What is CCDT (Care Coordination Data Template) in Healthcare?
The Care Coordination Data Template (CCDT) is a standardized framework developed to support the exchange of care coordination information across providers, payers, and health IT systems. It defines the core data elements needed to capture and share patient information related to care management, transitions of care, and population health programs.
In practice, CCDT helps providers ensure that essential care coordination data — such as medications, diagnoses, Social Determinants of Health (SDOH), and care team contacts — is consistently documented and transmitted. By providing a structured template, CCDT supports interoperability, clinical communication, and CMS reporting requirements.
For billing and compliance teams, CCDT has an indirect impact: while it does not generate claims, it ensures that the data needed for Value-Based Care (VBC) reporting, quality metrics, and care management programs is accurately captured and exchanged.
Key Components of the Care Coordination Data Template (CCDT)
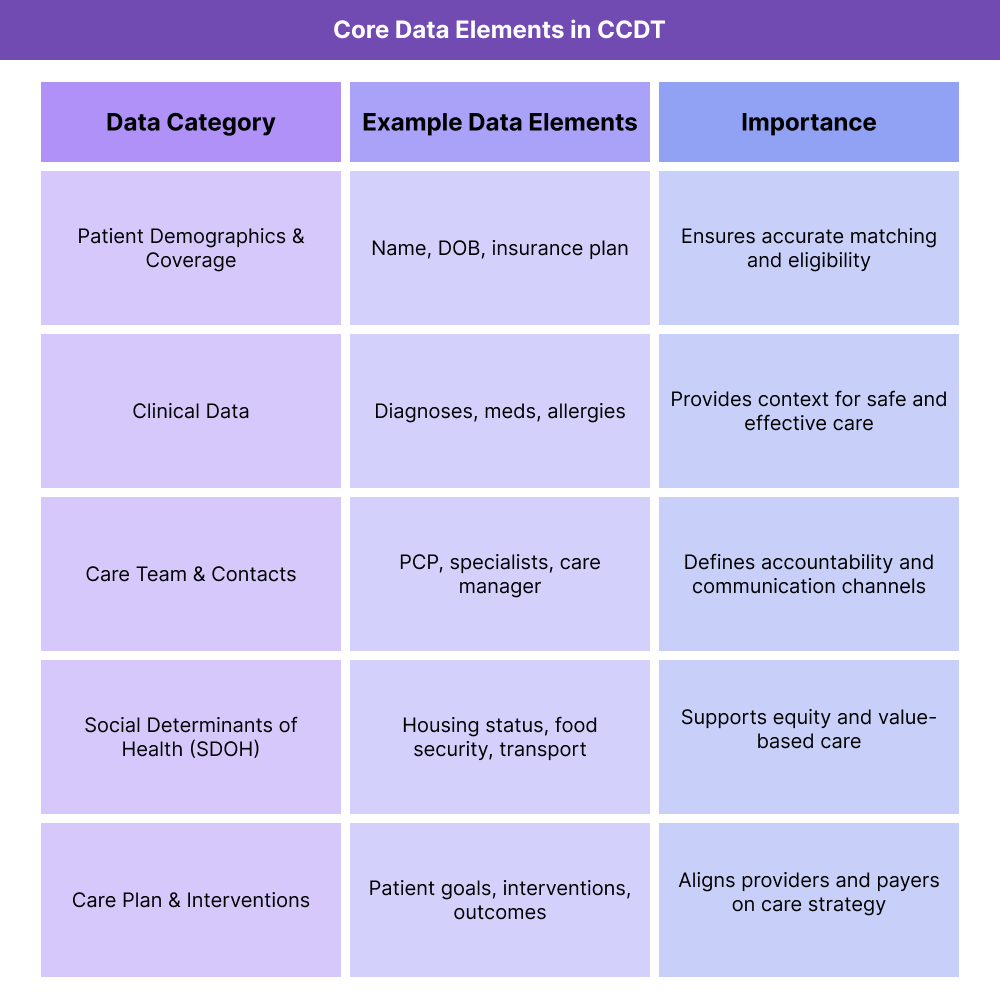
The Care Coordination Data Template (CCDT) was designed to ensure that the most critical elements of patient information are consistently captured and shared between healthcare organizations. By defining what data must be included, CCDT improves care continuity, population health tracking, and CMS reporting compliance.
For providers and payers, the CCDT offers a common data framework that bridges gaps between disparate EHR systems, helping teams communicate patient needs more effectively during transitions of care.
Patient Demographics and Coverage
- Basic patient identifiers such as name, date of birth, address, and insurance coverage.
- Ensures accurate patient matching and reduces duplicate records.
Clinical Data
- Diagnoses, medications, allergies, and problem lists.
- Provides clinicians with the essential clinical context needed for safe and effective care.
Care Team and Contacts
- Lists care managers, primary care physicians, specialists, and support staff involved in the patient’s care.
- Clarifies roles and responsibilities in multi-provider environments.
Social Determinants of Health (SDOH)
- Includes non-clinical factors such as housing status, food insecurity, or transportation access.
- Supports value-based care programs by addressing equity and outcomes.
Care Plan and Interventions
- Summarizes patient goals, interventions, and progress tracking.
- Aligns providers and payers on care strategies and outcomes measurement.
How CCDT Is Used in Healthcare Workflows
The Care Coordination Data Template (CCDT) is designed to make care transitions and ongoing management more consistent across providers, payers, and care teams. It ensures that essential information flows seamlessly, reducing gaps and improving outcomes.
Step 1: Patient Registration and Intake
- Demographics, coverage details, and basic medical history are collected in the CCDT structure.
- This ensures patient data can be matched and shared accurately with downstream systems.
