What are What are NCDs (National Coverage Determinations) in Healthcare?
National Coverage Determinations (NCDs) are federally binding Medicare coverage policies issued directly by the Centers for Medicare & Medicaid Services (CMS) that establish whether a medical service, procedure, device, or technology is reasonable and necessary for all Medicare beneficiaries nationwide.
Unlike Local Coverage Determinations (LCDs)—which vary by Medicare Administrative Contractor (MAC) jurisdiction—NCDs apply uniformly across every state and region, ensuring consistent coverage rules regardless of where a service is furnished.
NCDs define national policy for:
- Covered indications
- Non-covered indications and exclusions
- Clinical evidence requirements
- Documentation and coding expectations
- Limitations and frequency guidelines
- Device- or diagnostic-specific conditions of coverage
CMS develops NCDs when a service has broad national impact, significant clinical or technological implications, or when variation in regional policy may lead to inconsistent access across the country.
NCDs override all conflicting LCDs and MAC-level guidance. When an NCD exists, MACs must follow its provisions exactly when adjudicating claims, applying prepayment edits, or conducting medical necessity reviews.
NCDs are particularly common for:
- Advanced diagnostic imaging
- Molecular testing and genomics
- Durable medical equipment (DME) categories
- Cardiovascular and neurologic interventions
- New or emerging medical technologies
- Preventive services and screenings
- Drugs administered incident-to physician services
While NCDs ensure nationwide consistency, they are updated far less frequently than LCDs, which can create gaps that MACs fill with local coverage policy until CMS issues a new or revised NCD.
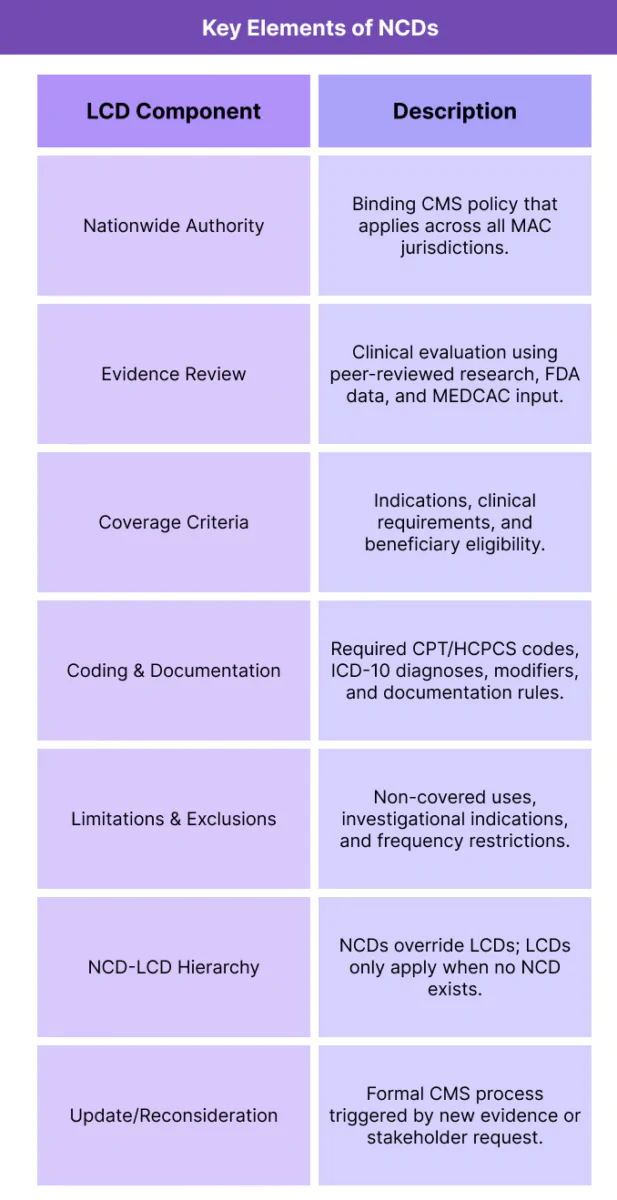
Key Components of National Coverage Determinations (NCDs)
National Coverage Determinations (NCDs) establish nationwide Medicare coverage rules for specific services, based on CMS’s formal evaluation of clinical evidence, risk–benefit profiles, and statutory requirements.
Because they apply uniformly across all MAC jurisdictions, NCDs serve as the highest level of Medicare coverage authority—defining when services must be covered, when they must not be covered, and what clinical criteria must be met for payment.
