What is an MUA (Medically Underserved Area)?
A Medically Underserved Area (MUA) is a federal designation used by the Health Resources and Services Administration (HRSA) to identify geographic regions where residents face significant barriers to accessing primary care services.
MUA status is determined using the Index of Medical Underservice (IMU)—a scoring methodology that evaluates provider availability, population characteristics, poverty, and health outcomes to measure overall access need.
In addition to area-level designation, HRSA may also assign Medically Underserved Population (MUP) status, which applies the same criteria to specific underserved groups within a community—such as low-income residents, Medicaid-eligible individuals, migrant workers, or other vulnerable populations.
MUA and MUP designations help federal and state agencies allocate critical resources to areas experiencing:
- Insufficient primary care provider supply
- High poverty and socioeconomic barriers
- Elevated infant mortality or chronic disease burden
- Limited local healthcare infrastructure
- Geographic isolation or travel burdens
MUA/MUP status plays an important role in:
- Federally Qualified Health Center (FQHC) eligibility
- Expansion of safety-net services
- Grant funding, community health planning, and workforce programs
- Identification of access gaps and structural inequities in healthcare delivery
While HPSAs identify workforce shortages, MUA/MUP designations assess broader community need, making them complementary tools for addressing underserved access across the United States.
Key Components of Medically Underserved Areas (MUAs)
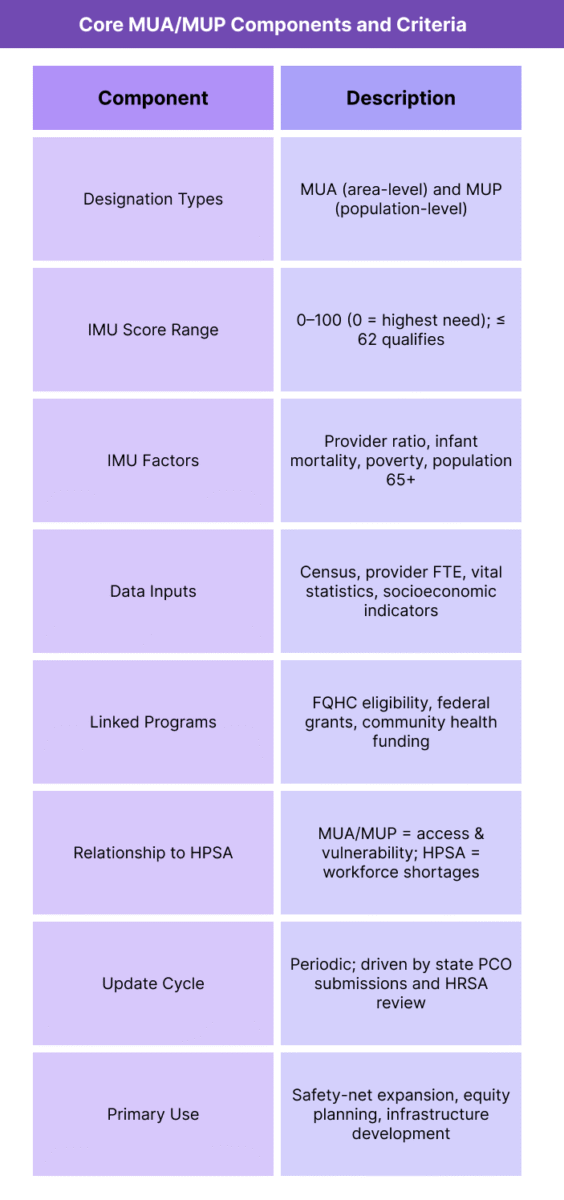
Medically Underserved Areas (MUAs) are identified through a structured federal evaluation process designed to measure broad access barriers—not only provider shortages, but also socioeconomic challenges, health outcomes, and community vulnerability.
The designation guides federal funding, FQHC eligibility, and national strategies to strengthen primary care access in underserved communities.
Below are the core elements that define MUA/MUP designation, scoring, and operational relevance.
1. MUA vs. MUP Designation Types
- HRSA assigns two related designation types:
- Medically Underserved Area (MUA)
A geographic area—such as a county, group of counties, or census tract—with significant barriers to primary care access. - Medically Underserved Population (MUP)
A specific population within a community that experiences disproportionate access challenges, such as:- Low-income residents
- Medicaid-eligible populations
- Migrant or seasonal farmworkers
- Homeless populations
- Native/Tribal communities
- Medically Underserved Area (MUA)
- Both designations use the same scoring criteria to measure need.
