What Is an IDT (Interdisciplinary Team) in Healthcare?
An Interdisciplinary Team (IDT) is a coordinated group of healthcare professionals from different clinical and support disciplines who work together to plan, deliver, and evaluate patient care. IDTs are used across Medicare-funded settings to manage complex patients who require coordinated medical, functional, and social support. In Medicare and post-acute care environments, IDTs are not just a care model — they are often a regulatory and documentation expectation. Settings such as Inpatient Rehabilitation Facilities (IRFs), Home Health Agencies (HHAs), and value-based Medicare programs rely on IDTs to demonstrate coordinated care planning, ongoing assessment, and appropriate transitions of care. Operationally, IDTs function as the bridge between clinical delivery and compliance. How well an IDT is structured, documented, and executed directly affects quality outcomes, audit defensibility, and reimbursement integrity.
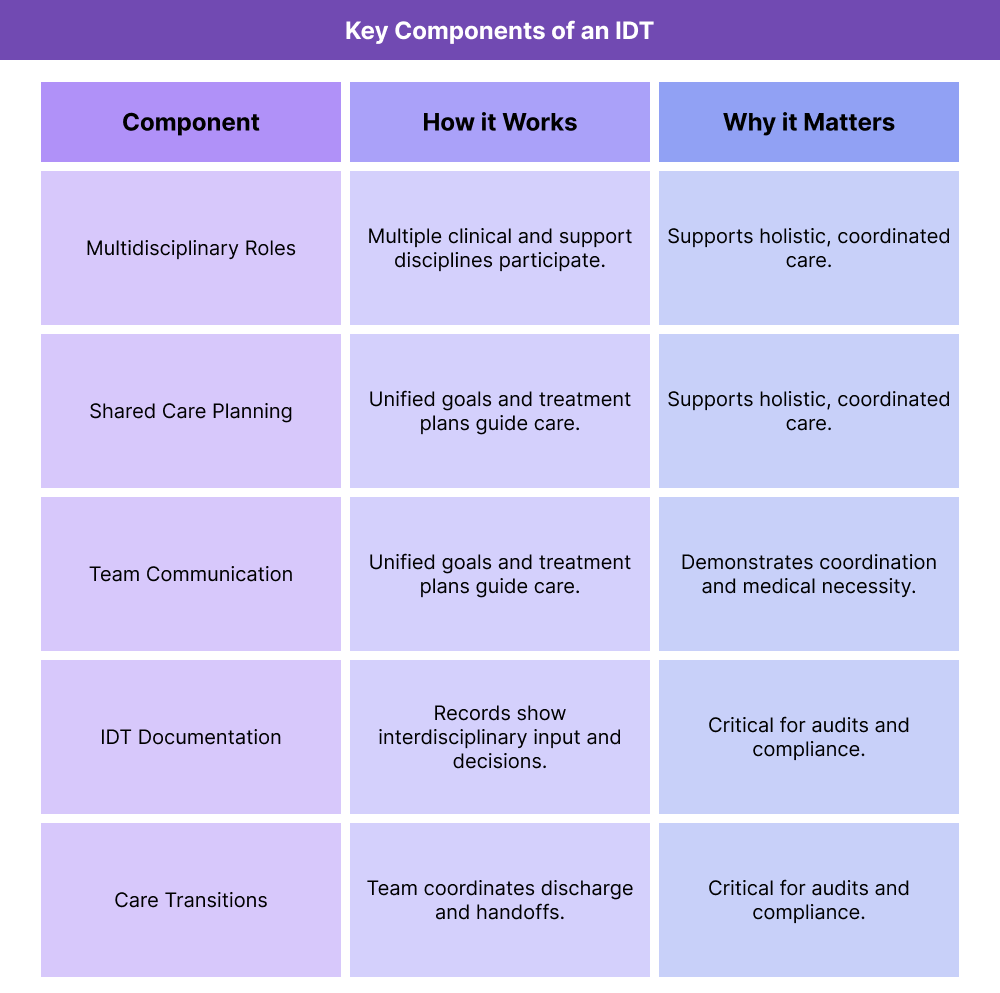
Key Components of the Interdisciplinary Teams (IDTs)
While the exact composition of an IDT varies by care setting, effective IDTs share common structural and operational components that support coordination, accountability, and compliance. Core Clinical and Support Roles Within an IDT An IDT typically includes professionals from multiple disciplines, such as physicians, nurses, therapists, social workers, care managers, and other support roles. Each member contributes specialized expertise while participating in shared care planning. The key operational requirement is not just who is on the team, but how responsibilities are defined and coordinated. Shared Care Planning and Goal Setting IDTs are responsible for developing and maintaining a unified plan of care. This includes identifying patient goals, assigning responsibilities across disciplines, and adjusting the plan as patient needs change. From a Medicare compliance standpoint, shared care planning helps demonstrate that services are coordinated rather than duplicative. Ongoing Communication and Team Coordination Effective IDTs rely on structured communication, such as regular team meetings, case conferences, or documented care reviews. These interactions ensure alignment across disciplines and reduce fragmentation. Poor communication is a common failure point that leads to inconsistent documentation and audit findings. Documentation of IDT Participation and Decisions Documentation is critical. Medicare reviewers often look for evidence that interdisciplinary input informed care decisions, not just parallel services delivered by different providers. IDT documentation should reflect: Participation from multiple disciplines Clinical rationale for care decisions Updates based on patient progress or changes IDTs and Care Transitions IDTs play a central role in managing transitions between care settings, such as discharge from IRF to home health or coordination with outpatient providers. Clear handoffs reduce readmissions and improve continuity of care.
