What is ACO REACH (Accountable Care Organization Realizing Equity, Access, and Community Health)?
ACO REACH (Accountable Care Organization Realizing Equity, Access, and Community Health) is a value-based care model from the Centers for Medicare & Medicaid Services (CMS) that began in 2023. It was created to replace the Direct Contracting Model (DCM) after concerns about transparency and equity, and it requires Accountable Care Organizations (ACOs) and other participants to take on financial risk while advancing health equity. ACO REACH is part of CMS’s broader effort to move Medicare away from fee-for-service and toward value-based care (VBC) and accountable, population-based care.
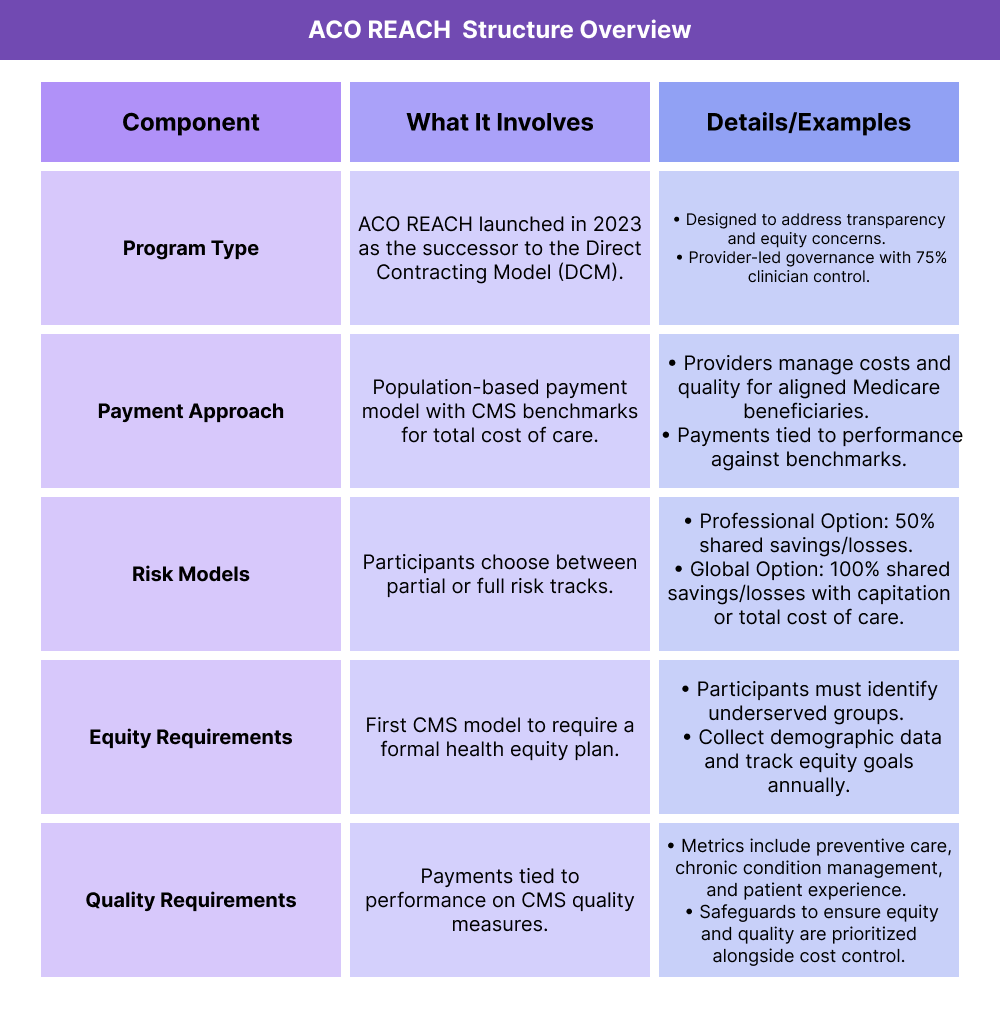
Key Components of ACO REACH
How Does ACO REACH Work?
ACO REACH organizations agree to manage the cost and quality of care for a defined group of Medicare beneficiaries. CMS establishes spending benchmarks, and participants are accountable for meeting both financial and quality performance standards.
What Risk Arrangements Are Available?
Participants can choose between two risk tracks:
- Professional Option (Partial Risk): 50% shared savings and losses on total cost of care.
- Global Option (Full Risk): 100% shared savings and losses, with either capitation or total cost of care payments.
How Does Equity Fit Into the Model?
ACO REACH is the first CMS model to require a health equity plan. Participants must collect demographic and social needs data, develop measurable equity goals, and report progress annually.
What Governance Rules Apply?
At least 75% of the ACO REACH governing board must be made up of participating providers. This ensures the model is provider-led and accountable to clinicians, not just investors.
What Quality Measures Are Used?