2. Index of Medical Underservice (IMU)
- MUAs and MUPs are defined through the Index of Medical Underservice (IMU), a composite score from 0 to 100, where 0 = highest need and 100 = lowest need.
- An IMU score of 62.0 or below qualifies an area or population for MUA/MUP designation.
- The IMU evaluates four weighted factors:
- Primary Care Provider Ratio – Fewer clinicians per population indicates higher need.
- Infant Mortality Rate – Higher mortality signals greater health vulnerability.
- Percent of Population Below Poverty Level – Measures socioeconomic barriers to accessing care.
- Population Age 65+ – Assesses need based on aging demographics.
- This holistic approach captures structural inequities beyond raw provider counts.
3. Data Sources for MUA/MUP Determination
- State Primary Care Offices (PCOs) and HRSA use:
- State licensing board data
- Census and socioeconomic datasets
- Vital statistics (“infant health”) data
- Local health department assessments
- Community health needs assessments (CHNAs)
- Provider FTE verification
- These inputs guide both scoring and periodic updates.
4. Federal Programs Linked to MUA/MUP Status
- MUA/MUP designation determines eligibility for several critical access and safety-net programs:
- FQHC certification and Section 330 funding
- Targeted grants for primary care expansion
- Workforce pipeline programs in underserved communities
- Telehealth expansion support
- Community health infrastructure funding
- Maternal and child health initiative alignment
- While HPSAs drive workforce incentives, MUAs/MUPs support safety-net infrastructure.
5. Use in Community Health Planning
- Local planning organizations—including hospitals, public health agencies, and community health centers—use MUA/MUP data to:
- Identify service gaps
- Prioritize underserved census tracts
- Build primary-care, dental, and behavioral health capacity
- Support grant applications and strategic initiatives
- Inform health equity programs and resource distribution
- Because the IMU incorporates social determinants of health, it effectively guides equitable planning.
6. Relationship With HPSA Designations
- MUA/MUP and HPSA designations often overlap but serve different federal priorities:
- HPSA = Workforce shortage measurement
- MUA/MUP = Community vulnerability and access measurement
- Many areas hold both designations, especially rural counties and urban low-income neighborhoods.
7. Review, Maintenance, and Updates
- HRSA reviews MUA/MUP data periodically, and states may request:
- Redesignation
- Boundary updates
- New population group evaluations
- Expansion to adjacent underserved areas
- Community changes—clinic closures, demographic shifts, and provider departures—can trigger reevaluation.
How Medically Underserved Areas (MUAs) Work in Practice
Medically Underserved Areas (MUAs) and Medically Underserved Populations (MUPs) serve as core federal access-designation tools used across healthcare operations, community planning, funding decisions, and safety-net expansion.
While HPSAs primarily guide workforce incentives, MUA/MUP designations guide infrastructure investments and determine eligibility for critical access programs such as FQHC certification and Section 330 funding.
Below is the practical workflow for how MUA/MUP status is used by providers, public health agencies, community organizations, and federal programs.
Step 1: Community Needs Assessment and Data Submission
- State Primary Care Offices (PCOs), local health departments, and community health organizations:
- Identify access gaps in primary care, maternal health, dental, and behavioral health
- Collect socioeconomic and demographic data
- Gather provider FTE information and validate practice locations
- Monitor infant mortality, poverty levels, and aging trends
- Submit data to HRSA for MUA/MUP scoring and designation consideration
- Local health needs assessments (CHNAs) often trigger new MUA/MUP applications.
Step 2: FQHC Eligibility and Safety-Net Expansion
- MUA/MUP designation is the key federal requirement for:
- Federally Qualified Health Center (FQHC) certification
- Section 330 grant eligibility
- Funding for new access points (NAPs)
- Expansion of primary care, dental, and behavioral health service lines
- Health systems and community organizations use MUA/MUP designations to support:
- Opening new clinics in underserved neighborhoods
- Adding dental and behavioral health capacity
- Securing federal operational and capital grants
- Without MUA/MUP status, many communities would not qualify for FQHC support.
Step 3: Workforce Recruitment and NHSC Placement
- While HPSA scores primarily determine NHSC prioritization, MUA/MUP status influences:
- Eligibility for NHSC sites that are not auto-HPSAs
- Placement of clinicians into community health centers
- Recruitment packages for underserved urban populations
- Behavioral health and primary care pipeline development
- Facilities located in MUAs/MUPs often partner with state workforce offices to secure competitive placements.
Step 4: Grant Funding, Resource Allocation, and Program Eligibility
- Federal and state agencies use MUA/MUP designations to award:
- Community health center grants
- Maternal and child health grants
- Telehealth access funding
- Rural and frontier health grants
- Opioid and behavioral health treatment funds
- Infrastructure modernization support
- MUA/MUP status strengthens grant applications by confirming objective federal need.
