What is an RHC (Rural Health Clinic) in Healthcare?
A Rural Health Clinic (RHC) is a federally certified healthcare facility established to improve access to primary care services in rural and underserved communities. Created under the Rural Health Clinic Services Act of 1977, the RHC program is administered by the Centers for Medicare & Medicaid Services (CMS) and designed to expand availability of outpatient, preventive, and basic laboratory services in areas facing provider shortages.
RHCs can be either independent (standalone facilities) or provider-based (operated by a hospital, nursing home, or other health system). They deliver services primarily through nurse practitioners (NPs), physician assistants (PAs), and certified nurse midwives (CNMs) working alongside physicians. To qualify for certification, an RHC must be located in a CMS-designated rural area experiencing a shortage of healthcare professionals.
From a billing and reimbursement perspective, RHCs operate under a cost-based payment model, rather than the traditional Medicare Physician Fee Schedule (MPFS). This ensures fair compensation for providers serving rural populations, where patient volume is often lower and operational costs are higher.
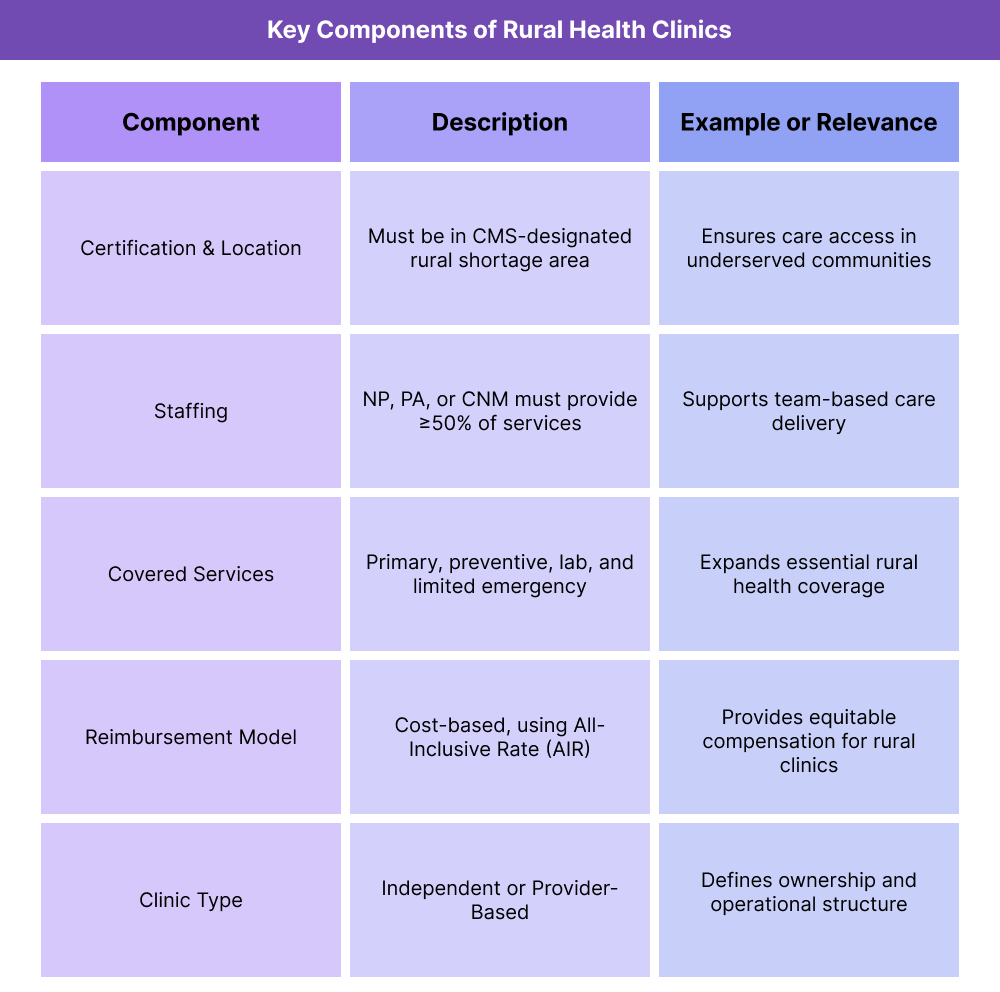
Key Components of a Rural Health Clinic (RHC)
The Rural Health Clinic (RHC) model was created to ensure that residents in rural or medically underserved areas have access to consistent, high-quality primary care. To qualify for certification and reimbursement, an RHC must meet specific CMS-defined operational, staffing, and service delivery requirements.
1. Certification and Location Requirements
- RHCs must be located in a CMS-designated rural area and in a Health Professional Shortage Area (HPSA), Medically Underserved Area (MUA), or Governor-designated shortage area.
- Facilities are certified through a survey process administered by the state agency and CMS regional offices.
- RHCs must comply with federal Conditions for Certification, including patient care standards, physical accessibility, and infection control policies.
