date of service.
- Summary of the discussion, including:
- Key points discussed with the patient or caregiver.
- Advice, recommendations, or next steps provided.
- Whether follow-up was deemed necessary or not.
- Provider attestation confirming personal performance and accuracy of the documentation.
- Statements confirming:
- The call was initiated by the patient or caregiver.
- No related E/M visit occurred within the previous 7 days.
- The call did not result in a same-day or next-available E/M appointment.
- Follow-up plan documented, if applicable (e.g., “patient to call back if symptoms persist or worsen”).
Common CPT 98016 Billing Mistakes (and How to Avoid Them)
❌ Billing Without 5 Minutes of Documented Time
Providers must record at least 5 minutes of total provider time. Calls under this threshold are considered incidental and non-billable.
❌ Using CPT 98016 for Calls Over 10 Minutes
This code applies only to brief communications (5–10 minutes). Encounters exceeding 10 minutes should be billed using the appropriate audio-only E/M code (98012–98015) based on time and MDM complexity.
❌ Applying 98016 to New Patients
CPT 98016 is for established patients only. New-patient communications must be billed under CPT 98008–98011 or treated as administrative triage, not a billable service.
❌ Omitting Patient-Initiated Requirement
This service must be initiated by the patient or caregiver. Provider-initiated calls, follow-ups, or outreach do not qualify.
❌ Missing Audio-Only Modality Statement
Each note must specify that the communication occurred via audio-only synchronous technology (not video, text, or asynchronous messaging).
❌ Billing When Related to a Recent or Upcoming E/M Visit
CPT 98016 cannot be billed if the call is:
- Related to an E/M visit that occurred within the prior 7 days, or
- Leads to an E/M service within 24 hours or the next available appointment.
❌ Counting Administrative or Non-Clinical Time
Scheduling, charting, or other administrative activities are not billable toward the 5–10 minute total. Only direct, medically necessary communication counts.
❌ Incomplete Documentation of Consent or Time
Failure to document verbal patient consent or total duration of communication is a frequent reason for payer denial.