Step 5: Local Health Planning and Service-Line Decisions
- Hospitals, CAHs, and health systems use MUA/MUP data to:
- Guide strategic planning and community service expansions
- Identify neighborhoods needing mobile clinics, CHWs, or home-based outreach
- Expand primary care, dental, and pediatric service lines
- Design interventions for low-income residents and vulnerable populations
- Build partnerships with FQHCs and social services organizations
- MUA/MUP criteria align closely with the social determinants of health, making them essential to community-based planning.
Step 6: Public Health Preparedness and Policy Development
- MUA/MUP designations are used by public health agencies to prioritize:
- Primary care access during outbreaks and emergencies
- Vaccination resource distribution
- Emergency planning for vulnerable populations
- Long-term community resilience initiatives
- Areas with MUA/MUP status are frequently prioritized for federal response funding.
Step 7: Monitoring Community Changes and Re-Designation
- Communities must continuously monitor:
- Provider additions or departures
- Clinic openings or closures
- Changes in population density or demographics
- Poverty and infant mortality trends
- Healthcare utilization shifts
- These changes may prompt states or local coalitions to request re-designation or updated scoring from HRSA.
Step 8: Integration With Equity and Rural Access Programs
- Because MUA/MUP calculations incorporate poverty, infant health, and aging demographics, they integrate into programs addressing:
- Health equity
- Rural access disparities
- Tribal and frontier health
- Access for immigrant and migrant populations
- Medicaid expansion strategies
- Telehealth modernization
- Chronic disease management initiatives
- This makes MUA/MUP designations central to federal equity frameworks.
MUAs in Billing, Reimbursement, and Compliance Limitations
Unlike HPSAs, Medically Underserved Area (MUA) and Medically Underserved Population (MUP) designations do not directly modify Medicare Part B reimbursement or trigger automatic provider bonuses.
Instead, MUA/MUP status influences institutional billing structures, primarily through eligibility for Federally Qualified Health Center (FQHC) designation and broader Medicaid and safety-net funding.
Because MUAs/MUPs reflect socioeconomic vulnerability rather than workforce ratios alone, reimbursement implications are indirect but still significant for clinics and health systems operating in underserved communities.
How MUA/MUP Status Affects Reimbursement
Although MUAs don’t change fee schedule amounts, they determine eligibility for FQHC certification, which carries major reimbursement implications:
- 1. Prospective Payment System (PPS) Rates for FQHCs
FQHCs receive:- A national, encounter-based PPS rate
- Annual inflation adjustments
- Wraparound payments when Medicaid MCO rates fall below PPS
- Enhanced payment stability compared to standard outpatient clinics
Because only clinics located in MUAs/MUPs (or HPSAs) can qualify as FQHCs, MUA designation indirectly drives higher, more predictable reimbursement for safety-net providers.
- 2. Medicaid Enhanced Payments
States may use MUA/MUP data to:- Increase Medicaid PPS wraparound support
- Prioritize safety-net expansions
- Direct targeted maternal, dental, and behavioral health funding
- Approve new Rural Health Clinics (RHCs)
- 3. HRSA Section 330 Grant Funding
FQHCs serving MUAs/MUPs may receive:- Operating grants
- Capital development awards
- Behavioral health integration support
- Workforce funding tied to population need
These grants significantly augment financial stability—and they require MUA/MUP documentation.
Reimbursement Challenges for Providers in MUAs/MUPs
- Despite access to safety-net programs, clinics in MUAs/MUPs face notable financial constraints:
- High uncompensated care due to insurance instability
- Lower commercial payer penetration than non-underserved areas
- Higher reliance on Medicaid, with state-dependent payment structures
- Greater overhead associated with social determinants of health
- Higher care coordination burden for complex patients
- Even with PPS or enhanced Medicaid payments, many MUAs operate with tight margins.
Medicaid Variation and Payment Limitations
- Medicaid policy varies widely by state, affecting MUA-located clinics in important ways:
- Some states fully fund FQHC wraparound payments; others fall behind on timeliness
- Dental and behavioral health reimbursement varies greatly
- States determine whether mobile clinics, school-based clinics, or sub-sites are eligible for PPS
- Medicaid expansion status influences payer mix and revenue stability
- This state-by-state divergence affects financial sustainability for clinics serving MUA populations.