2. Provider Staffing Requirements
- RHCs must employ at least one nurse practitioner (NP), physician assistant (PA), or certified nurse midwife (CNM) who provides services at least 50% of the time the clinic operates.
- Services may be supervised by a physician, but direct on-site supervision is not always required.
- This team-based model expands capacity while maintaining flexibility in rural staffing structures.
3. Covered Services
- Core services include primary and preventive care, diagnostic and laboratory testing, and basic emergency services.
- Additional covered services often include behavioral health, chronic care management, and telehealth when compliant with CMS regulations.
- RHCs may also provide visiting nurse services in certain shortage areas.
4. Reimbursement Methodology
- Unlike standard Medicare billing, RHCs are reimbursed under a cost-based payment system that reflects their actual operating costs.
- Each RHC is assigned an All-Inclusive Rate (AIR) per patient visit, capped annually by CMS (adjusted for inflation).
- The AIR includes both professional and facility components and is reconciled through the annual Medicare Cost Report process.
5. Types of RHCs
- Independent RHCs: Standalone clinics not affiliated with hospitals.
- Provider-Based RHCs: Owned and operated by a hospital or integrated health system, often within 50 beds or fewer.
How Rural Health Clinics (RHCs) Operate in Practice
Rural Health Clinics (RHCs) provide comprehensive primary and preventive care to underserved rural communities through a team-based, cost-based reimbursement model. Their operational workflows blend traditional patient care with unique reporting and billing requirements that reflect their federally certified status.
The following steps outline how an RHC functions from patient encounter through reimbursement and compliance.
Step 1: Patient Encounter and Service Delivery
- Patients receive care from a qualified provider — typically a nurse practitioner (NP), physician assistant (PA), certified nurse midwife (CNM), or physician.
- Services may include acute visits, preventive care, chronic disease management, or behavioral health interventions.
- RHCs often integrate telehealth and care coordination programs to extend reach to remote populations.
Step 2: Documentation and Coding
- Providers document encounters in the electronic health record (EHR) following CMS and payer requirements.
- Services are assigned CPT or HCPCS codes for tracking, though RHCs do not bill individual codes to Medicare Part B in the same way as standard physician practices.
- Instead, these codes are used to support the encounter-level claim that determines the All-Inclusive Rate (AIR) payment.
Step 3: Claim Submission and Reimbursement
- Each patient visit is billed as an encounter claim under the RHC’s Type of Bill 71X, with the AIR applied per qualifying visit.
- Additional reimbursable services, such as telehealth or chronic care management, may be billed separately using designated HCPCS codes if covered by the payer.
- Medicare reimburses up to the annual AIR cap, while Medicaid and commercial payers may use different rate methodologies.
Step 4: Cost Reporting and Reconciliation
- RHCs must file an annual Medicare Cost Report (Form CMS-222-17) to reconcile interim payments with actual operating costs.
- The report includes staffing expenses, facility overhead, and service utilization data.
- Adjustments to the AIR are made based on this cost reporting, ensuring reimbursement aligns with the clinic’s real-world resource use.
Step 5: Compliance and Quality Reporting
- RHCs participate in CMS quality reporting programs, which may include preventive service benchmarks and outcome metrics.
- Compliance with Conditions for Certification and periodic surveys is required to maintain active RHC status.
- Many clinics integrate RHC participation into broader value-based initiatives, leveraging data for population health analytics and grant opportunities.
RHC Billing, Reimbursement, and Program Limitations
Rural Health Clinics (RHCs) operate under a cost-based reimbursement system that is fundamentally different from standard physician billing. This model is intended to ensure financial sustainability for providers serving rural and underserved populations, but it comes with strict compliance and reporting rules that affect how claims are submitted and reimbursed.
Cost-Based Reimbursement Methodology
- RHCs receive payment based on their All-Inclusive Rate (AIR), which reflects the average cost of providing one qualifying patient encounter.
- The AIR covers both professional and facility components for Medicare Part B services.
- CMS establishes an annual payment limit (cap) for AIR reimbursement; as of 2025, the cap continues to adjust for inflation under the Medicare Economic Index (MEI).
- The AIR is determined during certification and recalculated annually through the Medicare Cost Report process (Form CMS-222-17).
Claim Submission and Billing Process
- Each qualifying patient visit is billed as a single encounter, regardless of the number of procedures or diagnoses documented.
- RHCs submit claims under Type of Bill 71X using Revenue Code 0521 for general medical visits and other 052X subcodes for specialized services.
- Additional services, such as telehealth, behavioral health integration, or care management, may be billed separately if covered and supported by documentation.
- RHCs cannot bill individual CPT line items to Medicare for professional services — they must be rolled into the encounter-based AIR structure.
Payment Adjustments and Cost Reporting
- Interim payments are made throughout the year based on expected utilization.
- At year-end, the RHC’s Medicare Administrative Contractor (MAC) performs a reconciliation against the Cost Report to ensure the clinic is reimbursed correctly.
- Overpayments or underpayments are adjusted accordingly.