1. Nationwide Coverage Authority
- NCDs are issued directly by CMS Central Office, not by MACs.
- They are binding on all contractors, regardless of jurisdiction.
- MACs cannot modify, reinterpret, or selectively enforce NCD provisions.
- When an NCD exists, it supersedes all Local Coverage Determinations (LCDs) and local contractor guidance.
- This uniformity is essential for ensuring consistent access to key services for all Medicare beneficiaries.
2. Evidence-Based Evaluation Process
- CMS develops NCDs through a rigorous evaluation that may include:
- Systematic review of peer-reviewed clinical evidence
- Assessment of clinical utility and diagnostic accuracy
- Consideration of FDA approvals, safety data, and labeling
- Review of practice guidelines and specialty society recommendations
- Public comment periods and Medicare Evidence Development & Coverage Advisory Committee (MEDCAC) input
- This process ensures NCDs reflect robust, evidence-based conclusions.
3. National Coverage Criteria and Clinical Indications
- NCDs define:
- Covered clinical indications (conditions, risk factors, severity criteria)
- Non-covered indications or investigational uses
- Beneficiary eligibility requirements
- Prerequisite testing or prior interventions
- Frequency limits for repeat testing or treatment
- These criteria form the basis of MAC claim adjudication nationwide.
4. Documentation and Coding Requirements
- NCDs include specific coding and documentation expectations, such as:
- Required CPT®/HCPCS codes
- Associated ICD-10 diagnosis codes
- Required modifiers or billing conditions
- Documentation elements needed to substantiate coverage
- Technical component vs professional component billing distinctions (when applicable)
- Because NCDs are binding, these requirements must be followed exactly.
5. Limitations, Non-Covered Uses, and Exclusions
- NCDs commonly outline:
- Conditions where the service is not reasonable or necessary
- Clinical scenarios where evidence does not support benefit
- Safety concerns or investigational uses
- Situations where coverage is explicitly prohibited
- These limitations drive both claim denials and audit enforcement.
6. Interaction With LCDs and MAC Adjudication
- The relationship is hierarchical:
- If an NCD exists → LCDs cannot contradict it.
- If no NCD exists → MACs may issue LCDs.
- If both exist → NCD governs; LCD may clarify operational details but cannot modify coverage.
- Understanding this hierarchy is essential for correct billing and appeals.
7. Update, Reconsideration, and Public Process
- NCDs undergo formal reconsideration when:
- New evidence emerges
- FDA issues new approvals
- Specialty societies request updates
- CMS identifies gaps or inconsistencies
- Stakeholders file a reconsideration request
- Revisions often take months to years, which is why LCDs frequently fill interim policy gaps.
How National Coverage Determinations (NCDs) Work in Practice
National Coverage Determinations (NCDs) function as the highest level of Medicare coverage authority, guiding clinical teams, coding and billing staff, and compliance departments in determining whether a service is covered nationwide.
While LCDs address regional nuances, NCDs define universal rules, making them central to consistent and defensible reimbursement practices across all Medicare jurisdictions.
Because NCDs dictate when services are payable and medically necessary, they are referenced throughout the entire revenue cycle—from care planning to claim submission, denial management, and appeals.
Step 1: Determining Whether an NCD Applies
- Before providing or billing for a service, providers must determine:
- Whether an NCD exists for the procedure or diagnostic test.
- Whether the NCD fully governs coverage or allows for MAC-level interpretation in specific scenarios.
- Whether any LCD is relevant in the absence of a national policy.
- NCD lookup is typically conducted through:
- The Medicare Coverage Database (MCD)
- CMS transmittals and manual updates
- Compliance or RCM software integrated with NCD rulesets
- If an NCD exists, its provisions override all contractor-level policy.
Step 2: Applying National Coverage Criteria
- NCDs define the clinical indications and beneficiary eligibility required for Medicare coverage. Providers must ensure:
- The patient meets the covered indications.
- Excluded or investigational uses do not apply.
- Any prerequisite tests, conditions, or risk factors are documented before proceeding.
- Frequency limitations are respected.
- Clinical decision-making must align with these NCD requirements to avoid non-covered services or beneficiary liability issues.
Step 3: Aligning Documentation to NCD Standards
- NCDs specify precise documentation elements, which may include:
- Diagnostic findings
- Imaging, lab results, or clinical tests
- Symptoms, duration, or severity
- Conservative therapy attempted before advanced treatment
- Treatment rationale or specialty consultation notes
- Because NCDs are binding, documentation must match the clinical criteria exactly.