Limitations of IMU Scoring in Reimbursement Policy
- The Index of Medical Underservice (IMU) is widely used but has notable constraints:
- Static scoring model—only four factors (provider ratio, poverty, infant mortality, age 65+)
- Does not account for modern access barriers such as broadband, behavioral health gaps, or transportation
- Relies on datasets that may lag 2–3 years behind current conditions
- Does not differentiate severity gradations within sub-county regions
- Does not reflect community-level clinic closures or new developments in real time
- This can result in:
- High-need areas lacking designation
- Low-need areas retaining designation longer than appropriate
- Inconsistent alignment with real-world need compared to HPSA scoring
- Despite limitations, IMU remains the gateway for FQHC eligibility and major federal funding.
- Interactions With HPSAs and Overlapping Designations
- Areas may hold:
- HPSA only
- MUA/MUP only
- Both HPSA and MUA/MUP
- Neither
- Overlap affects financial impact:
- HPSA → Medicare 10% bonus
- MUA/MUP → FQHC eligibility and infrastructure funding
- Areas with only MUA/MUP designation may not receive direct Medicare bonuses, despite high unmet need.
Equity and Funding Limitations
- Even with safety-net enhancements, MUAs face structural financial challenges:
- Persistent workforce shortages (HPSA solves only part of the issue)
- Limited specialty care availability
- Transportation and geographic barriers that PPS cannot solve
- Higher administrative costs for care coordination
- Greater chronic disease burden among residents
- Lower local tax base to support public health initiatives
- Thus, reimbursement improvements help—but do not fully offset the access barriers MUA/MUP communities experience.
Key Takeaway
MUA/MUP designation does not directly increase provider reimbursement under Medicare—but it unlocks the infrastructure, grant funding, and PPS payment pathways that sustain safety-net providers in underserved areas.
However, IMU scoring limitations, Medicaid variation, and socioeconomic barriers often constrain financial stability, demonstrating the need for continued policy innovation to support equitable access.
MUAs and Their Impact on Quality, Access, and Equity in Healthcare
Medically Underserved Areas (MUAs) and Medically Underserved Populations (MUPs) are core federal designations used to highlight communities experiencing the deepest structural barriers to primary care access.
Because MUAs incorporate socioeconomic factors, infant health outcomes, and population demographics—not just provider supply—they serve as one of the most equity-focused tools in federal health policy.
MUA/MUP designations help policymakers, health systems, and community organizations identify where the healthcare system is failing underserved populations and where targeted investment can drive the greatest impact.
Identifying Structural Barriers to Primary Care Access
- The Index of Medical Underservice (IMU) reveals multi-layered inequities in:
- Poverty and economic instability
- Infant mortality and maternal health disparities
- Older adult care needs
- Limited access to preventive and chronic-care services
- Geographic barriers and insufficient local infrastructure
- MUAs help illuminate socioeconomic drivers of poor health outcomes, moving beyond raw provider ratios to include broader vulnerability indicators.
Strengthening the Safety-Net Through FQHC Expansion
- MUA/MUP designation is foundational to FQHC eligibility, which supports:
- Community-based primary care in high-need areas
- Culturally competent and linguistically appropriate services
- Integrated behavioral health and dental care
- Sliding-fee discounts for low-income patients
- Care management and enabling services
- Chronic disease management programs tailored to underserved populations
- FQHCs are one of the most effective mechanisms for reducing disparities in access, outcomes, and preventive care.
Improving Access in Rural, Frontier, and Urban Underserved Communities
- MUAs cover diverse geographies:
- Rural/frontier regions with provider shortages and long travel distances
- Urban neighborhoods with concentrated poverty, housing instability, and insufficient local clinics
- Immigrant and migrant communities with cultural and linguistic barriers
- Tribal and reservation communities with limited infrastructure and high chronic disease prevalence
- This versatility helps MUAs support both rural and urban equity strategies.
Advancing Maternal, Infant, and Childhood Health Equity
- Because infant mortality is a key IMU factor, MUA designation highlights areas where:
- Prenatal care is limited
- High-risk pregnancies lack local obstetric services
- Infants experience poor birth outcomes
- Pediatric primary care access is insufficient
- These insights help align federal and state programs such as:
- Maternal and Child Health Block Grants
- Healthy Start
- HRSA’s rural maternal health initiatives
- MUAs directly support interventions across the reproductive and pediatric care continuum.
Supporting Behavioral Health Expansion
- MUA and MUP designations frequently overlap with behavioral health shortages, guiding investments in:
- Integrated behavioral health within FQHCs
- Substance use disorder (SUD) programs
- Tele-behavioral health expansion
- Crisis stabilization services
- Workforce pipelines for high-need populations
- Given the national mental health crisis, MUAs help target behavioral health investments where they are most urgently needed.
