What is BPCI (Bundled Payments for Care Improvement)?
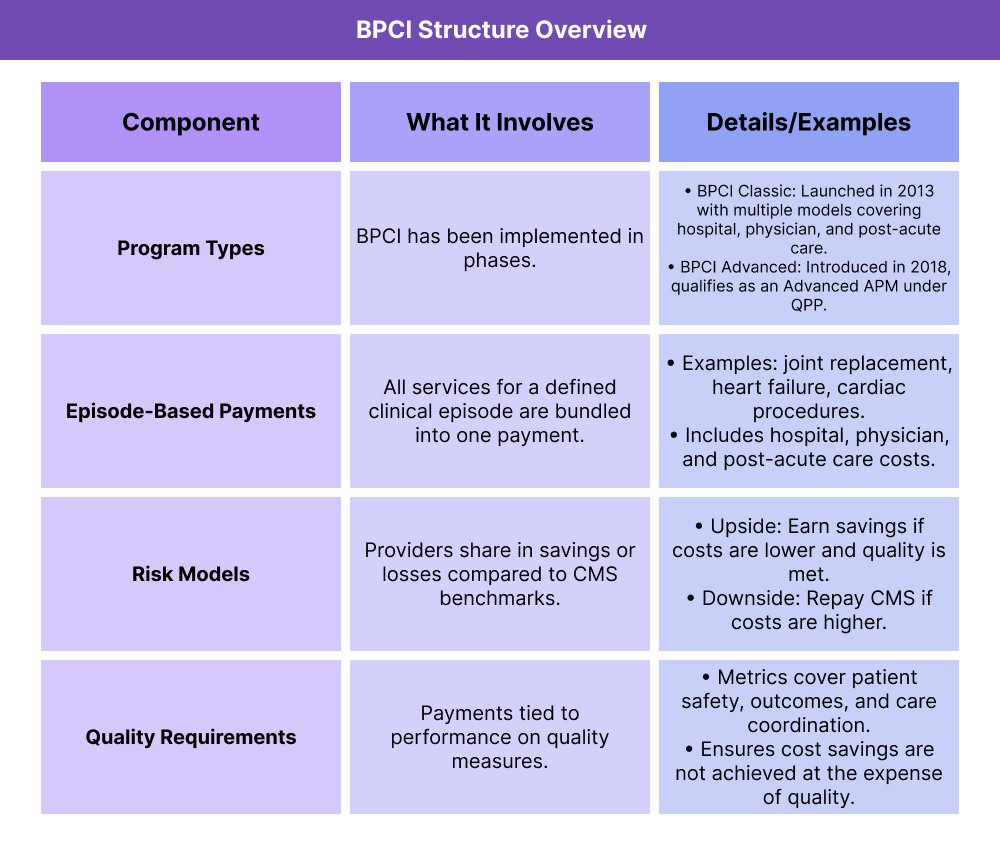
BPCI was a payment model developed by the Centers for Medicare & Medicaid Services (CMS) to encourage more coordinated, cost-efficient care. Instead of paying providers separately for each service delivered during a treatment episode, BPCI bundled all related services into a single payment amount.
Under BPCI, hospitals, physician groups, and post-acute care providers shared accountability for the total cost and quality of care during a defined episode, such as a joint replacement or cardiac procedure. If providers delivered care for less than the bundled amount while meeting quality standards, they shared in the savings. If costs exceeded the target, they were responsible for some or all of the losses.
BPCI was a key example of an Alternative Payment Model (APM) under Medicare’s broader shift to value-based care (VBC). The program ran through multiple phases, most notably BPCI Classic and BPCI Advanced, before concluding in 2023.
Key Components of BPCI
The Bundled Payments for Care Improvement (BPCI) initiative was structured around defined episodes of care, with participating providers taking accountability for cost and quality across an entire episode. CMS offered multiple versions of the program, most notably BPCI Classic and BPCI Advanced, before the initiative ended in 2023.
How Episode-Based Payments Worked in BPCI
Instead of separate payments for each service, CMS set a target price for the entire episode of care. Providers were incentivized to coordinate care across hospitals, physicians, and post-acute facilities to stay within the budget.
