CPT 98010 Description, Billing Rules, & Use Cases
CPT 98010 is used to bill for a synchronous audio-only evaluation and management (E/M) visit with a new patient that involves moderate medical decision making (MDM) or at least 45 minutes of total provider time on the date of the encounter.
This code is part of the 2025 audio-only telemedicine E/M series (98008–98011), introduced to replace the deleted telephone codes (99441–99443). CPT 98010 applies to encounters that require more in-depth assessment and discussion than CPT 98009, including evaluation of multiple symptoms or conditions that require moderate complexity decision making.
The visit typically includes:
- Conducting a detailed medical and medication history through audio-only communication
- Managing multiple or unstable chronic conditions or a new, moderate-severity issue
- Reviewing lab results, specialist notes, or imaging with the patient
- Adjusting treatment plans or medications
- Providing in-depth education and counseling on management or risk reduction
- Documenting all clinical findings and care coordination efforts
Billing Notes:
- Applies only to audio-only telehealth (no video component).
- Requires moderate MDM or at least 45 minutes of provider time.
- Must involve real-time verbal interaction between the provider and patient.
- May not be billed on the same day as an in-person or video E/M encounter.
- The provider must document patient consent, communication method, and total time or MDM level supporting the service.
What is CPT Code 98010?
CPT 98010 is an evaluation and management (E/M) code for audio-only telemedicine visits with new patients that require moderate medical decision making (MDM) or 45–59 minutes of total provider time on the date of the encounter.
Introduced in 2025, CPT 98010 is part of the new audio-only E/M range (98008–98011) for new-patient encounters. These codes allow providers to bill legitimate telehealth visits conducted entirely by phone or other real-time audio technology when a video connection is unavailable, clinically unnecessary, or inaccessible for the patient.
Key points about CPT 98010:
- Used for moderate-complexity new-patient visits via audio-only communication.
- The provider must spend a minimum of 45 minutes performing and documenting the encounter.
- Requires real-time, synchronous communication — not prerecorded messages or asynchronous exchanges.
- May include discussion of multiple conditions, medication management, and coordination of diagnostic workups.
- The service must meet all telehealth documentation and consent standards.
- Cannot be billed on the same day as an in-person or audio-video E/M service.
In summary: CPT 98010 applies to audio-only telehealth visits with new patients that involve moderate complexity decision making or 45–59 minutes of total provider time, bridging the gap between shorter low-complexity encounters (98009) and high-complexity visits (98011).
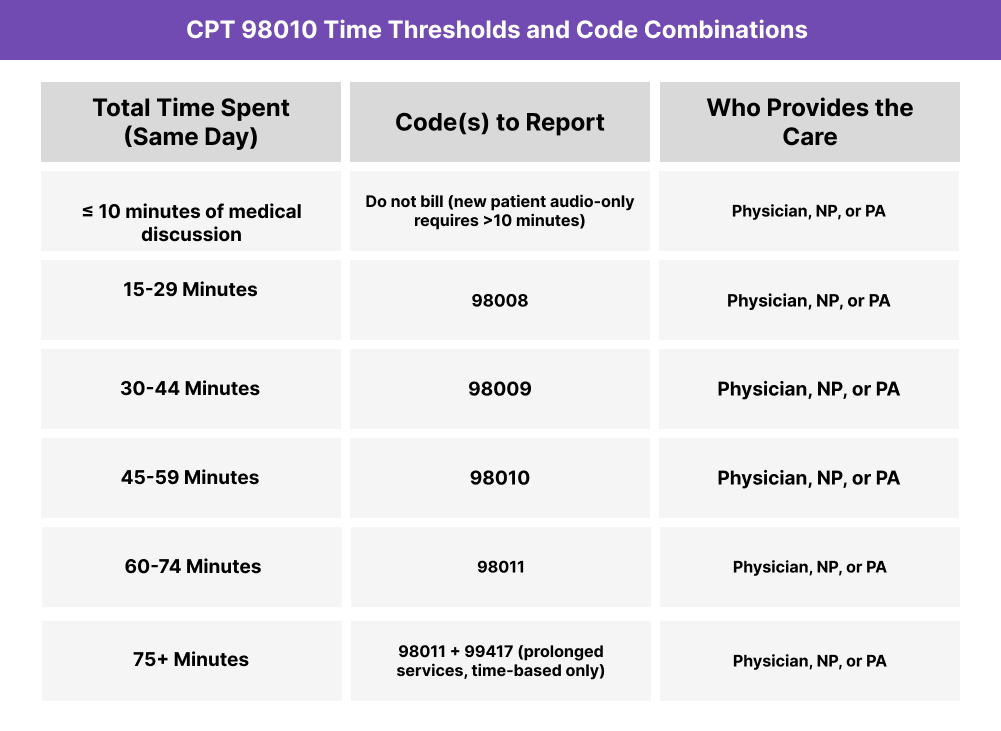
CPT 98010 Time Thresholds and Code Combinations
CPT 98010 represents a synchronous audio-only evaluation and management (E/M) service for a new patient that requires moderate medical decision making (MDM) or at least 45 minutes of total provider time on the date of the encounter.
Understanding the Time Component
When coding by time, a minimum of 45 minutes must be spent by the billing provider in real-time audio communication and related care activities performed on the same date. Time includes:
- Reviewing relevant medical history, results, and prior documentation
- Conducting an in-depth clinical discussion with the patient
- Providing counseling, education, or medication management
- Coordinating care with other professionals (if applicable)
- Documenting the visit, care plan, and follow-up arrangements
If total time exceeds 59 minutes, the next code (CPT 98011) should be reported. Encounters shorter than 45 minutes may qualify for CPT 98009 (30–44 minutes).
