CPT 99417 Description, Billing Rules, & Use Cases
CPT 99417 is an add-on code used to bill for prolonged outpatient evaluation and management (E/M) services when the provider spends additional time beyond the required threshold of the highest-level primary service. It is reported in 15-minute increments and can only be billed in conjunction with specific primary E/M codes, such as 99205 (new patient) or 99215 (established patient)
This code applies when a physician, nurse practitioner (NP), or physician assistant (PA) provides extra time-intensive care in an office, outpatient, or telehealth setting that extends beyond the usual maximum service time of the base code.
- Examples of activities that may qualify for prolonged service billing under CPT 99417 include:
- Extensive review and interpretation of diagnostic data
- Extended patient or caregiver counseling sessions
- Complex care coordination involving multiple specialists
- Documentation and communication that go beyond the typical scope of a standard encounter
What is CPT Code 99417?
CPT 99417 is an evaluation and management (E/M) add-on code that represents prolonged outpatient services provided by a physician, nurse practitioner (NP), or physician assistant (PA). It is billed when the encounter time extends at least 15 minutes beyond the required threshold for the highest-level primary E/M code
Key points:
- CPT 99417 is not reported on its own — it must be billed in addition to a primary E/M code such as 99205 (new patient) or 99215 (established patient).
- Each unit of 99417 corresponds to an additional 15 minutes of total time spent on the encounter.
- Time may include both face-to-face and non–face-to-face activities performed on the date of the encounter, such as chart review, counseling, coordinating care, and documentation.
- Encounters must meet or exceed the base time threshold of the highest-level E/M code before 99417 can be added.
- For new patients, billing begins once total time reaches 75 minutes (60 min base for 99205 + 15 min).
- For established patients, billing begins once total time reaches 55 minutes (40 min base for 99215 + 15 min).
In short, CPT 99417 allows providers to receive reimbursement for time-intensive outpatient visits that exceed the typical duration of standard E/M codes.
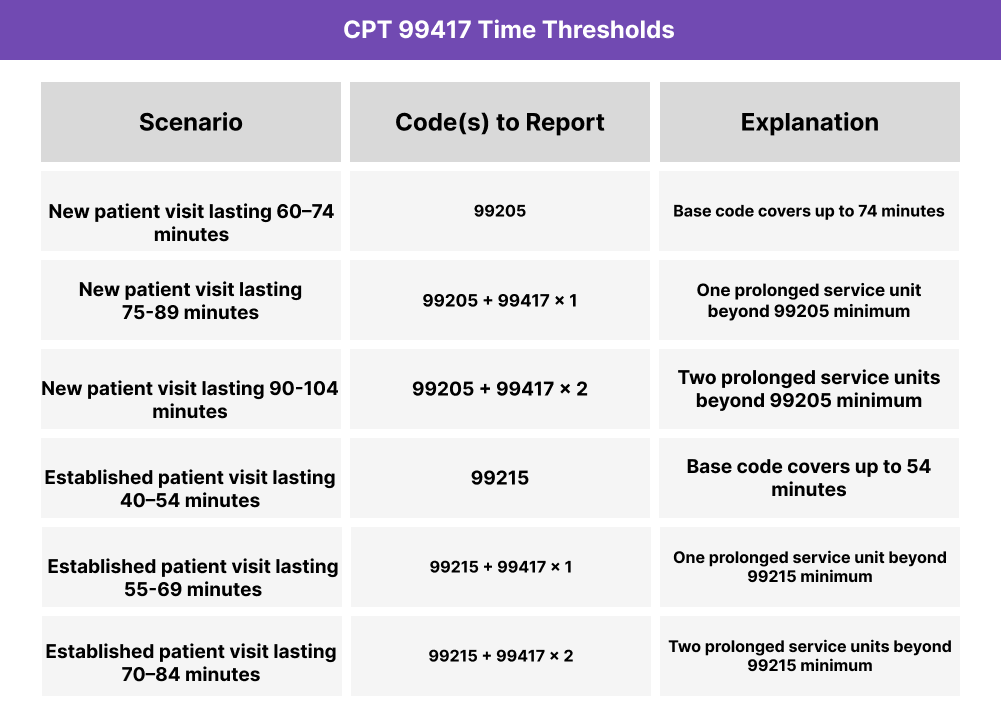
CPT 99417 Time Thresholds and Code Combinations
CPT 99417 is billed for every 15 minutes of prolonged outpatient service beyond the required time for the highest-level primary E/M code. It can only be reported after the base threshold for 99205 (new patient) or 99215 (established patient) has been met and exceeded.
