What is a NPPES (National Plan and Provider Enumeration System)?
The National Plan and Provider Enumeration System (NPPES) is the CMS-managed database that assigns and maintains National Provider Identifiers (NPIs) for healthcare providers and organizations in the United States. NPPES serves as the official source of record for NPI issuance, provider identity details, and taxonomy classifications that are used across Medicare, Medicaid, and commercial payer systems.
NPPES was created to support standardized provider identification across the healthcare ecosystem. When a clinician or healthcare entity applies for an NPI, NPPES collects and stores core information such as legal name, practice location, mailing address, taxonomy codes, and authorized contacts. This data feeds payer enrollment systems, claims processing, credentialing workflows, and provider directory listings.
In practice, NPPES is foundational to reimbursement and interoperability. Accurate, up-to-date NPPES records help prevent claim mismatches, enrollment delays, and directory errors, while also enabling payers and health IT platforms to reliably link providers to billing activity and care services.
Key Components of NPPES
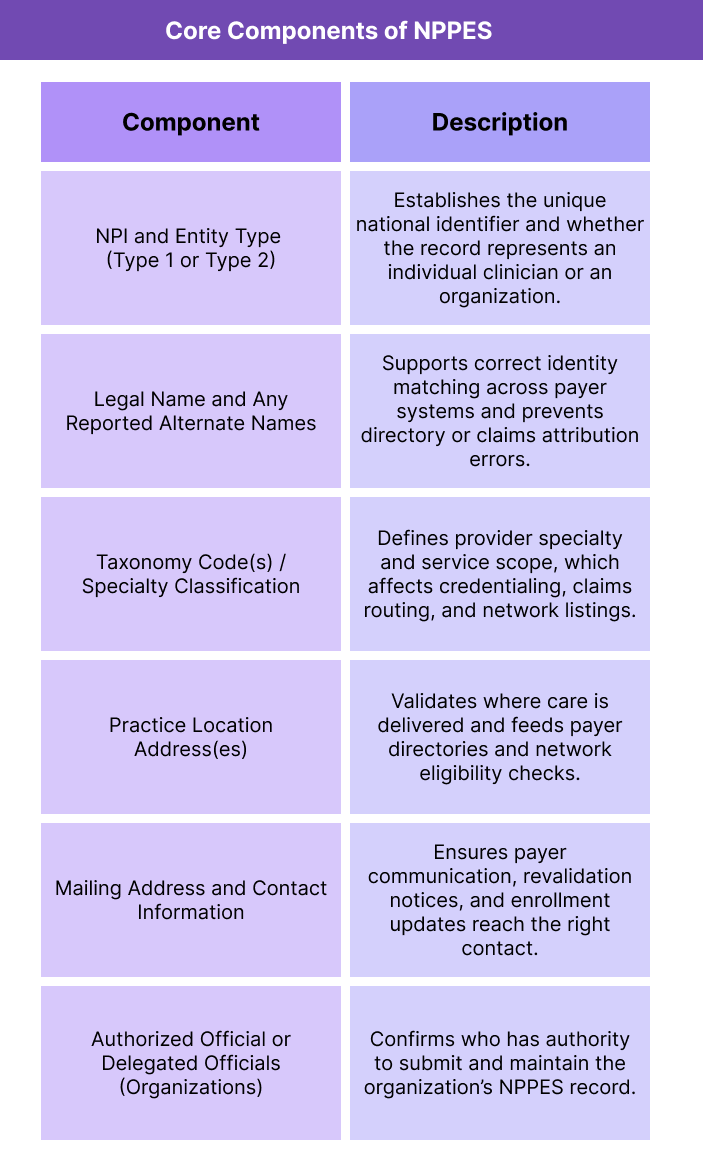
NPPES is designed to serve as the national source of truth for provider identity so that payers, health systems, and health IT platforms all reference the same standardized data when verifying a provider or processing claims. To do that, NPPES collects a specific set of data elements for every Type 1 (individual) and Type 2 (organization) NPI record and maintains those records over time.
The system plays two parallel roles: first, as the intake and maintenance portal where providers apply for and update their NPI; second, as the backend data source that powers the public NPI Registry and downloadable provider datasets used across the industry.