Step 2: Care Planning and Coordination
- Providers and care managers document diagnoses, medications, allergies, and patient goals within the template.
- Care team roles (e.g., primary care physician, specialist, social worker) are assigned for accountability.
Step 3: Communication Across Settings
- When a patient transitions from hospital to outpatient care, CCDT ensures consistent information is passed along.
- CCDT data supports interoperability standards like HL7, CDA, and FHIR, making it usable across different EHRs.
Step 4: Tracking Interventions and Outcomes
- Providers log care plan updates, interventions, and progress in the template.
- Care coordination activities — such as follow-up calls or medication reconciliations — are documented for visibility.
Step 5: Reporting for Compliance and Value-Based Care
- CCDT data feeds into CMS reporting requirements, quality programs, and population health initiatives.
- Standardized CCDT fields allow organizations to measure SDOH factors, care plan adherence, and outcome metrics.
CCDT in Billing, Reimbursement, and Compliance Limitations
The Care Coordination Data Template (CCDT) is not a billing tool in itself, but it plays an indirect yet critical role in how providers and payers manage reimbursement, particularly under Value-Based Care (VBC) and CMS reporting requirements. By ensuring that key data elements are consistently captured and shared, CCDT helps organizations meet compliance standards and demonstrate performance on quality measures.
Indirect Role in Reimbursement
- CCDT does not generate CPT or HCPCS codes, but it provides the supporting data needed for claims accuracy.
- Documentation of diagnoses, interventions, and SDOH factors feeds into risk adjustment models such as HCC and RAF scoring.
- Proper CCDT use supports quality reporting tied to reimbursement in Medicare and Medicaid programs.
Compliance and Reporting Benefits
- CCDT ensures that required data elements for care management programs are structured and available for reporting.
- Supports CMS initiatives such as Chronic Care Management (CCM), Transitional Care Management (TCM), and Population Health reporting.
- Provides an auditable trail of care coordination, reducing compliance risk during CMS or payer reviews.
Limitations and Adoption Challenges
- Not Universal: CCDT is not as widely implemented as HL7 CDA or FHIR, limiting interoperability in some settings.
- Workflow Burden: Smaller practices may find CCDT adoption resource-intensive, requiring workflow redesign.
- Data Overlap: Providers may see redundancy between CCDT and other templates (e.g., CCD/Continuity of Care Document), creating confusion without clear governance.
- Technology Gaps: Systems that don’t support structured data capture may not fully benefit from CCDT, requiring manual workarounds.
CCDT and Its Impact on Care Quality, Equity, and Data Integrity
The Care Coordination Data Template (CCDT) contributes directly to quality improvement, equity in care delivery, and stronger data integrity. By standardizing care coordination data, CCDT ensures that both clinical and non-clinical information flows across the continuum of care, supporting better patient outcomes and more equitable access to services.
Improving Quality of Care and Patient Safety
- CCDT ensures that diagnoses, medications, and allergies are consistently documented and shared, reducing the risk of errors during care transitions.
- Care plans and interventions logged in CCDT help multidisciplinary teams stay aligned on treatment goals.
- Standardized CCDT fields enable quality tracking across patient populations, feeding into performance dashboards and CMS quality programs.
Supporting Equity Through SDOH Capture
- CCDT includes structured fields for Social Determinants of Health (SDOH), such as housing, food security, and transportation.
- Capturing this data helps providers identify barriers to care and connect patients with community resources.
- For payers and regulators, CCDT’s inclusion of SDOH data supports equity-focused initiatives and CMS health equity reporting requirements.
Enhancing Data Integrity and Transparency
- Standardized CCDT records provide an auditable trail of care coordination activities, strengthening compliance and reducing disputes with payers.
- By integrating with interoperability standards like HL7 and FHIR, CCDT improves data consistency across EHRs and care settings.
- For providers, this transparency reduces rework and supports trust in shared data across organizations.
Challenges and Adoption Considerations
- Without full adoption, equity-focused data like SDOH may remain inconsistently documented.
- Smaller providers may struggle with the technology investment required to implement CCDT effectively.
- To maximize impact, CCDT needs alignment with broader interoperability efforts, including HL7 CDA and FHIR.
Frequently Asked Questions about CCDT
1. What is CCDT in healthcare?
CCDT stands for Care Coordination Data Template, a standardized framework for documenting and exchanging patient care coordination information across providers, payers, and health IT systems.
2. How is CCDT used in medical billing?
CCDT does not directly generate billing codes, but it ensures that the data supporting claims — such as diagnoses, interventions, and care plans — is consistently captured. This improves compliance and supports value-based reimbursement programs.
3. How is CCDT different from CCD (Continuity of Care Document)?
- CCDT: Focused on standardized care coordination data elements, including SDOH and care plan details.
- CCD: A clinical summary document used during transitions of care, standardized under HL7 CDA.
They complement each other but serve different purposes.
4. What data is included in CCDT?
Typical CCDT elements include patient demographics, coverage, diagnoses, medications, allergies, care team members, SDOH factors, and care plan goals.
5. How does CCDT support CMS reporting?
CCDT provides structured data for programs like Chronic Care Management (CCM), Transitional Care Management (TCM), and other population health initiatives. It also supports Medicare quality reporting and health equity mandates.
6. What are the benefits of CCDT for providers?
- Improves care transitions by ensuring consistent handoffs.
- Reduces errors through standardized documentation.
- Strengthens compliance and reporting readiness.
- Supports value-based care by capturing interventions and outcomes.
7. What challenges exist in implementing CCDT?
Barriers include limited adoption compared to HL7 standards, technology gaps in smaller practices, and potential overlap with other templates. Successful use requires EHR support and staff training.
