What are Z Codes?
Z codes are a category within the ICD-10-CM medical coding system used to capture factors that influence a patient’s health but are not classified as diseases or injuries. They are especially important for documenting social determinants of health (SDOH) such as housing instability, food insecurity, or lack of transportation. The “Z” does not stand for a specific word — it is simply the ICD-10 chapter designation (Z00–Z99) for codes that reflect health status factors and reasons for healthcare encounters.
In value-based care models, Z codes help providers and payers better understand patient risk, support care coordination, and identify populations with unmet social needs. While Z codes generally do not affect reimbursement directly, they provide critical data that informs quality reporting, care management programs like Chronic Care Management (CCM), and risk adjustment methodologies such as Hierarchical Condition Categories (HCC).
By standardizing documentation of non-clinical factors, Z codes strengthen connections between value-based care (VBC) goals and real-world patient needs, supporting equity-focused initiatives across CMS programs.
Key Components of Z Codes
Definition & Scope
- Found in the ICD-10-CM coding system, under chapter Z00–Z99
- Capture reasons for healthcare encounters and factors affecting health status
- Include both clinical context codes (e.g., follow-ups, screenings) and social determinants of health (SDOH) codes
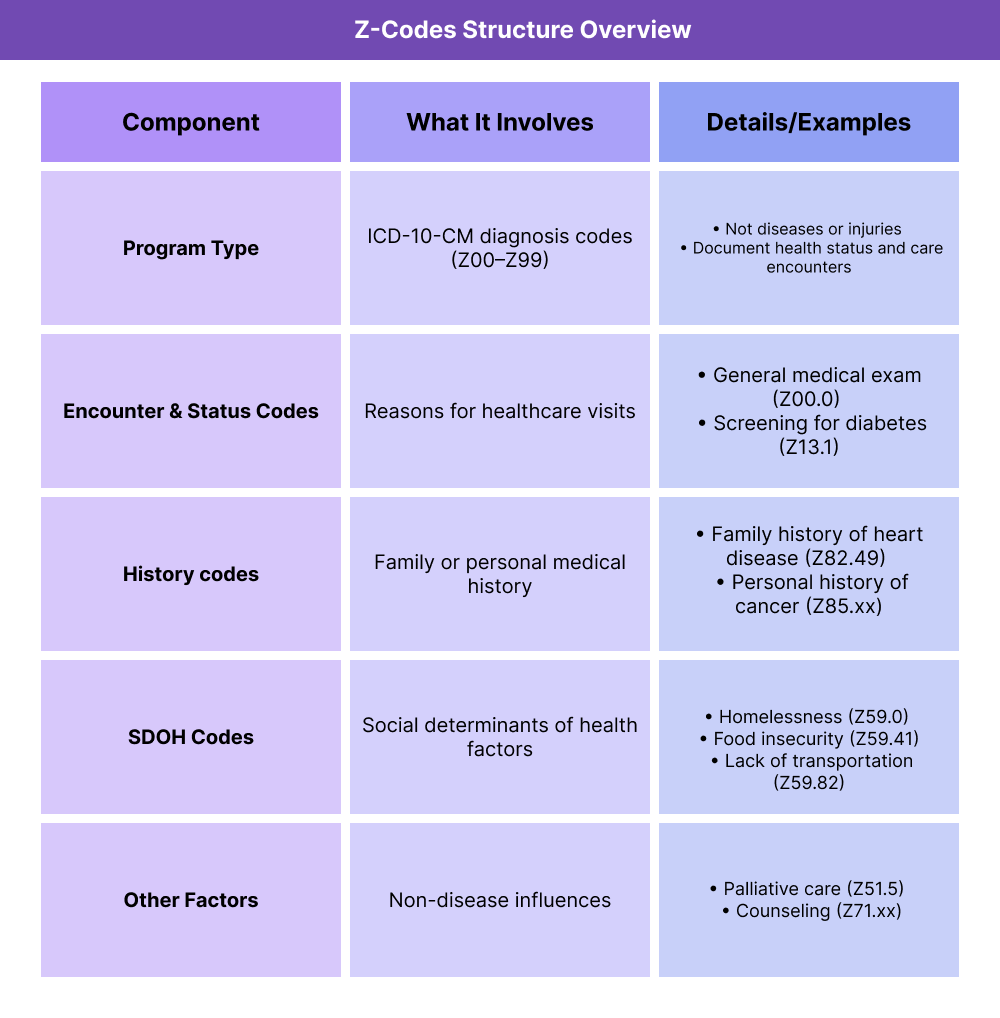
Types of Z Codes
- Encounter & Status Codes: Document reasons for visits (e.g., general check-ups, screenings, aftercare)
- History Codes: Capture family or personal history of conditions (e.g., cancer history, prior procedures)
- Social Determinants of Health Codes: Document non-clinical factors like housing, food, employment, and education
- Other Factors: Such as palliative care, counseling, or other influences not tied to a disease
Use in Billing & Reporting
How Z Codes Are Used in Practice
Step 1 — Patient Encounter Occurs
A patient comes in for care — this could be a routine check-up, management of a chronic condition, or a visit where social needs are identified.