Required NPPES Provider Identity Information
NPPES records include core information that establishes who the provider is and how they are classified. This data ensures that claims, enrollment files, directories, and care coordination systems can reliably match activity to the correct entity.
Key identity elements include legal business name, entity type, taxonomy codes, and provider contact details. Because taxonomy codes define specialty and service type, they are critical for payer credentialing and correct claims routing.
Practice Location and Contact Data in NPPES
NPPES requires providers to enter both practice location and mailing address information. These fields are used by payers to validate where services are rendered or administered and are also pulled into provider directories to support patient access and network accuracy.
Organizations with multiple sites may list multiple practice locations, and maintaining accuracy across those entries helps prevent directory mismatches and reimbursement delays.
Updating NPPES Records Over Time
NPPES is not a one-and-done enrollment step. Providers are responsible for keeping their records current when changes occur, such as new practice locations, specialty shifts, name changes, ownership updates, or authorized official updates for organizations.
Outdated NPPES data is a common source of billing friction because payer systems depend on NPPES alignment to validate provider identity. Even small mismatches between payer files and NPPES records can trigger enrollment delays or claims rejection.
How NPPES Works in Practice
NPPES functions as the operational backbone of the NPI lifecycle. Providers and organizations use it to apply for an NPI, maintain their identity record over time, and publish standardized information that payers and health IT systems rely on for enrollment and claims validation.
At a workflow level, NPPES supports several practical use cases across the reimbursement and compliance ecosystem.
Step 1: NPI Application and Enumeration Through NPPES
When a clinician or healthcare organization needs an NPI, they submit an application through NPPES. The system collects required identity, specialty, and contact details, then issues a unique NPI tied to that record. For individuals, this is a Type 1 NPI. For organizations such as practices, clinics, or health systems, this is a Type 2 NPI.
Once issued, the NPI becomes the consistent identifier used across all payer and claims systems.
Step 2: Public Registry Publishing and Industry Use
NPPES automatically feeds the public NPI Registry and downloadable NPPES datasets. These data sources allow payers, credentialing platforms, and healthcare software vendors to verify provider identity, specialty taxonomy, and addresses.
For B2B systems, NPPES data is often used to auto-populate provider profiles, validate enrollment status, and support network directory accuracy.
Step 3: Ongoing Record Maintenance
Providers are expected to update NPPES when key changes occur, such as:
- Practice location or mailing address updates
- Legal name changes
- Specialty or taxonomy updates
- Organizational ownership or authorized official changes
Keeping NPPES aligned with real-world operations reduces mismatches that cause payer enrollment delays or claims rejection.
Step 4: Downstream Enrollment and Claims Alignment
While NPPES does not enroll providers into Medicare or commercial networks, it supplies the foundational identity data those enrollment systems depend on. If NPPES data conflicts with PECOS, MAC enrollment files, or payer credentialing records, providers often experience delays, rework requests, or billing interruptions.
In practice, organizations treat NPPES accuracy as a prerequisite for stable reimbursement workflows.
NPPES in Billing, Reimbursement, and System Limitations
NPPES is not a billing system, but it directly affects billing success because it is the upstream source of truth for provider identity and specialty classification. Payers use NPPES data to validate who is billing, what services they are eligible to provide, and whether claims match the enrolled provider record. Even small inconsistencies between NPPES and payer enrollment files can trigger delays, denials, or revalidation requests.
How NPPES Impacts Claims Processing and Payment
Most payer systems cross-check claim submissions against NPPES-derived identity fields, including legal name, NPI, and taxonomy. If a claim does not align with what NPPES shows for that provider, common outcomes include:
- Claims rejecting due to NPI or taxonomy mismatch
- Delayed payment while payer systems request corrections
- Incorrect provider attribution in reporting or value-based programs
- Directory and network listing errors that affect patient access
Because taxonomy codes in NPPES are used to define specialty and billing scope, they are especially important for ensuring services route correctly and are paid under the right provider classification.
Where NPPES Intersects With Medicare and Commercial Enrollment
NPPES is often confused with enrollment systems like PECOS. The difference is that NPPES assigns and maintains the NPI record, while enrollment systems determine whether that provider is approved to bill a specific payer. However, enrollment files are built from NPPES identity data.
