CPT 99214 Description, Billing Rules, & Use Cases
CPT 99214 is used to bill for an office or other outpatient visit with an established patient that requires moderate level medical decision making (MDM) and/or at least 30 minutes of total provider time on the date of the encounter.
This code represents a moderate-complexity E/M visit, typically involving multiple chronic conditions, prescription management, or diagnostic data review that requires more provider involvement than CPT 99213.
The visit may include:
- Reviewing detailed medical and medication history
- Performing a focused but expanded physical examination
- Managing one or more moderate-complexity problems
- Adjusting medications or ordering diagnostic testing
- Counseling the patient or caregiver on treatment plans or risk reduction
- Coordinating care with other providers or specialists
- Documenting findings, assessment, and plan in the medical record
What is CPT Code 99214?
CPT 99214 is an evaluation and management (E/M) code used for established patient office or outpatient visits that require moderate level medical decision making (MDM) or at least 30 minutes of total provider time on the date of the encounter.
Key points about CPT 99214:
- It applies to visits that involve multiple chronic conditions or an acute illness with systemic symptoms requiring management or coordination of care.
- The provider must personally perform the service — 99214 cannot be billed for staff-only visits.
- The 2024 E/M guidelines require documentation that 30 minutes or more were spent if coding by time.
- Moderate-complexity MDM includes review of multiple data elements (e.g., test results, external notes) and moderate risk due to treatment decisions or medication management.
- If total time is less than 30 minutes, or the visit only involves low-complexity MDM, 99213 should be used instead.
In summary: CPT 99214 represents a moderate-complexity visit where the provider performs an expanded evaluation, manages ongoing care, and documents at least 30 minutes or equivalent MDM complexity.
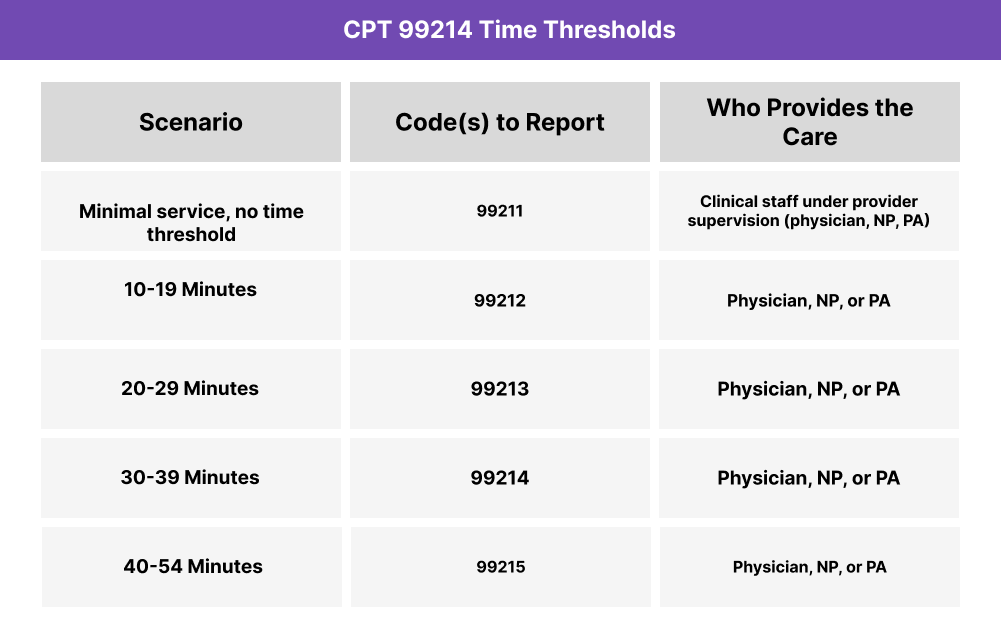
CPT 99214 Time Thresholds and Code Combinations
CPT 99214 is used when an established patient office or outpatient visit requires moderate-complexity medical decision making (MDM) or at least 30 minutes of total provider time on the date of the encounter. This code is often chosen for visits that demand significant provider involvement, such as managing multiple medications, reviewing extensive diagnostic data, or coordinating care for complex but stable conditions.
Understanding the Time Component
When coding based on time, the provider must document a minimum of 30 minutes spent on the encounter. This includes both face-to-face and non–face-to-face activities on the same date of service, such as:
- Reviewing test results, imaging, or external records
- Conducting a detailed history and exam
- Counseling the patient or family about condition management
- Ordering, reviewing, or interpreting diagnostic studies
- Updating care plans and documenting in the EHR
- Coordinating care with other specialists or facilities
If the visit exceeds 54 minutes, you should consider reporting CPT 99215 instead. For shorter encounters (20–29 minutes), use CPT 99213.
