What is IHS (Indian Health Service) and What Is an IHS Clinic?
The Indian Health Service (IHS) is a federal health system within the U.S. Department of Health and Human Services that provides medical care to enrolled American Indian and Alaska Native (AI/AN) individuals. IHS delivers care through a network of hospitals, health centers, and clinics operated either directly by IHS or by Tribes and Tribal organizations under self-governance authority.
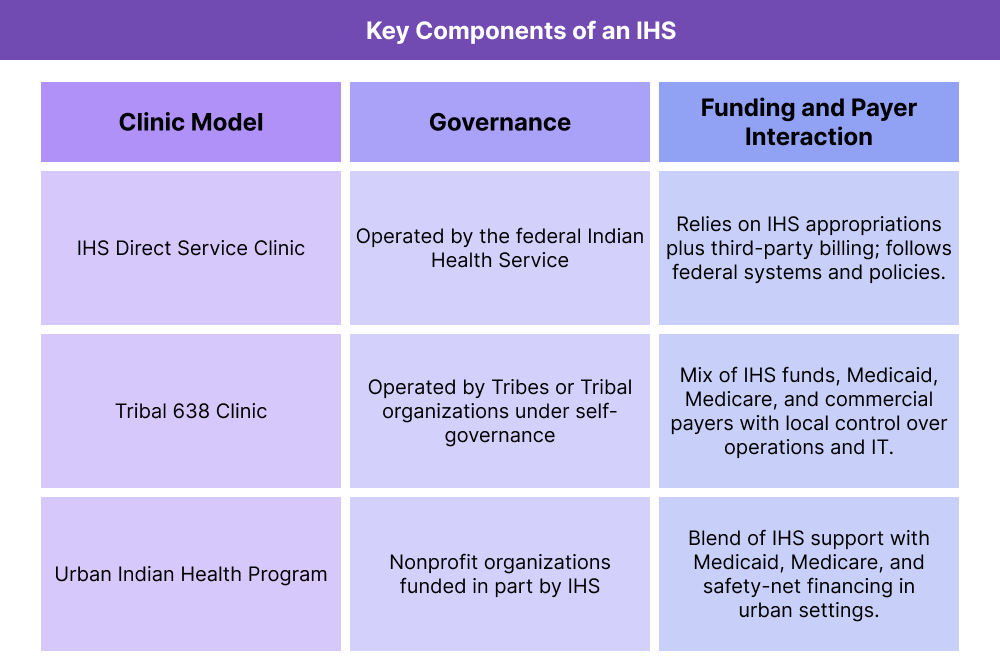
An IHS clinic (often referred to as an IHS facility or Tribal 638 clinic) is a primary care or outpatient clinic that provides culturally informed, community-based healthcare to AI/AN populations. Clinics may be:
- IHS Direct Service Facilities — operated federally by IHS
- Tribal 638 Facilities — operated by Tribes under the Indian Self-Determination and Education Assistance Act (ISDEAA)
- Urban Indian Health Programs (UIHPs) — nonprofit clinics serving AI/AN people in urban settings
All are part of the broader Indian Health system, but each has different degrees of autonomy, billing capabilities, and operational structure.
In practice, IHS and Tribal clinics serve as essential access points in rural, frontier, and reservation-based communities where alternatives may be limited. They provide primary care, behavioral health, preventive services, case management, and community health programs rooted in cultural context and sovereignty.
Key Components of IHS and Tribal Clinics
IHS and Tribal clinics share a common mission—to provide accessible, culturally grounded care for American Indian and Alaska Native (AI/AN) people—but they operate under different governance and reimbursement models. Understanding these models is important for payers, health IT vendors, and partner organizations that interact with IHS facilities on referrals, data exchange, and contracting.
IHS Direct Service Clinics and Health Centers
IHS direct service clinics are federally operated facilities managed by the Indian Health Service. They follow federal civil service structures, use IHS-operated infrastructure, and typically deliver primary care, preventive services, behavioral health, and limited specialty care based on local capacity.
For external partners, direct service IHS clinics function as federal providers with specific rules for credentialing, contracting, and data sharing.
Tribal 638 Clinics and Self-Governance Facilities
Tribal 638 clinics are operated by Tribes or Tribal organizations under the Indian Self-Determination and Education Assistance Act. These clinics assume responsibility for delivering services that might otherwise be provided by IHS, with more local control over staffing, budgeting, and care models.
From a business standpoint, Tribal clinics behave more like independent health systems: they make local decisions about EHR platforms, care management programs, payer contracts, and how to integrate Medicare, Medicaid, and commercial billing alongside IHS funding.
Urban Indian Health Programs (UIHPs)
Urban Indian Health Programs are nonprofit organizations that provide culturally informed care to AI/AN people living in urban areas. They are not always operated by IHS directly but receive IHS funding and may also function as FQHCs or community health centers for billing and regulatory purposes.
These programs blend IHS support with mainstream safety-net financing, including Medicaid, Medicare, and sometimes RHC-like primary care access models.