Performance is tied to established CMS quality metrics, including preventive care, chronic condition management, patient experience, and health outcomes. These safeguards ensure the model improves care while reducing costs.
How the ACO REACH Model Works in Practice
The ACO REACH program establishes a process for aligning beneficiaries, defining accountability, and reconciling performance against CMS benchmarks.
Step 1 — Participant Organizations Apply
Eligible entities include provider-led Accountable Care Organizations, health systems, physician groups, and other risk-bearing organizations. Each must demonstrate the ability to manage population health and comply with CMS requirements.
Step 2 — Beneficiaries Are Aligned
Medicare fee-for-service beneficiaries are attributed to ACO REACH participants through voluntary alignment (patients choosing a provider) or claims-based alignment (based on where they typically receive care).
Step 3 — Benchmarks and Risk Tracks Established
CMS sets spending benchmarks for the ACO REACH population. Participants select either the Professional (50% risk) or Global (100% risk) track.
Step 4 — Care Delivery and Equity Plans Implemented
Participants manage care across the continuum, with required health equity plans to identify underserved groups, collect demographic data, and report annual progress.
Step 5 — Performance Measurement and Reconciliation
CMS evaluates total spending against benchmarks and ties results to quality and equity measures. Organizations share in savings if goals are met — or may owe CMS repayments under downside risk.
Payment & Risk Structure (Billing and Reimbursement) in ACO REACH
How Payments Are Structured in ACO REACH
ACO REACH participants are reimbursed through a population-based payment system rather than traditional fee-for-service billing. CMS sets a benchmark for each organization’s attributed beneficiaries, and actual spending is compared against that benchmark at the end of the year.
- Benchmarks are based on historical Medicare spending data, adjusted for risk and regional factors.
- Payments function as prospective or retrospective reimbursement depending on the track selected.
- Savings or losses are reconciled annually through CMS billing and settlement.
Risk Options for Participants
ACO REACH offers two tracks that define billing flows and financial accountability:
Professional Option (Partial Risk):
- 50% shared savings and 50% shared losses on total cost of care.
- Monthly primary care capitation payments available for reimbursement.
Global Option (Full Risk):
- 100% shared savings and 100% shared losses.
- Two reimbursement pathways: Total Care Capitation (per-beneficiary payments) or Total Cost of Care (benchmark vs actual spending).
How Savings and Losses Are Reconciled in ACO REACH
- If actual spending is below the benchmark and quality/equity requirements are met → participants share in savings.
- If actual spending is above the benchmark → participants must repay CMS under their chosen billing and risk arrangement.
Quality & Equity Requirements in ACO REACH
Quality Measures
ACO REACH ties financial performance directly to quality outcomes. Participants are evaluated on CMS quality metrics that focus on preventive care, chronic disease management, patient experience, and overall health outcomes.
- Preventive services (e.g., screenings, vaccinations)
- Chronic condition management (e.g., diabetes, hypertension)
- Patient experience surveys (CAHPS)
- Avoidable hospitalizations and readmissions
Equity Requirements
ACO REACH is the first CMS model to formally require participants to address health equity. Each participating organization must:
- Develop a Health Equity Plan outlining how it will identify and reduce disparities.
- Collect demographic and social needs data on attributed beneficiaries.
- Set measurable goals for improving access and outcomes among underserved groups.
- Submit annual progress reports to CMS for review and accountability.
Safeguards for Beneficiaries
To ensure quality and equity are not compromised in pursuit of savings, CMS requires:
- Transparent reporting of performance data.
- Patient protections around access to care and freedom of choice.
- Oversight mechanisms to prevent underutilization or inequitable care delivery.
Frequently Asked Questions about ACO REACH
1. What is ACO REACH?
ACO REACH (Accountable Care Organization Realizing Equity, Access, and Community Health) is a CMS value-based care model launched in 2023. It replaced the Direct Contracting Model (DCM) to strengthen transparency, accountability, and health equity.
2. Who can participate in ACO REACH?
Eligible participants include provider-led ACOs, physician groups, health systems, and other risk-bearing entities that can manage population health and comply with CMS’s equity and quality requirements.
3. What happened to the Direct Contracting Model (DCM)?
The Direct Contracting Model was retired due to concerns about transparency and equity. ACO REACH is its successor, designed to address those concerns while keeping population-based payment models in place.
4. Is ACO REACH considered an Advanced APM?
Yes. ACO REACH qualifies as an Advanced Alternative Payment Model (APM) under the Quality Payment Program (QPP). Participants may be eligible for QPP incentives if requirements are met.
5. How does ACO REACH differ from MSSP ACOs?
MSSP ACOs are primarily shared savings programs, while ACO REACH involves higher levels of risk and requires formal health equity plans. ACO REACH also offers capitation options that MSSP does not.
6. What are the equity requirements in ACO REACH?
Participants must create and implement a Health Equity Plan, collect demographic and social needs data, and report annually to CMS on equity goals and outcomes.