How Risk Sharing Worked in BPCI
Participants could earn shared savings if they kept costs below benchmarks while meeting quality standards. In downside-risk arrangements, they were required to repay CMS if costs exceeded benchmarks.
What Quality Measures Were Used in BPCI
To safeguard patients, CMS tied bundled payments to quality metrics such as safety indicators, readmission rates, and care coordination outcomes. This helped ensure BPCI promoted better outcomes instead of just lower costs.
How the Bundled Payments for Care Improvement Model Worked in Practice
The BPCI program followed a structured workflow that begins with a defined patient episode and ends with reconciliation of costs and quality performance against CMS benchmarks.
Step 1 — Patient Episode Defined
A patient received treatment for a clinical condition, such as a joint replacement or cardiac procedure. CMS defined the episode of care, including all related services during a set time frame.
Step 2 — Bundled Payment Target Set
CMS established a target price for the entire episode, covering hospital, physician, and post-acute services. The target was based on historical cost and utilization data.
Step 3 — Care Delivered and Coordinated
Providers across settings (hospital, physician group, rehabilitation facility, etc.) delivered care with a focus on efficiency and coordination to stay within the budget while maintaining quality.
Step 4 — Costs and Quality Measured
CMS evaluated actual spending against the target price and reviews quality measures to confirm outcomes were not compromised.
Step 5 — Reconciliation of Payments
If costs were below the target and quality standards were met → providers shared in the savings.
If costs were above the target → providers may have owed CMS a repayment under the risk-sharing model.
BPCI and its Impact on Billing and Reimbursement
The Bundled Payments for Care Improvement (BPCI) initiative changed how providers are reimbursed by moving away from fee-for-service and toward episode-based payments. This approach directly impacted billing cycles, claims submission, and provider incentives.
From Fee-for-Service to Bundled Payments
- In traditional fee-for-service, each service — hospital stay, physician visit, lab test, rehabilitation — generated a separate claim.
- Under BPCI, all services for a defined episode were grouped into a single bundled payment amount.
Claims Processing in BPCI
- Claims were still submitted by individual providers, but CMS reconciled them against the target price for the episode.
- The total cost was calculated across all providers involved, not just one entity.
Reconciliation and Payment Adjustments
- If total costs were below the target price and quality standards were met → providers share in the savings.
- If costs exceeded the target price → providers may have been required to repay CMS for the difference.
Quality as a Condition of Payment
Bundled payments were tied to quality performance measures. Providers could not earn savings unless patient outcomes met CMS standards for safety, care coordination, and effectiveness.
Why BPCI Mattered in Billing and Reimbursement
BPCI demonstrated the federal shift toward value-based care, where payment depends on cost efficiency and quality outcomes instead of service volume. For providers, this meant billing was no longer just about coding individual encounters but about coordinating care across the full episode to maximize value.
Frequently Asked Questions about BPCI
1. What was BPCI in healthcare?
BPCI (Bundled Payments for Care Improvement) was a CMS payment initiative that grouped all services for a defined episode of care into a single payment. Providers shared in savings or losses depending on whether costs stay below or exceed CMS benchmarks.
2. What was BPCI Advanced?
BPCI Advanced was the updated version of the program launched in 2018. It qualified as an Advanced Alternative Payment Model (APM) under the Quality Payment Program (QPP), meaning participants could earn a 5% Medicare incentive if criteria were met.
3. How does BPCI differ from MSSP?
Both are value-based models, but they functioned differently:
- BPCI: Focused on episodes of care (e.g., surgery + rehab + follow-up).
- MSSP: Focuses on total cost of care for a defined patient population.
Providers may participate in both, but they measure value at different levels.
4. Who could participate in BPCI?
Eligible participants included hospitals, physician group practices, post-acute care providers, and other entities that manage episodes of care. Participation required meeting CMS requirements and entering into agreements that include financial risk.
5. Is BPCI still active?
No. The original BPCI Classic ended in 2018, and BPCI Advanced concluded in 2023. While CMS continues to explore bundled payment strategies, the BPCI initiative itself is no longer active. Its lessons informed future value-based care models, including ACO REACH and other innovation programs.