Step 4: Coding and Billing According to NCD Rules
- Billing teams rely on NCDs to correctly code and submit claims, including:
- Applicable CPT®/HCPCS codes
- Required ICD-10 diagnosis codes
- Mandatory modifiers
- Billing-specific rules (e.g., global periods, technical vs professional components)
- Device-specific coverage criteria (e.g., implantable devices)
- MACs use these coding criteria to ensure the claim is processed in accordance with national policy.
Step 5: Claim Submission and National Adjudication Consistency
Once submitted, MACs must evaluate claims directly against the NCD, ensuring uniform adjudication across all jurisdictions.
This eliminates regional variation and promotes predictable, standardized outcomes.
NCD-governed claims are:
- Less likely to be denied based on region-specific interpretation
- More predictable in terms of coverage and payment
- Subject to national consistency audits by CMS
Step 6: Handling NCD-Based Denials
- If an NCD requirement is not met, denials may be issued for:
- Non-covered indications
- Missing clinical documentation
- Unsupported diagnosis codes
- Exceeding frequency limits
- Billing for investigational or experimental use
- Providers may appeal NCD-based denials, but appeals must be rooted in:
- Clear alignment with NCD criteria
- New or overlooked evidence
- Corrections to coding or documentation
- Because NCDs are binding, appeals are typically evidence-driven, not interpretive.
Step 7: NCDs in Multi-State and National Provider Operations
- NCDs are essential for ensuring consistent workflows across large organizations, including:
- National health systems
- Multi-state specialty practices
- Telehealth providers
- DME suppliers
- Laboratory and diagnostic chains
- By providing nationwide criteria, NCDs allow providers to implement standardized protocols, reducing the administrative burden that accompanies LCD variation.
Step 8: NCDs in Audit, Compliance, and Program Integrity
- NCDs play a major role in federal audit programs:
- RACs use NCDs to validate coverage and medical necessity.
- TPE reviews reference NCD criteria when selecting claims.
- UPICs and OIG rely on NCDs for evaluating suspected fraud or abuse.
- CERT audits assess improper payment rates based on NCD alignment.
- Failure to adhere to NCD criteria is a leading cause of:
- Improper payments
- Audit findings
- Repeated medical record requests
- Prepayment claim holds
- For compliance teams, NCD familiarity is critical to minimizing risk and ensuring defensible billing.
NCDs in Billing, Reimbursement, and Compliance Limitations
National Coverage Determinations (NCDs) are the most authoritative Medicare coverage rules, shaping reimbursement accuracy, consistency, and predictability across every MAC jurisdiction.
When an NCD exists, it sets mandatory national guidelines for payment—defining medical necessity, documentation requirements, coding rules, and coverage limitations that all contractors must apply uniformly.
While NCDs eliminate regional variability and reduce adjudication inconsistencies, they can also introduce challenges, including slow update cycles, gaps in clinical relevance, and complexities when emerging technologies evolve faster than CMS can revise national policy.
How NCDs Influence Medicare Reimbursement
- Because NCDs are binding nationwide, they directly determine:
- Whether a service is covered, non-covered, or conditionally covered
- Which diagnoses support medical necessity
- What documentation must be present
- Which CPT®/HCPCS codes may be billed—and how
- How MACs adjudicate claims and conduct edits
- Whether claims undergo prepayment review
- NCD-governed services benefit from predictable, uniform reimbursement, reducing the administrative burden associated with regional LCD variation.
Advantages of National Consistency
- NCDs streamline reimbursement by:
- Eliminating regional differences in coverage
- Standardizing documentation expectations
- Ensuring the same service is covered similarly across all states
- Reducing variability in claims adjudication
- Simplifying billing for national and multi-state organizations
- This uniformity supports equitable access for beneficiaries regardless of geography.
Limitations in Update Frequency and Clinical Relevance
- One of the most significant limitations of NCDs is that they are often slow to update, sometimes lagging behind:
- Advances in diagnostics and imaging
- New medical devices
- Evolving specialty guidelines
- Precision medicine and genomics
- New evidence supporting efficacy or expanded indications
- As a result:
- Some NCDs become outdated relative to current practice.
- MACs may need to issue LCDs to fill gaps until CMS revises the NCD.
- Stakeholders may request NCD reconsideration, but the process is time-intensive.
- This delay can impact access to newer, evidence-supported services.