Funding, Payer Mix, and IHS Reimbursement
IHS and Tribal clinics are funded through a combination of:
- Federal IHS appropriations
- Third-party revenue from Medicaid, Medicare, and commercial payers
- Grants and state or local program funds
Many IHS and Tribal clinics use an encounter-based reimbursement model for certain payers, where a single all-inclusive rate is paid per qualifying visit rather than fee-for-service line items. This has important implications for coding, visit structuring, and care management documentation.
Care Services Commonly Delivered in IHS Clinics
IHS clinics are primarily primary care access points. Typical services include:
- Family medicine and internal medicine
- Pediatric care
- Women’s health and prenatal care
- Behavioral health and substance use disorder support
- Preventive services, immunizations, and health screenings
- Chronic disease management and care coordination
- Community health worker and public health programs
These services are adapted to local community needs, geography, and available workforce.
How IHS Clinics Work in Practice
IHS and Tribal clinics operate at the intersection of federal obligations, Tribal sovereignty, and community-specific health needs. Day to day, they function as primary care and care-coordination hubs that link patients to both local services and external systems such as hospitals, CAHs, RHCs, and specialist networks.
Step 1: IHS Eligibility and Patient Registration
Patients who seek care at IHS or Tribal clinics typically go through an eligibility and registration process that confirms AI/AN status and gathers demographic and coverage information. Eligibility rules may differ between IHS direct service, Tribal 638 sites, and Urban Indian programs, but all rely on accurate registration to:
- Confirm who qualifies for IHS-funded services
- Capture Medicaid, Medicare, and commercial coverage for third-party billing
- Enable continuity of care and data sharing across visits
This front-end process is critical for correctly routing encounters and protecting access for eligible AI/AN populations.
Step 2: Primary Care and Preventive Services Delivery
Once registered, patients receive care through team-based primary care models that often integrate:
- Medical, behavioral health, and dental services
- Preventive screening and chronic disease management
- Health education and community outreach
Care teams may include physicians, nurse practitioners, physician assistants, behavioral health clinicians, pharmacists, nurses, and community health workers. Many IHS and Tribal clinics adapt workflows to local realities such as geography, transportation barriers, and cultural practices.
Step 3: Care Coordination, Referrals, and Purchased/Referred Care (PRC)
IHS and Tribal clinics frequently coordinate referrals to external hospitals, specialists, and emergency services, especially when local capacity is limited. For certain services, they may use Purchased/Referred Care (PRC) arrangements to fund care delivered outside the facility.
This coordination includes:
- Determining when PRC or other funding sources can support outside services
- Communicating clinical information to receiving providers
- Managing follow-up back at the IHS or Tribal clinic after hospital or specialist encounters
- Vendors and partners working with IHS clinics often focus on referral workflows, transitions of care, and data exchange with regional systems.
Step 4: Data Reporting, Quality Programs, and Compliance
IHS and Tribal clinics participate in a mix of federal, state, and Tribal quality programs. These can include:
- IHS-specific clinical performance measures and reporting
- Medicaid and Medicare quality or value-based programs where applicable
- Public health reporting and community health surveillance
EHR infrastructure and reporting tools must support not only standard quality measures but also IHS- or Tribal-specific reporting expectations. For SaaS vendors, this means aligning data models and reporting logic to IHS requirements as well as broader programs that overlap with RHCs, FQHCs, and CAHs.
IHS Clinics in Billing, Reimbursement, and System Limitations
IHS and Tribal clinics use a blended financing model that combines direct IHS funding with third-party revenue from Medicare, Medicaid, and commercial payers. For B2B and revenue-cycle stakeholders, the key reality is that IHS dollars alone are not sufficient—capture of external reimbursement is essential to sustain services.
How the IHS Encounter-Based Reimbursement Model Works
Many IHS and Tribal clinics are paid under encounter-based or all-inclusive rates for certain payers, especially Medicaid and some Medicare arrangements:
- A single qualifying visit (encounter) generates one all-inclusive payment, regardless of the number of services provided in that visit.
- Coding is still required, but payment is tied to the encounter rather than every individual line item.
- The visit must meet encounter criteria (e.g., qualifying provider type, face-to-face rules, documented services).
This model simplifies some billing steps but raises others: visit definition, documentation standards, and correct identification of encounter-eligible providers become critical.
IHS Clinics, Medicare, Medicaid, and Commercial Billing
IHS and Tribal clinics typically bill:
- Medicaid under special IHS/Tribal encounter rates or FQHC-like structures
- Medicare for eligible services when beneficiaries have Medicare coverage
- Commercial payers when patients have private insurance
Key business implications:
- Enrollment and credentialing workflows must map IHS/Tribal facilities correctly in payer systems (similar to RHC and FQHC, but with distinct rules).
- Revenue-cycle systems must handle mixed methodologies (encounter-based for some payers, fee-for-service for others).
Benefits coordination is complex—many patients have IHS eligibility plus Medicaid and/or Medicare.