Program Limitations and Challenges
- Annual AIR Cap: Limits total reimbursement potential and may not reflect the true cost of care for high-complexity populations.
- Service Exclusions: Certain services, such as technical-only lab tests or DME (durable medical equipment), are not included under the RHC benefit.
- Documentation Burden: RHCs must maintain precise cost accounting and encounter-level documentation to support CMS audits.
- Administrative Complexity: Managing dual billing streams (RHC encounter claims vs. ancillary services billed separately) can be resource-intensive.
- Rural Workforce Constraints: Recruiting and retaining NPs, PAs, and CNMs in rural regions remains a significant operational challenge.
RHC and Its Impact on Quality, Access, and Health Equity
Rural Health Clinics (RHCs) play a critical role in advancing health equity, access, and quality of care for populations living in rural and underserved regions. By linking cost-based reimbursement with local provider engagement, the RHC model helps sustain primary and preventive services where they might otherwise be unavailable.
Expanding Access to Primary and Preventive Care
- RHCs were designed to reduce geographic and economic barriers to healthcare by ensuring stable, community-based service delivery.
- They provide essential primary, preventive, and urgent care to rural patients who may live hours away from the nearest hospital.
- Cost-based reimbursement ensures that even low-volume or geographically isolated clinics can remain financially viable while meeting community needs.
Strengthening the Rural Healthcare Workforce
- The RHC staffing model encourages the integration of nurse practitioners (NPs), physician assistants (PAs), and certified nurse midwives (CNMs) to extend physician capacity.
- This team-based structure promotes flexible scheduling and interdisciplinary collaboration, particularly in areas facing acute provider shortages.
- RHCs often serve as training and retention hubs for rural clinicians, offering exposure to full-scope primary care and community health.
Improving Quality and Continuity of Care
- RHC participation in CMS quality programs promotes data-driven care improvement, focusing on preventive services, chronic disease management, and patient outcomes.
- Many RHCs integrate telehealth and care coordination programs to connect patients to specialty care while maintaining local oversight.
- By standardizing encounter documentation and cost reporting, RHCs contribute to greater transparency and accountability in rural health delivery.
Advancing Health Equity and Population Health Goals
- RHCs disproportionately serve older adults, Medicaid recipients, and low-income populations — groups that often experience the greatest barriers to care.
- By providing affordable access points, RHCs help reduce preventable hospitalizations and emergency department use in rural regions.
- Federal and state grants often fund SDOH initiatives and preventive outreach within RHCs, further aligning them with CMS’s health equity framework.
Challenges to Long-Term Equity
- Despite their mission, many RHCs face financial strain from capped reimbursement rates, limited payer participation, and rising operational costs.
- Broadband and infrastructure limitations hinder expansion of telehealth and data exchange.
- Addressing these barriers through policy reform and workforce investment is essential to preserving RHC impact across rural America.
Frequently Asked Questions about RHCs
1. What is an RHC in healthcare?
An RHC (Rural Health Clinic) is a federally certified healthcare facility that provides primary and preventive care in rural or medically underserved areas. RHCs receive cost-based reimbursement from Medicare to ensure access and financial stability for providers serving rural populations.
2. Who qualifies to operate as an RHC?
To qualify, a clinic must be located in a CMS-designated rural area and within a Health Professional Shortage Area (HPSA), Medically Underserved Area (MUA), or a Governor-designated shortage area. The clinic must also meet CMS Conditions for Certification related to staffing, services, and patient care standards.
3. What types of providers can work in an RHC?
RHCs must employ at least one nurse practitioner (NP), physician assistant (PA), or certified nurse midwife (CNM) who provides services at least 50% of the clinic’s operating hours. Physicians, behavioral health specialists, and other licensed clinicians may also participate as part of the care team.
4. How are RHCs reimbursed?
RHCs are reimbursed through a cost-based payment model using the All-Inclusive Rate (AIR), which represents the average cost of one qualifying encounter. The AIR is subject to an annual CMS cap and reconciled through the Medicare Cost Report process each year.
5. What services are covered under RHC reimbursement?
Covered services include primary and preventive care, laboratory testing, and basic emergency services, as well as certain mental health, chronic care management, and telehealth visits if compliant with CMS rules. Technical services (like lab-only tests) and durable medical equipment (DME) are typically excluded.
6. What is the difference between an RHC and an FQHC?
- RHC (Rural Health Clinic): Located in rural shortage areas; reimbursed under cost-based AIR model.
- FQHC (Federally Qualified Health Center): May operate in urban or rural underserved areas; receives prospective payment system (PPS) reimbursement and qualifies for additional federal grants.
Both aim to expand access, but they differ in funding mechanisms, scope, and regulatory oversight.
7. What are the main challenges for RHCs today?
RHCs face challenges including workforce shortages, capped reimbursement rates, and administrative complexity related to cost reporting. Many are also navigating the transition to hybrid models that integrate telehealth, behavioral health, and Value-Based Care while maintaining compliance with federal regulations.