Coverage Restrictions and Non-Covered Indications
- NCDs frequently include:
- Explicit lists of non-covered uses
- Investigational or experimental designations
- Technology-specific limitations
- Prerequisite testing or clinical criteria
- Strict beneficiary eligibility rules
- These restrictions can result in:
- Higher denial rates
- Increased appeals activity
- Patient responsibility for non-covered services
- Provider confusion about coverage boundaries
- In certain specialties (e.g., cardiovascular, oncology, diagnostics), NCD exclusions strongly influence care planning and billing workflows.
Interactions With LCDs and Contractor-Level Policy
- While NCDs override LCDs, challenges arise when:
- An NCD is outdated and LCDs must interpret gaps
- Evidence evolves faster than national policy
- MACs take different approaches in clarifying gray areas
- Providers operate across regions with mixed NCD/LCD governance
- This creates operational complexity when NCDs do not fully account for clinical exceptions.
Administrative Burden and Appeal Complexity
- NCD-driven denials can be more difficult to overturn because:
- Contractors cannot deviate from national policy
- Appeal reviewers must apply the NCD as written
- Supporting medical literature cannot supersede binding language
- Exceptions are rarely granted under reconsideration processes
- Providers may face:
- Increased appeals workload
- Prolonged reimbursement delays
- Administrative friction when NCD criteria are narrowly defined
- This is particularly difficult when NCDs do not reflect current standard-of-care evidence.
Impact on Innovation and Technology Adoption
- NCDs tend to be conservative by design. This can:
- Slow adoption of new diagnostic technologies
- Delay coverage of novel therapeutic interventions
- Limit the use of molecular and genomic testing
- Restrict coverage for rapidly evolving digital health tools
- Manufacturers and specialty societies frequently petition CMS for:
- Expanded indications
- Revised criteria
- New national coverage pathways
- But NCD updates can take months—or years—to complete.
Key Takeaway
NCDs provide essential national consistency, ensuring Medicare beneficiaries receive equitable coverage regardless of geography and simplifying claims adjudication for providers.
However, their slow update cycle, narrow criteria, and rigid enforcement can create operational challenges and limit timely access to emerging medical innovations.
A balanced understanding of NCD authority—and how it interacts with LCDs—helps providers navigate billing accurately, minimize denials, and maintain compliance in a continually evolving clinical landscape.
How NCDs Influence Quality, Access, and Equity in Healthcare
National Coverage Determinations (NCDs) are among the most influential tools CMS uses to promote consistent, evidence-based, and equitable coverage across the United States.
By establishing uniform rules for when services are considered reasonable and necessary, NCDs help ensure that Medicare beneficiaries receive care based on clinical evidence rather than geography, contractor interpretation, or local practice variation.
NCDs support quality and equity by setting nationwide standards—but they can also create challenges when slow update cycles lag behind clinical innovation or when the national criteria are more restrictive than modern practice.
Promoting Nationwide Consistency and Quality Standards
- NCDs provide uniform coverage criteria that all MACs must follow.
- This ensures that key services—imaging, diagnostics, preventive care, and medical devices—are covered consistently across all regions.
- National alignment supports:
- Predictable access for beneficiaries
- Standardized quality expectations
- Consistent provider workflows across states
- Because NCDs rely on evidence-based medicine, they reinforce clinical appropriateness and reduce the likelihood of low-value or unnecessary care.
- NCDs therefore function as a stabilizing force in Medicare’s coverage ecosystem.
Reducing Geographic Disparities and Contractor Variability
- Without NCDs, coverage decisions default to LCDs, which may vary regionally.
- NCDs minimize this variation by:
- Eliminating differences in MAC interpretation
- Ensuring equal access to essential services
- Reducing regional discrepancies in denial rates
- Preventing inconsistent adoption of new medical technologies
- Uniform policy is especially important for:
- Rural beneficiaries
- Multi-state provider networks
- National diagnostic laboratories
- Telehealth and virtual care providers
- NCDs help ensure that geography is not a barrier to covered care.
Transparency Through Public Evidence Evaluation
- CMS develops NCDs through a structured public and scientific review process that includes:
- Publication of clinical evidence summaries
- MEDCAC (Medicare Evidence Development & Coverage Advisory Committee) deliberations
- Public comment opportunities
- Stakeholder engagement, including specialty societies and manufacturers
- This transparent approach:
- Builds provider trust
- Allows specialists to influence national policy
- Ensures coverage decisions are grounded in peer-reviewed evidence
- Makes the Medicare coverage process more predictable and accountable
- Transparency strengthens both the scientific integrity and perceived fairness of NCDs.