Payment Integrity and Documentation in IHS Settings
Even under encounter-based payment, documentation must:
- Support medical necessity and visit eligibility
- Identify the rendering provider and service mix
- Capture preventive, behavioral health, and chronic care management actions that may be measured in quality programs, even if they do not change the payment amount for that encounter
Weak documentation can still create risk—even when the payment doesn’t vary line-by-line—because auditors focus on whether the encounter met the requirements for an all-inclusive payment.
System Limitations and Revenue-Cycle Watch-Outs
Common pressure points for IHS and Tribal clinics include:
- Fragmented funding streams (IHS, Medicaid, Medicare, grants, PRC) that are hard to reconcile in a single revenue-cycle system
- EHR and billing platforms that are not optimized for encounter-based rules, leading to errors in visit qualification or bundling
- Complex payer rules for IHS/Tribal facilities that differ from standard RHC or FQHC policies
- Limited RCM staffing or high turnover in remote areas, which increases denial and underbilling risk
Vendors and partners need to design workflows that respect IHS-specific rules while still interoperating with mainstream Medicare and Medicaid systems.
How IHS Clinics Influence Quality, Access, and Equity in Healthcare
IHS and Tribal clinics are not just another provider type; they are a central infrastructure for health equity and sovereignty in AI/AN communities. Their design directly shapes who can access care, how culturally relevant that care is, and how well the broader system collaborates with Tribal nations.
IHS Clinics and Rural Access to Care
In many reservation and frontier settings, the IHS or Tribal clinic is:
- The primary, and sometimes only, local primary care provider
- The main access point for vaccinations, chronic disease follow-up, and urgent care
- A gateway to external hospitals, CAHs, and specialists via referrals and PRC
When IHS clinics are under-resourced or face staffing shortages, local access can deteriorate quickly, forcing patients to travel long distances or forgo care altogether.
Quality and Care Coordination in IHS Systems
IHS and Tribal clinics participate in quality programs that:
- Track chronic disease control (e.g., diabetes, hypertension)
- Monitor preventive screening rates
- Measure behavioral health and SUD treatment engagement
- Support transitions of care after hospitalizations
Because patients often receive specialty or inpatient care outside the IHS system, care coordination and data exchange with non-IHS hospitals, RHCs, and CAHs are critical to avoiding gaps, duplicate work, or unsafe transitions.
Equity, Sovereignty, and Cultural Relevance
IHS and Tribal health systems are grounded in Tribal sovereignty and treaty obligations, not just standard payer relationships. That has real implications for B2B partners:
- Care models are tailored to cultural, linguistic, and community realities rather than purely volume-driven metrics.
- Quality initiatives need to align with Tribal health priorities, not just generic national benchmarks.
- Technology and workflows must account for connectivity constraints, remote geography, and local workforce realities.
When external partners overlook these factors—treating IHS like a standard RHC or FQHC—they risk reinforcing inequities instead of reducing them.
Frequently Asked Questions about IHS
1. What is IHS (Indian Health Service)?
IHS (Indian Health Service) is a federal health system that provides medical care to eligible American Indian and Alaska Native (AI/AN) people through a network of hospitals, clinics, and health programs operated by IHS, Tribes, or Tribal organizations.
2. What is an IHS clinic?
An IHS clinic is a primary care or outpatient facility within the Indian Health system that delivers community-based care to AI/AN patients. It may be operated directly by IHS, by a Tribe under a “638” self-governance agreement, or as an Urban Indian Health Program.
3. How is an IHS clinic different from an RHC or FQHC?
IHS clinics primarily serve AI/AN communities and are tied to federal trust and treaty responsibilities, while Rural Health Clinics (RHCs) and Federally Qualified Health Centers (FQHCs) are safety-net clinic types defined by Medicare and Medicaid policy. Some Urban Indian programs may also function as FQHCs, but IHS-specific rules still apply.
4. How do IHS and Tribal clinics get paid?
They are funded through a combination of IHS appropriations, third-party billing (Medicaid, Medicare, commercial insurance), grants, and other program funds. Many use encounter-based or all-inclusive rates for certain payers instead of pure fee-for-service.
5. What services do IHS clinics typically provide?
Most IHS clinics offer primary care, preventive services, chronic disease management, women’s health, pediatric care, behavioral health, and care coordination. Some also provide dental, pharmacy, and community health worker programs based on local capacity.
6. What is a Tribal 638 clinic?
A Tribal 638 clinic is a facility operated by a Tribe or Tribal organization under the Indian Self-Determination and Education Assistance Act. It delivers services that might otherwise be run by IHS, with more local control over staffing, budgeting, IT, and payer contracting.
7. How do IHS clinics coordinate with outside hospitals and specialists?
IHS and Tribal clinics frequently refer patients to external hospitals, CAHs, specialists, and emergency departments. They may use Purchased/Referred Care (PRC) or other funding arrangements to pay for outside services and then manage follow-up back at the IHS or Tribal clinic.
