What is a CHW (Community Health Worker)?
A Community Health Worker (CHW) is a frontline public health professional who serves as a trusted liaison between healthcare systems and the communities they support. CHWs are typically based in the communities they serve and are trained to provide culturally responsive health education, care navigation, and practical support that helps individuals access services, manage chronic conditions, and follow care plans. Their role is grounded in relationship-based engagement, often reaching patients who face barriers to traditional clinical care.
CHWs operate across a range of settings, including health systems, community-based organizations, public health departments, Medicaid programs, and value-based care initiatives. Their work may include outreach, screening support, health coaching, social needs assessment, care coordination reinforcement, and resource referral. Because CHWs understand local context and patient realities, they can improve communication, strengthen care continuity, and increase preventive service uptake.
From a quality and equity perspective, CHWs are an established workforce strategy for reducing disparities and improving access in underserved populations. They support health systems by extending care beyond the clinic, addressing social and behavioral drivers of health, and improving patient engagement in longitudinal care models such as Chronic Care Management, Maternal Health Programs, Behavioral Health Integration, and population health initiatives.
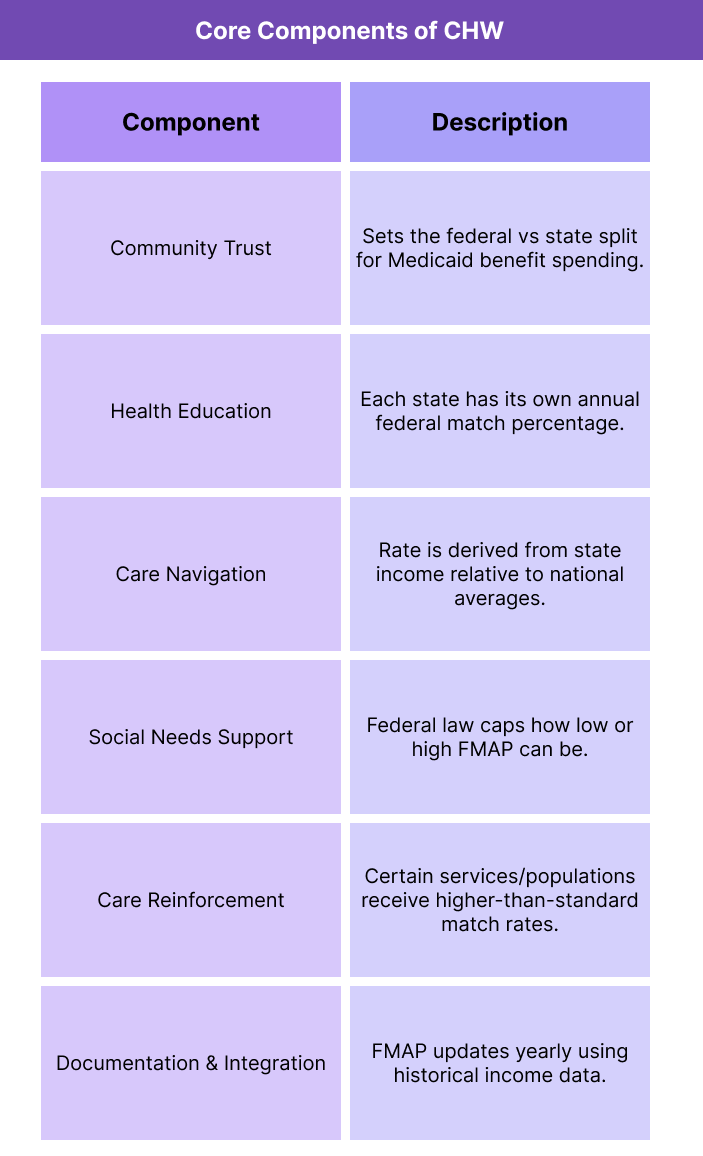
Key Components of a CHW
Community Health Workers (CHWs) function as a distinct, community-embedded workforce that extends health systems into everyday patient environments. Their effectiveness comes from combining trust-based relationships with practical support that helps individuals overcome barriers to care, especially in underserved populations.
While CHW programs vary by region and payer, most share common structural elements that define how CHWs operate, what services they provide, and how they integrate into clinical and community systems.
Community-Based Trust and Cultural Alignment
CHWs are typically recruited from the communities they serve, enabling shared language, lived experience, and cultural familiarity. This trust foundation is central to their ability to engage patients who may be hesitant to interact with formal healthcare systems.
Health Education and Coaching
CHWs deliver tailored health education that supports preventive care, chronic disease self-management, and treatment adherence. Education is often practical and behavior-focused, helping patients understand conditions, medications, and care plans in accessible terms.
Care Navigation and System Access Support
A core CHW function is helping patients navigate complex healthcare systems. This includes scheduling appointments, understanding benefits, preparing for visits, and connecting patients to the right level of care at the right time.