Step 2 — Provider Identifies a Relevant Non-Disease Factor
The clinician documents either:
- A reason for the visit (e.g., routine screening, follow-up exam)
- A patient’s history of illness or procedure
- A social determinant of health (SDOH) factor like food insecurity, housing, or transportation issues
Step 3 — Z Code is Assigned
The provider or coder selects the appropriate Z code from ICD-10-CM.
- Example: Z59.0 = homelessness
- Example: Z85.3 = personal history of breast cancer
- Example: Z00.00 = general adult medical exam
Step 4 — Claim Submission & Reporting
The Z code is included as a secondary diagnosis code on the claim.
- It typically does not affect reimbursement directly
- It adds contextual data for population health analytics, equity tracking, and quality reporting
Step 5 — Data Utilization
Payers, health systems, and CMS use Z code data to:
Billing and Reimbursement for Z Codes
How Z Codes Appear in Claims
- Z codes are submitted as ICD-10-CM diagnosis codes on medical claims.
- They are generally listed as secondary codes to provide context alongside the primary medical diagnosis.
- Example: A patient visit for diabetes management (E11.9) may also include Z59.41 (food insecurity).
Do Z Codes Affect Reimbursement?
- No direct payment: Z codes do not currently drive reimbursement by themselves.
- Indirect impact: They support quality reporting, risk adjustment, and population health management — all of which influence funding in value-based care (VBC) programs.
- CMS emphasis: Models like ACO REACH and VBID encourage Z code reporting to strengthen health equity initiatives.
Limitations of Z Codes in Billing
- Underutilization: Many providers do not consistently document Z codes, leaving social risk factors invisible in claims data.
- Variation: Coding practices vary across organizations, leading to inconsistent data capture.
- Non-mandatory: CMS strongly encourages use of Z codes but does not require them in all payment models.
Future Outlook
- Increased emphasis: CMS has signaled that Z code reporting may become more central to risk adjustment and quality reporting in the future.
- Integration: As equity and social determinants of health gain policy focus, Z codes are expected to play a bigger role in linking payment models with patient needs.
Quality & Equity Implications of Z Codes
Z Codes’ Role in Addressing Social Determinants of Health (SDOH)
Z codes allow providers to systematically document patient needs that affect health outcomes but fall outside traditional clinical diagnoses.
- Housing instability, food insecurity, lack of transportation
- Financial hardship or difficulty accessing medication
- Social support and caregiving challenges
Why Z Codes Matter for Equity
- Provide standardized data to identify disparities in care access and outcomes
- Help practices design targeted interventions for vulnerable populations
- Support CMS’s equity initiatives in models like ACO REACH, which requires an equity plan, and VBID, which tests benefit designs for high-need groups
Z Codes’ Impact on Quality Reporting
- Enhance risk adjustment by flagging social and environmental factors
- Improve accuracy of quality measures by showing context behind outcomes
- Feed into care management programs, including Chronic Care Management (CCM), where social needs often complicate chronic disease control
Challenges with Z Code Use
- Low adoption: Many providers underutilize Z codes due to workflow and documentation burdens
- Data gaps: Without consistent reporting, social risks remain invisible in population health strategies
- Future potential: CMS and payers may increasingly incentivize or require Z code documentation to strengthen quality and equity tracking
Frequently Asked Questions about Z Codes
1. What are Z codes in healthcare?
Z codes are part of the ICD-10-CM coding system, used to document factors that influence a patient’s health but are not diseases or injuries. They include reasons for encounters, medical history, and social determinants of health (SDOH).
2. How are Z codes used in medical billing?
Z codes are added as secondary diagnosis codes on claims to provide context. While they do not directly affect reimbursement, they support risk adjustment, quality reporting, and value-based care initiatives.
3. Are Z codes required for reimbursement?
No, Z codes are not required for payment. However, CMS strongly encourages their use because they capture important patient context that can shape quality metrics and population health strategies.
4. What is an example of a Z code?
Examples include Z00.00 (general adult medical exam), Z85.3 (personal history of breast cancer), and Z59.41 (food insecurity).
5. Are Z codes the same as SDOH codes?
Not exactly. SDOH codes are a subset of Z codes (Z55–Z65 and related categories) that specifically capture social and environmental factors like housing, food, and employment.
6. How do Z codes support value-based care (VBC)?
Z codes provide data that helps identify at-risk populations, track disparities, and design equity-focused interventions. They also enhance care coordination programs such as Chronic Care Management (CCM) and support equity requirements in models like ACO REACH and VBID.