Important to Note:
- Each unit of 99417 requires a full 15 minutes of additional time.
- Time may include both direct (face-to-face) and indirect (non–face-to-face) provider activities performed on the date of the encounter.
- Do not report 99417 for any time less than 15 minutes.
When to Use CPT 99417: Common Scenarios and Use Cases
CPT 99417 is appropriate when a physician, nurse practitioner (NP), or physician assistant (PA) provides prolonged outpatient evaluation and management (E/M) services that extend at least 15 minutes beyond the highest-level primary service (99205 or 99215).
Here are examples of how CPT 99417 is used in practice:
CPT 99417 Billing Requirements and Eligibility
CPT 99417 is reported when a provider delivers prolonged outpatient E/M services that extend beyond the time required for the highest-level new or established patient code. It is billed in 15-minute increments once the base threshold has been exceeded.
Patient Eligibility
- Must be seen in an office or outpatient setting (including approved telehealth encounters).
- Can apply to new patients (99205) or established patients (99215).
- Prolonged time must represent direct and indirect provider activities performed on the same date of service.
Provider Requirements
- Only a physician, nurse practitioner (NP), or physician assistant (PA) may bill this code.
- Provider must personally spend the prolonged time; staff or ancillary time does not count.
- Documentation must clearly link additional time to the same E/M encounter.
Service Requirements
May only be billed after meeting the threshold for the highest-level code:
- 99205: prolonged billing begins at 75 minutes
- 99215: prolonged billing begins at 55 minutes
- Each additional 15 minutes = 1 unit of 99417.
- Must not overlap with separately reported prolonged services (e.g., 99358, 99359, 99415, 99416).
- Not valid for inpatient or ED encounters — 99418 applies in those settings.
Comparison With Related Codes
- 99417 vs 99205/99215: 99417 is never standalone; it is only used in addition to the base code when time exceeds the minimum by 15 minutes.
- 99417 vs 99418: 99417 is for outpatient settings, while 99418 applies to inpatient and observation care.
- 99417 vs 99358/99359: 99417 is used when prolonged services occur on the same date as the encounter; 99358/99359 apply to prolonged services on different dates.
CPT 99417 Billing Documentation Checklist
To support compliant billing for CPT 99417, records should include:
- Primary E/M code documented (99205 or 99215) showing the base threshold was met
- Clear record of prolonged time, specifying:
- Total encounter duration (face-to-face + non–face-to-face)
- Activities performed during the additional 15+ minutes (e.g., chart review, counseling, coordination, documentation)
- Incremental time logs showing each full 15-minute unit of prolonged service achieved
- Provider attestation confirming the time was personally spent by a physician, NP, or PA
- Documentation of patient status (new or established) to support the correct primary code pairing
- Confirmation that prolonged services occurred on the same date of service as the primary E/M encounter
- Statement excluding overlapping time with other prolonged service codes (99358, 99359, 99415, 99416)
- Supporting notes for care complexity, demonstrating why prolonged time was required (e.g., multiple conditions, extensive counseling, care coordination)
Common CPT 99417 Billing Mistakes (and How to Avoid Them)
❌ Reporting 99417 Without a Primary E/M Code
This is an add-on code only. It must be billed with a qualifying primary code (99205 or 99215).
❌ Billing Before the Threshold is Met
Prolonged services can’t be reported until the encounter extends 15 minutes beyond the base code (75 minutes for 99205, 55 minutes for 99215).
❌ Counting Non-Provider Time
Only time personally spent by a physician, NP, or PA qualifies. Staff, nursing, or administrative time cannot be included.
❌ Rounding Up Time
Documentation must show a full 15-minute increment. Partial time units (e.g., 10 minutes) may not be billed.
❌ Using 99417 in the Wrong Setting
This code applies only to outpatient and office visits. Inpatient or observation encounters require CPT 99418.
❌ Overlapping With Other Prolonged Service Codes
99417 cannot be reported with 99358, 99359, 99415, or 99416 for the same date of service.