Social Needs Screening and Resource Connection
CHWs assess non-clinical barriers such as food insecurity, housing instability, transportation gaps, or utility needs. They connect patients to community resources, public benefits, and local support services that address these drivers of health.
Care Coordination Reinforcement
CHWs support care continuity by reinforcing clinical instructions and ensuring follow-through after visits. They often serve as support partners for nurses, care managers, or behavioral health teams in longitudinal care models.
Documentation and Program Integration
In structured CHW programs, CHWs document encounters, services provided, and social needs outcomes in health system tools or care management platforms. This supports accountability, continuity, and reimbursement alignment in Medicaid and value-based contracts.
How CHWs Work in Practice
Community Health Workers (CHWs) operate at the intersection of clinical care and community life, supporting patients in the environments where health decisions and barriers actually occur. In practice, CHWs extend the reach of healthcare teams by providing ongoing, non-clinical support that improves engagement, follow-through, and access to services.
1. Patients Are Identified Through Clinical or Community Pathways
CHWs may be assigned through referrals from primary care, care management teams, Medicaid health plans, hospitals, or community organizations. Patients are often selected because they face chronic disease burden, care gaps, social needs, or barriers to engaging with the healthcare system.
2. The CHW Builds Relationship and Trust
CHW work begins with establishing rapport. Through home visits, phone outreach, community meetings, or clinic-based interaction, CHWs create a trusted connection that allows patients to share concerns that may not surface in traditional clinical visits.
3. Health Risks and Social Needs Are Assessed
CHWs gather practical information about a patient’s daily realities, including access to food, housing stability, transportation, caregiver support, medication challenges, and understanding of care instructions. These insights help contextualize clinical risk.
4. Education and Coaching Support Behavior Change
Based on identified needs, CHWs provide accessible education on conditions, medications, lifestyle adjustments, and preventive actions. They often reinforce care plans over time, helping patients build confidence and self-management skills.
5. Care Navigation and Resource Linkage Occur
CHWs help patients access the right services by scheduling appointments, preparing patients for visits, explaining benefits, and connecting them to community supports such as transportation programs, food assistance, housing resources, or behavioral health services.
6. Ongoing Follow-Up Reinforces Continuity
CHWs maintain frequent touchpoints between clinical encounters. They check progress, troubleshoot barriers, and help patients stay engaged with long-term goals, especially for chronic disease management or post-discharge stabilization.
7. Information Flows Back to the Care Team
In integrated programs, CHWs document activities and communicate social needs or risk updates to nurses, care managers, or providers. This helps clinical teams adjust care plans and close gaps that would otherwise persist unnoticed.
CHWs in Billing, Reimbursement, and System Limitations
Community Health Workers (CHWs) are increasingly embedded in Medicaid, Medicare Advantage, and value-based care models, but their reimbursement pathways remain uneven across programs. While CHWs have longstanding clinical and public health value, payment structures often lag behind implementation, requiring organizations to understand state-specific rules and contract-specific allowances.
How CHW Services Are Funded
CHW services are most commonly funded through Medicaid mechanisms, including state plan amendments, waivers, managed care contracts, and grant-based programs. Some states recognize CHWs as reimbursable providers for defined preventive or care coordination functions, while others support CHW programs through health plan capitation or public health allocations. In Medicare and commercial markets, CHW funding is more often tied to value-based payment arrangements rather than direct fee-for-service billing.
Billing Pathways for CHW-Related Work
When CHW services are reimbursable, billing typically occurs through structured program codes, delegated care management benefits, or “in-lieu-of” service categories under managed care. In many models, CHW work is billed indirectly under the supervising organization or care management umbrella rather than as independent clinician billing. Successful billing depends on clear role definition, approved service scope, and compliant documentation.
Documentation Expectations and Audit Considerations
Even when CHW work is not billed directly, documentation is essential for proving program value and supporting payment within risk-based contracts. CHW documentation commonly includes encounter notes, social needs findings, education topics delivered, referrals made, patient goals, and follow-up outcomes. In Medicaid programs where CHWs are reimbursable, insufficient documentation or scope mismatch can create recoupment risk.
Scope of Practice and Credentialing Limits
CHWs are non-licensed professionals in most jurisdictions, meaning their reimbursable scope is limited to non-clinical support functions such as education, navigation, and social needs linkage. Some states require CHW certification or formal training for reimbursement eligibility, while others allow broader program-defined roles. Organizations must align job duties to the recognized scope to prevent compliance vulnerabilities.
Operational Constraints and Sustainability Challenges
CHW programs can face sustainability barriers when reimbursement is fragmented or dependent on time-limited grants. Programs without stable payment streams may experience staffing turnover, inconsistent integration into care teams, or limited capacity to scale. Health systems must often invest in supervision, training, and workflow design before financial returns become visible.