Understanding the MDM Component
When selecting by medical decision making, documentation must reflect moderate complexity:
- Problems: One or more chronic conditions with exacerbation, or new problems requiring diagnostic workup.
- Data: Moderate amount and/or complexity of data reviewed or ordered.
- Risk: Moderate risk of morbidity, mortality, or treatment side effects.
When to Use CPT 98010: Common Scenarios and Use Cases
CPT 98010 is appropriate when a physician, nurse practitioner (NP), or physician assistant (PA) provides a synchronous audio-only evaluation and management (E/M) visit with a new patient that involves moderate-complexity medical decision making (MDM) or 45–59 minutes of total provider time.
Here are examples of how CPT 98010 is used in practice:
CPT 98010 Billing Requirements and Eligibility
CPT 98010 is used to report a synchronous audio-only telehealth evaluation and management (E/M) service with a new patient that involves moderate medical decision making (MDM) or at least 45 minutes of total provider time.
This code reflects a higher level of complexity and duration than CPT 98009 and applies when the provider must evaluate multiple conditions, interpret data, or make treatment decisions that carry moderate clinical risk.
Patient Eligibility
The encounter must meet the following criteria:
- The patient is a new patient (has not received professional services from the same provider or group within the past three years).
- The visit was conducted via audio-only communication, in real time.
- The patient provided consent to receive telehealth care using audio-only technology.
- The condition addressed required moderate-complexity medical decision making or a minimum of 45 minutes of provider time.
- The service was not performed on the same day as an in-person or video-based E/M visit.
Provider Eligibility
The service must be personally performed by:
- A physician, nurse practitioner (NP), or physician assistant (PA) qualified to report E/M services.
- The billing provider must personally conduct the encounter and cannot delegate discussion or decision-making portions to staff.
- Providers must document the mode of communication, time spent, and MDM complexity in the record.
Service Requirements
- The provider must spend at least 45 minutes on the same day of service, including pre-visit review, clinical discussion, and documentation.
- Only provider time counts — exclude administrative, scheduling, or setup time.
- The visit may be selected based on MDM or time, but documentation must support the higher of the two.
- The encounter must involve meaningful medical evaluation and decision making, not administrative communication.
- Follow-up care should be planned and documented (telehealth, in-person, or referral).
Documentation Requirements
- Record start and end time, or total provider time (≥45 minutes).
- Note patient consent and specify the audio-only communication method.
- Include a clear reason for the visit and clinical justification for telehealth format.
- Document moderate-complexity MDM or time-based justification.
- Ensure the encounter includes a clinical assessment, plan, and next steps.
- Include a provider attestation confirming personal performance and documentation accuracy.
Medicare and Payer Coverage Notes
- Medicare: CPT 98010 currently has a status indicator “I” (invalid for Medicare billing).
- Commercial payers: Many may adopt CPT 98010 for reimbursement following RBRVS valuation.
- Verify payer-specific telehealth policies, as coverage for audio-only services varies by state and carrier.
CPT 98010 Billing Documentation Checklist
To support compliant billing for CPT 98010, documentation must demonstrate that the visit was a real-time, audio-only telehealth encounter with a new patient, requiring moderate-complexity MDM or at least 45 minutes of total provider time.
Your encounter record should include:
- Patient consent for telehealth services, including acknowledgment that the visit was audio-only (no video).
- Verification of patient identity at the beginning of the call.
- Reason for the visit or presenting problem (chief complaint).
- Provider credentials and role (physician, NP, or PA).
- Communication method clearly stated as “synchronous audio-only.”
- Total provider time documented (minimum 45 minutes) with either:
- Start and end times, or
- Total duration on the date of the encounter.
- Moderate-complexity MDM clearly shown, including:
- Problems: Multiple conditions or new problem requiring workup.
- Data: Moderate amount or complexity of tests, labs, or external notes reviewed.
- Risk: Moderate risk of complications or morbidity from management decisions.
- Summary of the medical discussion, including:
- History obtained via audio communication.
- Assessment and treatment plan discussed.
- Education or counseling provided to the patient.
- Follow-up plan, including timing and format (telehealth, in-person, or specialist referral).
- Provider attestation confirming the encounter was performed personally and documentation is complete.
- Statement of modality noting that the service was audio-only, not audiovisual.
- Non-duplication statement verifying no same-day in-person or video E/M service was reported.
Common CPT 98010 Billing Mistakes (and How to Avoid Them)
❌ Billing Without 45 Minutes of Documented Time
When coding by time, providers must record at least 45 minutes of total provider time on the date of the encounter. Calls that last less than 45 minutes should be billed under CPT 98009.
❌ Missing Moderate-Complexity MDM Details
If coding by MDM, documentation must clearly demonstrate moderate complexity — multiple problems or a new condition requiring diagnostic evaluation, moderate data review, and moderate clinical risk.
❌ Failing to Specify Audio-Only Communication
Every note must explicitly state that the encounter was synchronous audio-only (no video). Payers often deny or downcode claims that omit this clarification.
❌ Using CPT 98010 for Established Patients
This code applies only to new patient encounters. Established patient audio-only visits should use CPT 98014 or the appropriate code from 98012–98015.
❌ Counting Non-Billable or Administrative Time
Only provider-performed, medically necessary activities on the date of service count toward the time threshold. Exclude scheduling, connection setup, and post-visit documentation done later.
❌ Omitting Consent or Identity Verification
Patient consent and identity verification must be clearly recorded before clinical discussion begins.
❌ Reporting Alongside Other Same-Day E/M Services
Audio-only telehealth encounters billed under CPT 98010 cannot be reported with in-person or audio-video E/M services on the same day.
❌ Inadequate Clinical Documentation
Ensure the record includes a clear reason for the visit, assessment, plan, and follow-up, as well as justification for telehealth format. Missing these elements can lead to denials.