How Interdisciplinary Teams (IDTs) Work in Practice In practice, IDTs operate as the coordination engine behind complex care delivery. Rather than care occurring in silos, IDTs formalize how different disciplines contribute to a single plan of care, document shared decision-making, and adjust treatment as patient needs evolve. In Medicare-regulated settings, IDT workflows are especially important because reviewers often assess how care was coordinated—not just whether individual services were delivered. Step 1: Patient Assessment Across Disciplines IDT workflows begin with assessment. Each discipline evaluates the patient from its own perspective—medical, functional, behavioral, and social. Operationally, this means: Nursing assesses clinical stability and skilled needs Therapists assess functional limitations and rehabilitation potential Social work evaluates psychosocial barriers and support systems Physicians or practitioners provide medical oversight and direction These assessments form the foundation for shared care planning. Step 2: Development of a Unified Plan of Care After assessments are completed, the IDT collaborates to develop a unified plan of care. This plan outlines: Patient-centered goals Discipline-specific interventions Expected timelines and outcomes Criteria for reassessment or discharge In Medicare settings such as IRFs and HHAs, this step is critical for demonstrating coordinated, medically necessary care rather than disconnected services. Step 3: Ongoing IDT Communication and Case Review IDTs do not operate as a one-time meeting. Teams regularly communicate through scheduled case conferences, documented reviews, or structured check-ins. In practice, this includes: Reviewing patient progress and barriers Adjusting care plans based on response to treatment Escalating concerns such as deterioration or safety risks Aligning services to avoid duplication Regular communication reduces inconsistencies that often surface during audits. Step 4: Documentation of IDT Decisions and Participation Documentation is where IDT work becomes defensible. Medicare reviewers look for evidence that interdisciplinary input informed care decisions. Effective IDT documentation reflects: Participation from multiple disciplines Clinical rationale for changes in care Clear linkage between assessments, decisions, and services delivered Poor documentation can make coordinated care appear fragmented, even when collaboration occurred. Step 5: Discharge Planning and Care Transitions IDTs play a central role in discharge planning and transitions of care. The team evaluates readiness for discharge, coordinates follow-up services, and communicates plans to downstream providers. Strong IDT-led transitions reduce readmissions and support continuity, especially when patients move between IRFs, HHAs, outpatient care, or primary care.
IDTs in Billing, Reimbursement, and System Limitations
While IDTs are primarily a care delivery model, they directly affect reimbursement, audit outcomes, and operational risk. How IDTs Support Medicare Billing and Medical Necessity IDTs help support billing by demonstrating that services were coordinated and medically necessary. When documentation shows interdisciplinary planning and oversight, it strengthens the clinical narrative behind billed services. This is especially important in post-acute settings where payment is sensitive to documentation quality rather than service volume. IDTs and Audit Defensibility Auditors often look for signs of siloed care. IDT documentation helps counter this by showing that care decisions were informed by multiple disciplines and adjusted based on patient response. Lack of IDT evidence is a common audit finding in settings where interdisciplinary coordination is expected. System Limitations That Undermine IDT Effectiveness IDT effectiveness is often constrained by system limitations, such as: Fragmented EHRs that separate discipline-specific documentation Lack of standardized IDT templates or workflows Scheduling challenges that limit team communication High staff turnover affecting continuity Organizations that invest in structured IDT workflows and shared documentation tools tend to perform better in both quality and compliance reviews.
How IDTs Influence Quality, Access, and Equity in Home Health
IDTs are closely tied to patient outcomes, particularly for complex and high-risk populations. IDTs and Quality of Care By aligning multiple perspectives, IDTs improve care quality through better assessment, goal alignment, and early identification of issues. Coordinated care reduces duplication, errors, and gaps that negatively affect outcomes. IDTs and Access to Services IDTs can improve access by coordinating services efficiently and prioritizing interventions based on patient need. However, poorly resourced teams may struggle to maintain consistent communication, limiting effectiveness. Equity Implications of Interdisciplinary Care IDTs support equity by incorporating social, behavioral, and environmental factors into care planning. Including social work and care coordination roles helps address barriers that disproportionately affect underserved populations. Equity-focused IDTs ensure care plans reflect real-world patient circumstances, not just clinical diagnoses.
Frequently Asked Questions about IDTs
1. What is an IDT (Interdisciplinary Team) in healthcare?
An Interdisciplinary Team (IDT) is a group of healthcare professionals from different disciplines who work together to plan, deliver, and evaluate coordinated patient care.
2. Where are IDTs commonly required in Medicare care?
IDTs are commonly used in Medicare-regulated settings such as IRFs, home health, hospice, and value-based care programs where coordinated care planning is expected.
3. Why is IDT documentation important for Medicare compliance?
Documentation shows that care decisions were informed by multiple disciplines. This supports medical necessity, coordinated care, and audit defensibility.
4. Who typically participates in an IDT?
IDTs often include physicians, nurses, therapists, social workers, care managers, and other relevant support roles, depending on the care setting.
5. How do IDTs improve patient outcomes?
IDTs improve outcomes by aligning goals, reducing fragmented care, identifying issues early, and coordinating transitions between care settings.
6. Can poor IDT documentation affect reimbursement?
Yes. Weak or missing IDT documentation can undermine the clinical narrative behind billed services and increase audit or denial risk.
7. How do IDTs support care transitions?
IDTs coordinate discharge planning, communicate with downstream providers, and ensure continuity of care after transitions.