That means NPPES errors usually show up downstream as enrollment friction, such as:
- Enrollment applications being returned for corrected identity fields
- Revalidation delays caused by outdated NPPES addresses or contacts
- Ownership or authorized official mismatches after organizational change
In practice, enrollment success depends on NPPES accuracy.
System Limitations and Operational Watch-Outs
NPPES is a foundational identity registry, not a real-time billing validator. Key limitations to understand include:
- NPPES does not confirm payer network enrollment or billing privileges
- Updates can take time to propagate into payer and vendor systems
- Taxonomy updates in NPPES may not automatically update payer credentialing
- NPPES data can be correct but still conflict with payer-side records if the payer has not synced
Because of these limitations, organizations should treat NPPES maintenance as a critical upstream workflow, but not assume that updating NPPES alone resolves enrollment or claims issues.
How NPPES Influences Quality, Access, and Equity in Healthcare
NPPES is often viewed as an administrative registry, but its data accuracy has real downstream effects on care quality, patient access, and equity. Because NPPES powers how providers are identified across payer networks and directories, it shapes whether patients can find care, whether claims process correctly, and whether quality programs attribute outcomes to the right clinicians.
How NPPES Supports Care Quality and Safety
Accurate NPPES records help ensure that clinical services are correctly attributed to the providers who delivered them. This matters for quality tracking, care coordination, and safety monitoring. When NPIs and taxonomy codes are correct, organizations can reliably link outcomes, follow-up responsibilities, and quality measures to the right care teams.
Conversely, mismatched or outdated NPPES data can create attribution gaps that weaken performance analysis and make it harder to identify where quality improvements are needed.
How NPPES Affects Patient Access to Care
NPPES feeds major provider directories and payer network listings. If a provider’s address, specialty, or status is incorrect in NPPES, that error often appears in public directories or insurer search tools. The result can be:
- Patients being routed to the wrong location
- Providers appearing under the wrong specialty
- Missing or incomplete listings in payer directories
- Delayed enrollment that limits when a provider can see covered patients
In this way, NPPES accuracy directly influences whether patients can identify and access in-network care.
How NPPES Can Influence Equity and Disparities
Directory accuracy is an equity issue. Populations with fewer provider options—such as rural communities, low-income areas, or patients seeking specialty access—are more affected by missing or incorrect provider listings. When NPPES data is incomplete, the patients who rely most on payer directories may face longer delays, fewer choices, or misdirected referrals.
Maintaining accurate NPPES data supports more reliable network representation and helps reduce avoidable access barriers that disproportionately affect vulnerable groups.
Frequently Asked Questions about NPPES
1. What is NPPES used for?
NPPES is used to issue and maintain National Provider Identifiers (NPIs) and to store standardized provider identity data, including legal name, addresses, and taxonomy codes. Payers and healthcare systems rely on NPPES data for enrollment verification and claims matching.
2. Is NPPES the same as the NPI Registry?
Not exactly. NPPES is the backend system that assigns and maintains NPI records. The public NPI Registry is a searchable front-end tool that displays NPPES data for verification and lookup.
3. How do providers apply for an NPI in NPPES?
Providers apply for an NPI by submitting an application through the NPPES portal. Once approved, NPPES issues a unique Type 1 NPI for individuals or a Type 2 NPI for organizations.
4. How often should NPPES information be updated?
Providers should update NPPES whenever key information changes, such as practice location, mailing address, legal name, taxonomy codes, or organizational authorized officials. Keeping NPPES current helps prevent payer enrollment delays and claim mismatches.
5. What happens if NPPES data is incorrect?
Incorrect NPPES data can lead to downstream problems such as payer enrollment rework, directory listing errors, or claims rejection due to NPI or taxonomy mismatches. Fixing NPPES issues early reduces reimbursement disruption.
6. What is the difference between NPPES and PECOS?
NPPES assigns and maintains the NPI and core provider identity record. PECOS is the Medicare enrollment system that determines whether a provider is approved to bill Medicare. PECOS enrollment relies on identity data sourced from NPPES, so mismatches between the two systems often cause enrollment delays.
7. What are taxonomy codes in NPPES?
Taxonomy codes in NPPES describe a provider’s specialty and service type. Payers use these codes to confirm billing scope, route claims correctly, and populate provider directories under the right specialty.