Guiding Federal and State Equity Funding
- MUAs inform prioritization for:
- Community health worker (CHW) programs
- Telehealth infrastructure grants
- Transportation and mobile-clinic initiatives
- School-based health centers
- Health equity demonstration projects
- Social determinants of health (SDOH) interventions
- Communities with MUA/MUP designations often qualify for a broader array of federal and state equity programs.
Limitations and Remaining Equity Gaps
- Despite the benefits, MUAs face persistent challenges:
- IMU criteria may not fully capture behavioral health or specialty-care shortages
- Scoring may lag behind real-world change
- Communities can lose designation even while still experiencing unmet need
- Medicaid reimbursement limitations reduce financial sustainability
- FQHCs alone cannot solve specialty and hospital-level access gaps
- Transportation, broadband, and housing barriers remain outside the scope of MUA policy
- These gaps underscore the need for integrated, multi-sector equity strategies.
Key Insight
MUA/MUP designations are powerful federal tools for identifying and addressing structural inequities in primary care access.
They support the expansion of FQHCs, guide major equity investments, and illuminate communities where socioeconomic vulnerability and limited healthcare infrastructure most severely impact outcomes.
However, MUAs are just one component of a broader ecosystem of rural and underserved access programs. Sustained progress requires aligning MUA/MUP strategies with HPSA designations, Medicaid policy, and community-level social support initiatives.
Frequently Asked Questions about Medically Underserved Areas (MUAs
1. What is a Medically Underserved Area (MUA)?
A Medically Underserved Area (MUA) is a federal designation used by HRSA to identify geographic regions with significant barriers to accessing primary care. MUAs are determined using the Index of Medical Underservice (IMU), which evaluates provider supply, poverty levels, infant mortality, and the percentage of residents age 65+.
2. What is a Medically Underserved Population (MUP)?
A Medically Underserved Population (MUP) is a specific population group within a community—such as low-income residents, Medicaid-eligible individuals, migrant farmworkers, or homeless populations—that experiences reduced access to care. MUPs use the same IMU scoring criteria as MUAs.
3. How does HRSA calculate MUA/MUP eligibility?
HRSA uses the IMU score (0–100), incorporating four factors:
- Primary care provider-to-population ratio
- Infant mortality rate
- Percentage of residents below the federal poverty level
- Percentage of the population age 65+
An IMU score ≤ 62.0 qualifies an area or population for MUA/MUP designation.
4. What is the difference between an MUA and an HPSA?
- MUA/MUP identifies community vulnerability and access barriers using socioeconomic and demographic data.
- HPSA identifies workforce shortages using provider-to-population ratios and access measures.
They often overlap but serve different federal policy functions.
5. Does MUA designation affect Medicare reimbursement?
No. MUA/MUP status does not directly change Medicare fee-for-service rates or provide a bonus.
However, MUA designation is a core requirement for FQHC eligibility, which gives clinics access to:
- FQHC PPS reimbursement
- Medicaid wraparound payments
- HRSA Section 330 operating grants
These funding mechanisms indirectly improve financial stability.
6. How does MUA status support FQHC development?
To qualify as an FQHC or FQHC look-alike, a clinic must be located in—or serve—a designated MUA or MUP.
This allows access to:
- Federal grant funding
- PPS reimbursement
- Sliding fee discount programs
- Integrated behavioral health and dental expansion funds
MUA/MUP status is foundational to safety-net infrastructure.
7. How often are MUA/MUP designations updated?
HRSA reviews designations periodically, generally every few years, but updates can occur sooner if:
- Provider supply changes
- Clinics open or close
- Community demographics shift
- State Primary Care Offices request reevaluation
Designation is not static and may change with evolving conditions.
8. Do MUAs affect Medicaid reimbursement?
Indirectly. While MUAs do not change Medicaid rates themselves, they influence:
- Eligibility for Medicaid PPS wraparound payments
- State decisions about telehealth expansion
- Maternal and behavioral health program funding
- Safety-net prioritization for high-need areas
State policies vary widely.
9. Can a community lose its MUA designation?
Yes. Areas or populations may lose status if:
- Provider supply increases
- Poverty or infant mortality rates improve
- Clinics expand or relocate
- Data updates increase IMU scores above 62
Loss of designation can impact FQHC funding and safety-net eligibility.
10. Why are MUAs important for health equity?
MUA/MUP designations help federal and state agencies direct resources to communities facing the highest barriers to primary care access—often low-income, rural, tribal, or socially marginalized populations.
They guide investments that improve preventive care, reduce disparities, and expand community health infrastructure.