Understanding the MDM Component
Moderate-complexity MDM under CPT 99214 generally involves:
- Problems: One or more chronic illnesses with exacerbation or two or more stable chronic conditions
- Data: Review or ordering of multiple tests, external notes, or independent interpretation
- Risk: Moderate risk of morbidity or treatment side effects (e.g., prescription drug management, diagnostic procedures, or escalation of care)
These parameters distinguish 99214 from lower-level codes (which involve simpler problems or limited data) and from 99215 (which represents high-complexity care).
When to Use CPT 99214: Common Scenarios and Use Cases
CPT 99214 is appropriate when a physician, nurse practitioner (NP), or physician assistant (PA) provides an established patient visit that involves moderate-complexity medical decision making (MDM) or at least 30 minutes of total provider time. These visits often include chronic disease management, medication adjustments, or coordination of care across specialties.
Here are examples of how CPT 99214 is used in practice:
CPT 99214 Billing Requirements and Eligibility
To bill CPT 99214, the encounter must reflect either moderate-complexity medical decision making (MDM) or at least 30 minutes of total provider time on the date of service.
Patient Eligibility
- The patient must be an established patient (seen by the same group within the past three years).
- The encounter should address moderate-complexity issues, such as:
- Two or more stable chronic conditions
- One or more chronic illnesses with exacerbation, progression, or side effects of treatment
- A new problem with uncertain prognosis that requires ongoing management
Provider Eligibility
- The service must be personally performed by a physician, nurse practitioner (NP), or physician assistant (PA).
- Clinical staff may assist (e.g., recording vitals or history), but provider evaluation and management must occur.
- The billing provider is responsible for documenting both time and medical complexity if applicable.
Service Requirements
Time-based billing:
- At least 30 minutes of total provider time on the date of the encounter
- Includes all qualifying activities such as chart review, history/exam, ordering/interpreting tests, counseling, documentation, and coordination of care
MDM-based billing:
- Must meet moderate-complexity MDM, defined by:
- Problems: multiple chronic or complex issues
- Data: moderate amount of data reviewed, ordered, or analyzed
- Risk: moderate risk of morbidity, mortality, or treatment side effects
- If total time is 20–29 minutes, bill 99213 instead.
- If the encounter exceeds 54 minutes or involves high-complexity MDM, bill 99215.
Code Comparison
- 99213 vs 99214: 99213 = 20–29 minutes or low MDM; 99214 = 30–39 minutes or moderate MDM.
- 99214 vs 99215: 99215 applies to visits of 40–54 minutes or high-complexity MDM, often requiring intensive data review or decision making.
CPT 99214 Billing Documentation Checklist
To support compliant billing for CPT 99214, documentation should include:
- Established patient status confirmed (seen by the practice within the past three years).
- Reason for the encounter documented (e.g., management of multiple chronic conditions, medication adjustment, or moderate-severity acute issue).
- Provider involvement clearly stated — service must be performed by a physician, NP, or PA.
- Time documentation (if coding by time):
- At least 30 minutes of total provider time on the date of service
- Record specific time spent and qualifying activities (exam, review of results, patient counseling, documentation, coordination of care)
- Medical decision making (if coding by MDM):
- Problems: One or more chronic illnesses with exacerbation, or two or more stable chronic conditions
- Data: Review or ordering of multiple tests, notes, or independent interpretations
- Risk: Moderate risk of morbidity or treatment side effects (e.g., prescription drug management)
- Exam and history findings supporting the MDM level or time spent.
- Patient counseling and education documented when provided.
- Provider attestation confirming personal performance and accuracy of documentation.
- Non-overlap statement confirming time and services are distinct from any other codes billed that day.
Common CPT 99214 Billing Mistakes (and How to Avoid Them)
❌ Billing Without 30 Minutes of Documented Time
When coding by time, at least 30 minutes must be clearly documented. Encounters under this threshold should be billed as 99213.
❌ Under-Documenting Moderate MDM
If coding by MDM, notes must demonstrate moderate complexity — multiple problems, review of multiple data elements, and moderate risk due to medication or management decisions.
❌ Confusing 99213 With 99214
Many providers default to 99214 for routine visits that only qualify as 99213. Documentation must justify either the time or MDM required for moderate complexity.
❌ Overlooking Time Outside the Encounter
Only time spent on the date of the encounter counts. Pre-visit prep or post-visit documentation done on another date cannot be included.
❌ Missing Prescription Drug Management
Moderate-complexity MDM often includes medication management. If this occurs, it must be clearly stated to justify the risk level.
❌ Using 99214 in the Wrong Setting
This code is valid only for office or outpatient visits. For hospital, observation, or ED visits, use the corresponding inpatient E/M codes.