Challenges in Innovation and Timely Access
- NCDs are comprehensive but slow to update, often trailing advances in:
- Precision medicine
- Molecular diagnostics
- Imaging technologies
- Implantable devices
- Digital health and remote patient monitoring
- AI-enabled diagnostics
- Slow revision cycles can create:
- Coverage gaps for emerging technologies
- Barriers to timely patient access
- Administrative workarounds until CMS updates national policy
- Increased reliance on LCDs or local contractor discretion
- As a result, beneficiaries may temporarily face restricted access to innovations supported by strong but recent evidence.
Equity Implications for Underserved Populations
- NCDs can support or challenge health equity depending on their scope:
- When broad and inclusive, they ensure consistent access for all beneficiaries—including those in underserved or rural settings.
- When narrowly defined or outdated, they may unintentionally limit coverage for populations with:
- Lower access to specialty providers
- Higher disease prevalence
- Delayed diagnosis or barriers to documentation
- Limited access to prerequisite testing required by national policy
- CMS increasingly reviews NCDs through an equity lens, assessing whether coverage criteria inadvertently create barriers for vulnerable populations.
Impact on Quality Measurement and Value-Based Care
- NCDs also influence quality initiatives because they:
- Shape which services and screening tests are covered nationwide
- Enable uniform quality measurement across states
- Support consistent adoption of preventive and diagnostic services
- Provide a national foundation for value-based care models
- By defining when a service is medically necessary, NCDs indirectly structure how providers measure, deliver, and improve outcomes.
Key Insight
NCDs are essential to promoting nationwide consistency, transparency, and equitable access to evidence-based care.
However, the balance between stability and innovation is delicate—slow updates can create temporary inequities, and overly narrow criteria may not fully reflect current clinical best practices.
A modernized, agile NCD framework is critical to ensuring timely, fair, and clinically aligned coverage for all Medicare beneficiaries.
Frequently Asked Questions about National Coverage Determinations (NCDs)
1. What is a National Coverage Determination (NCD)?
A National Coverage Determination (NCD) is a binding Medicare policy issued by CMS that defines whether a medical service, procedure, device, or diagnostic test is considered reasonable and necessary nationwide.
NCDs override all Local Coverage Determinations (LCDs) and must be followed by every Medicare Administrative Contractor (MAC) across all states and territories.
2. How do NCDs differ from LCDs?
The key differences are:
- NCDs apply nationally and are issued by CMS Central Office.
- LCDs apply regionally and are issued by MACs.
- When both exist, the NCD governs and overrides any conflicting LCD language.
- NCDs are updated less frequently but provide consistent national coverage standards.
3. How do I find out if an NCD applies to a service?
You can locate NCDs in the:
- CMS Medicare Coverage Database (MCD)
- CMS transmittals and Medicare manuals
- Compliance or EHR-integrated coverage tools
Always verify whether an NCD is active, retired, or superseded, as some NCDs have been replaced by updated national guidance.
4. What happens if a claim does not meet NCD criteria?
Claims may be denied for:
- Missing or unsupported diagnosis codes
- Failure to meet medical necessity criteria
- Lack of required documentation
- Non-covered or investigational indications
- Exceeding frequency limitations
Because NCDs are binding, appeal reviewers must apply the NCD as written, making NCD-based denials more difficult to overturn than LCD-based denials.
5. How often are NCDs updated?
NCDs are updated infrequently—some remain unchanged for years.
Updates occur when:
- New clinical evidence emerges
- FDA approvals or labeling changes occur
- Stakeholders request reconsideration
- CMS identifies inconsistencies or outdated criteria
This slow update cycle is a major reason why LCDs continue to fill coverage gaps at the regional level.
6. Can an NCD be appealed or reconsidered?
Providers cannot appeal the content of an NCD through the traditional claims appeals process.
However:
- Providers and stakeholders may request reconsideration by submitting clinical evidence to CMS.
- CMS may revise, expand, or retire an NCD through its structured public process.
- Claims denied under an NCD may be appealed only on the basis of documentation errors, not disagreement with national policy.
7. How do NCDs affect audits and program integrity?
NCDs are used extensively during federal oversight reviews:
- RACs apply NCD criteria when identifying improper payments.
- TPE reviews use NCD language for documenting medical necessity.
- UPIC and OIG investigations rely on NCDs to detect aberrant or non-covered billing.
- CERT audits measure national payment accuracy based on NCD alignment.
Failure to comply with NCD requirements is a common source of prepayment review, recoupments, and audit findings.