System Limitations in Measuring CHW ROI
Traditional fee-for-service systems are not designed to capture the value of CHW work, which is often preventive, longitudinal, and socially oriented. Outcomes like improved trust, reduced barriers, and better care follow-through may take time to translate into measurable cost savings. This lag can make it harder for organizations to defend ongoing funding without strong evaluation frameworks.
How CHWs Influences Quality, Access, and Equity
Community Health Workers (CHWs) are widely recognized as a workforce strategy that improves care quality and closes access gaps by addressing barriers that sit outside traditional clinical workflows. Their impact is strongest in longitudinal and community-based models where trust, follow-through, and social risk mitigation determine clinical outcomes.
CHWs and Patient-Centered Quality Improvement
CHWs improve quality by reinforcing care plans, supporting medication adherence, and helping patients understand how to manage chronic conditions day to day. Their continuous, relationship-based engagement reduces care fragmentation and increases the likelihood that patients complete recommended preventive services and follow-up visits.
Access to Care Through Care Navigation
CHWs increase access by helping patients overcome logistical and system-level obstacles. They assist with appointment scheduling, transportation coordination, benefit understanding, and referral completion, ensuring that patients reach appropriate services earlier and more consistently—especially when healthcare systems are complex or difficult to navigate independently.
Reducing Preventable Utilization
By intervening early on care gaps and social risks, CHWs can reduce avoidable emergency department use, preventable hospitalizations, and missed follow-up after discharge. Their role in stabilizing patients within community settings supports more efficient use of healthcare resources while maintaining continuity.
Advancing Health Equity and Trust
CHWs are uniquely positioned to reduce disparities because they are culturally aligned with the populations they serve and often share lived experience with patients. This trust helps address historical mistrust of healthcare institutions and improves engagement among communities that have experienced systemic barriers or discrimination.
Addressing Social Drivers of Health
CHWs directly influence equity by identifying and responding to social drivers such as food insecurity, housing instability, transportation gaps, caregiver strain, and safety concerns. When these needs are addressed, clinical interventions become more effective and sustainable, especially for high-risk Medicaid and Medicare populations.
Impact in Rural and Underserved Communities
In rural and medically underserved areas, CHWs help extend limited clinical capacity by providing consistent outreach and care reinforcement where provider shortages and geographic barriers are common. They can serve as a stabilizing access layer for populations that might otherwise disengage from care due to distance, cost, or system fatigue.
Frequently Asked Questions about CHWs
1. What is a CHW?
A Community Health Worker (CHW) is a frontline public health professional who supports patients through health education, care navigation, and social needs assistance. CHWs build trusted relationships in the communities they serve and help connect individuals to services and resources that improve health outcomes.
2. What does a Community Health Worker do in healthcare?
CHWs provide non-clinical support such as outreach, patient coaching, care plan reinforcement, appointment navigation, and connections to community resources. Their work helps patients overcome barriers to engaging in care.
3. How are CHWs different from nurses or care managers?
CHWs are typically non-licensed and community-embedded, focusing on trust-building, education, navigation, and social needs support. Nurses and care managers are licensed clinicians who deliver clinical assessment and medical management.
4. Where do CHWs work?
CHWs work in hospitals, primary care practices, Medicaid and Medicare Advantage programs, community-based organizations, public health departments, and value-based care initiatives.
5. Are CHWs reimbursable under Medicaid or Medicare?
CHW reimbursement is more common in Medicaid than Medicare. Some states reimburse CHW services through state plan amendments, waivers, or managed care contracts. Medicare reimbursement is usually indirect through value-based or population health models.
6. Do CHWs need certification?
Certification requirements vary by state and program. Some Medicaid or health system programs require CHW certification or approved training, while others allow CHW practice based on employer-defined competencies.
7. What kinds of patients benefit most from CHW support?
CHWs are especially effective for patients with chronic conditions, high social risk, care access barriers, frequent hospital use, or low engagement with clinical systems.
8. How do CHWs support chronic disease management?
CHWs reinforce care plans, provide coaching on self-management, help patients adhere to medications, and address day-to-day barriers that make chronic disease harder to control.
9. What role do CHWs play in addressing social drivers of health?
CHWs screen for needs like food insecurity, housing instability, transportation gaps, and financial stress. They connect patients to community resources and benefits that reduce these barriers.
10. How do CHWs improve health equity?
Because CHWs are often culturally aligned with the communities they serve, they build trust, improve communication, and help reduce disparities caused by system barriers, mistrust, or uneven access.
11. Can CHWs reduce hospitalizations or ER visits?
Yes. By improving follow-through, addressing social needs, and stabilizing patients between visits, CHWs can reduce avoidable emergency department use and preventable admissions.
12. How do CHWs fit into value-based care models?
CHWs extend care beyond the clinic, improve preventive engagement, and help manage total cost of care. Their services support quality measures and outcomes-based reimbursement.
